J Korean Neurosurg Soc.
2020 May;63(3):272-278. 10.3340/jkns.2020.0068.
Spinal Dysraphism in the Last Two Decades : What I Have Seen during the Era of Dynamic Advancement
- Affiliations
-
- 1Division of Pediatric Neurosurgery, Seoul National University Children’s Hospital, Seoul, Korea
- KMID: 2501715
- DOI: http://doi.org/10.3340/jkns.2020.0068
Abstract
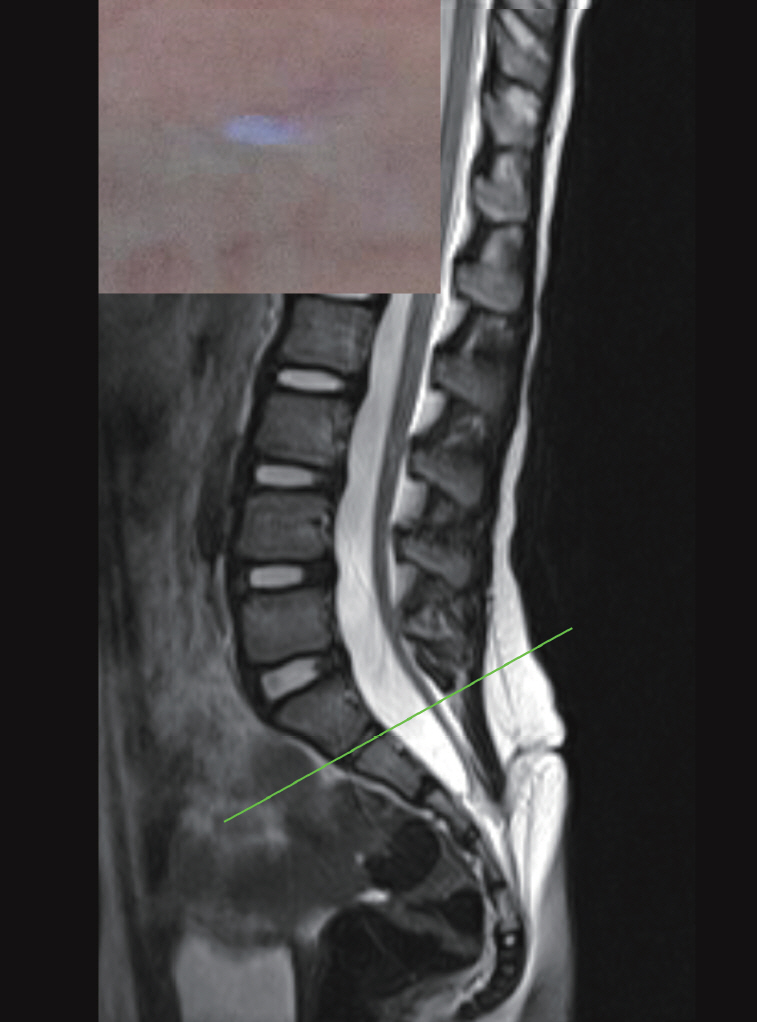
- Compared to any other decade, the last two decades have been the most dynamic period in terms of advances in the knowledge on spinal dysraphism. Among the several factors of rapid advancement, such as embryology during secondary neurulation and intraoperative neurophysiological monitoring, there is no doubt that Professor Dachling Pang stood high amidst the period. I review here the last two decades from my personal point of view on what has been achieved in the field of spinal dysraphism, focusing on occult tethered cord syndrome, lumbosacral lipomatous malformation, terminal myelocystocele, retained medullary cord, limited dorsal myeloschisis and junctional neural tube defect. There are still many issues to revise, add and extend. Profound knowledge of basic science is critical, as well as refined clinical analysis. I expect that young scholars who follow the footsteps of precedent giants will shed bright light on this topic in the future.
Figure
Cited by 1 articles
-
Disorders of Secondary Neurulation : Mainly Focused on Pathoembryogenesis
Jeyul Yang, Ji Yeoun Lee, Kyung Hyun Kim, Kyu-Chang Wang
J Korean Neurosurg Soc. 2021;64(3):386-405. doi: 10.3340/jkns.2021.0023.
Reference
-
References
1. Beardmore HE, Wiglesworth FW. Vertebral anomalies and alimentary duplications; clinical and embryological aspects. Pediatr Clin North Am. 5:457–474. 1958.
Article2. Bremer JL. Dorsal intestinal fistula; accessory neurenteric canal; diastematomyelia. AMA Arch Pathol. 54:132–138. 1952.3. Caram PC, Carton CA, Scarcella G. Intradural lipomas of the spinal cord; with particular emphasis on the intramedullary lipomas. J Neurosurg. 14:28–42. 1957.4. Chapman PH. Congenital intraspinal lipomas: anatomic considerations and surgical treatment. Childs Brain. 9:37–47. 1982.5. Dady A, Havis E, Escriou V, Catala M, Duband JL. Junctional neurulation: a unique developmental program shaping a discrete region of the spinal cord highly susceptible to neural tube defects. J Neurosci. 34:13208–13221. 2014.
Article6. Dias MS, Walker ML. The embryogenesis of complex dysraphic malformations: a disorder of gastrulation? Pediatr Neurosurg. 18:229–253. 1992.
Article7. Eibach S, Moes G, Hou YJ, Zovickian J, Pang D. Unjoined primary and secondary neural tubes: junctional neural tube defect, a new form of spinal dysraphism caused by disturbance of junctional neurulation. Childs Nerv Syst. 33:1633–1647. 2017.
