Trends in the Incidence and Treatment of Cerebrovascular Diseases in Korea : Part I. Intracranial Aneurysm, Intracerebral Hemorrhage, and Arteriovenous Malformation
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Department of Neurosurgery, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2501693
- DOI: http://doi.org/10.3340/jkns.2018.0179
Abstract
Objective
: To analyze the incidence and treatment trends of hemorrhagic stroke (HS), according to HS subtypes, using nationwide data in Korea from January 2008 to December 2016.
Methods
: We used data from the national health-claim database provided by the National Health Insurance Service for 2008–2016 using the International Classification of Diseases. The crude incidence and age-standardized incidence of each disease associated with HS, which included intracranial aneurysm (IA), hypertensive intracerebral hemorrhage (ICH), and arteriovenous malformation (AVM), were calculated and additional analysis was conducted according to age and sex. Changes in trends in treatment methods and number of treatments were analyzed for each cerebrovascular disease using the Korean Classification of Diseases procedure codes.
Results
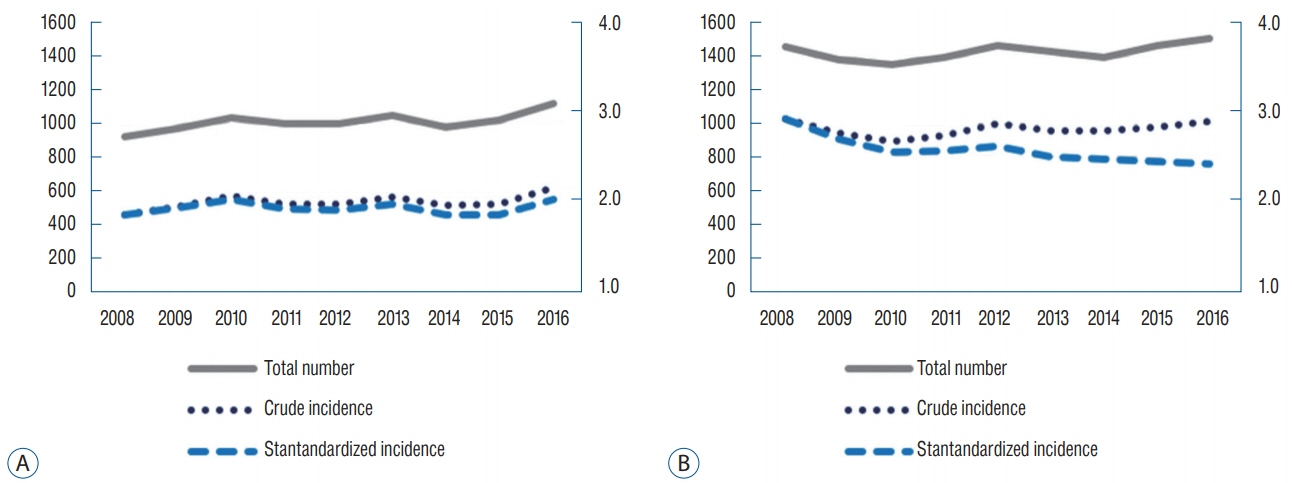
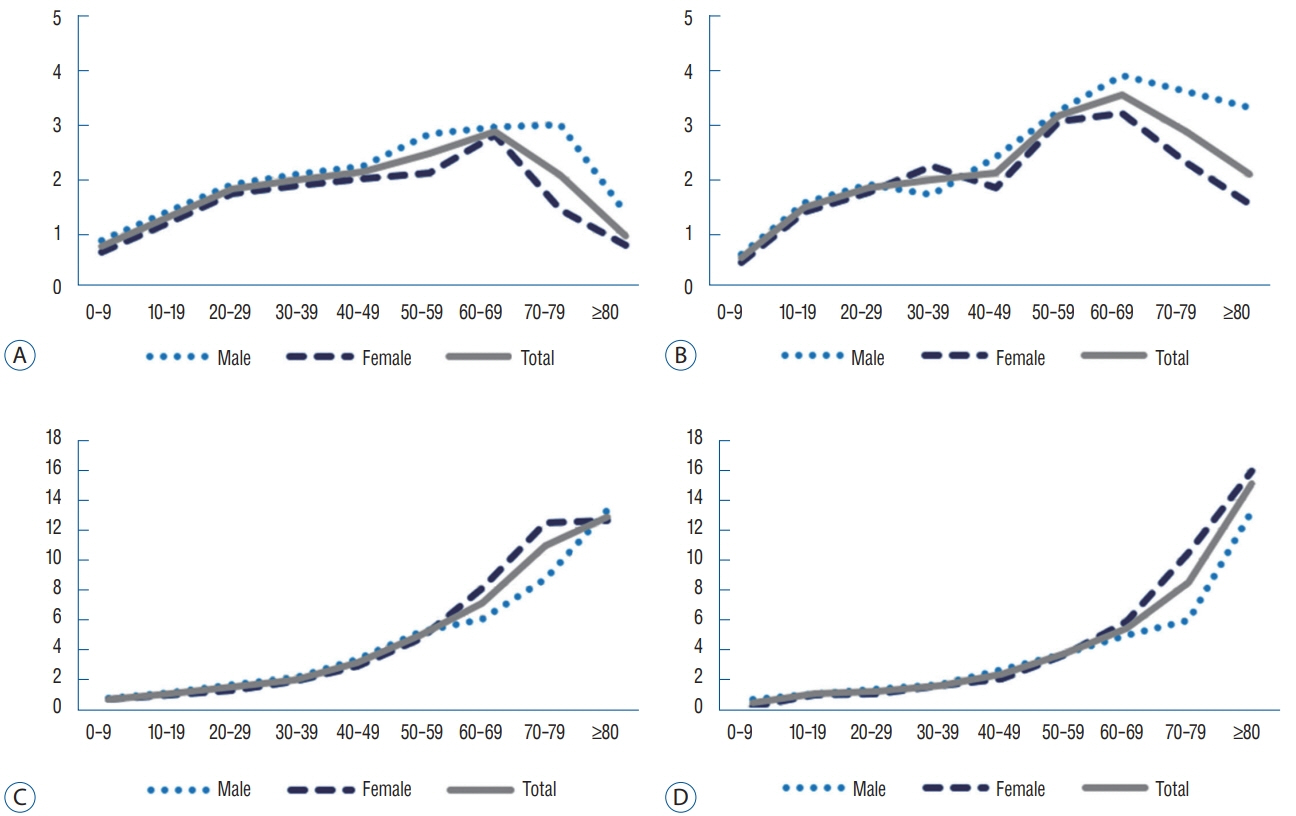
: In 2016, the total number of newly diagnosed adult patients with HS was 24169, showing a decrease by 7.0% since 2008; the age-standardized incidence of HS was 46.