Article8. Garceau GJ. The filum terminale syndrome (the cord-traction syndrome). J Bone Joint Surg Am. 35-A:711–716. 1953.9. Hoffman HJ, Hendrick EB, Humphreys RP. The tethered spinal cord: its protean manifestations, diagnosis and surgical correction. Childs Brain. 2:145–155. 1976.
Article10. Kang JK, Kim MC, Kim DS, Song JU. Effects of tethering on regional spinal cord blood flow and sensory-evoked potentials in growing cats. Childs Nerv Syst. 3:35–39. 1987.
Article11. Kim JW, Wang KC, Chong S, Kim SK, Lee JY. Limited dorsal myeloschisis: reconsideration of its embryological origin. Neurosurgery. 86:93–100. 2020.
Article12. Lee JY, Kim SP, Kim SW, Park S-H, Choi JW, Phi JH, et al. Pathoembryogenesis of terminal myelocystocele: terminal balloon in secondary neurulation of the chick embryo. Childs Nerv Syst. 29:1683–1688. 2013.
Article13. Lee JY, Park SH, Chong S, Phi JH, Kim SK, Cho BK, et al. Congenital dermal sinus and limited dorsal myeloschisis: “spectrum disorders” of incomplete dysjuction between cutaneous and neural ectoderms. Neurosurgery. 84:428–434. 2019.
Article14. Li YC, Shin SH, Cho BK, Lee MS, Lee YJ, Hong SK, et al. Pathogenesis of lumbosacral lipoma: a test of the “premature dysjunction” theory. Pediatr Neurosurg. 34:124–130. 2001.
Article15. McLone DG, Naidich TP. Spinal dysraphism : Experimental and clinical. In : Holtzman RN, Stein BM, editors. The tethered spinal cord. New York: Thieme-Stratton;1985. p. 14–28.16. McLone DG, Naidich TP. Terminal myelocystocele. Neurosurgery. 16:36–43. 1985.
Article17. Naidich TP, McLone DG, Mutluer S. A new understanding of dorsal dysraphism with lipoma (lipomyeloschisis): radiologic evaluation and surgical correction. AJR Am J Roentgenol. 140:1065–1078. 1983.
Article18. Pang D. Split cord malformation: part II: clinical syndrome. Neurosurgery. 31:481–500. 1992.19. Pang D. Sacral agenesis and caudal spinal cord malformations. Neurosurgery. 32:755–778. discussion 778-779. 1993.
Article20. Pang D, Dias MS, Ahab-Barmada M. Split cord malformation: part I: a unified theory of embryogenesis for double spinal cord malformations. Neurosurgery. 31:451–480. 1992.21. Pang D, Zovickian J, Lee JY, Moes GS, Wang KC. Terminal myelocystocele: surgical observations and theory of embryogenesis. Neurosurgery. 70:1383–1404. discussion 1404-1405. 2012.22. Pang D, Zovickian J, Moes GS. Retained medullary cord in humans: late arrest of secondary neurulation. Neurosurgery. 68:1500–1519. discussion 1519. 2011.
Article23. Pang D, Zovickian J, Oviedo A. Long-term outcome of total and near-total resection of spinal cord lipomas and radical reconstruction of the neural placode: part I-surgical technique. Neurosurgery. 65:511–528. discussion 528-529. 2009.24. Pang D, Zovickian J, Oviedo A. Long-term outcome of total and near-total resection of spinal cord lipomas and radical reconstruction of the neural placode, part II: outcome analysis and preoperative profiling. Neurosurgery. 66:253–272. discussion 272-273. 2010.25. Pang D, Zovickian J, Oviedo A, Moes GS. Limited dorsal myeloschisis: a distinctive clinicopathological entity. Neurosurgery. 67:1555–1579. discussion 1579-1580. 2010.
Article26. Pierre-Kahn A, Zerah M, Renier D, Cinalli G, Sainte-Rose C, LellouchTubiana A, et al. Congenital lumbosacral lipomas. Childs Nerv Syst. 13:298–334. discussion 335. 1997.
Article27. Selçuki M, Coşkun K. Management of tight filum terminale syndrome with special emphasis on normal level conus medullaris (NLCM). Surg Neurol. 50:318–322. discussion 322. 1998.
Article28. Wang KC, Lee JS, Kim K, Im YJ, Park K, Kim KH, et al. Do junctional neural tube defect and segmental spinal dysgenesis have the same pathoembryological background? Childs Nerv Syst. 36:241–250. 2020.
Article29. Yamada S, Zinke DE, Sanders D. Pathophysiology of “tethered cord syndrome”. J Neurosurg. 54:494–503. 1981.
Article30. Yang HJ, Lee DH, Lee YJ, Chi JG, Lee JY, Phi JH, et al. Secondary neurulation of human embryos: morphological changes and the expression of neuronal antigens. Childs Nerv Syst. 30:73–82. 2014.
Article31. Yang HJ, Wang KC, Chi JG, Lee MS, Lee YJ, Kim SK, et al. Neural differentiation of caudal cell mass (secondary neurulation) in chick embryos: Hamburger and Hamilton stages 16-45. Brain Res Dev Brain Res. 142:31–36. 2003.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intramedullary Spinal Cord Lipoma without Spinal Dysraphism
- Spinal Dysraphism and Tethered Cord Syndrome
- Spinal Intramedullary Lipoma without Dysraphism
- Spinal Ultrasonography in Newborns and Infants with Cutaneous Manifestation of Spinal Dysraphism
- Perspectives : The Role of Clinicians in Understanding Secondary Neurulation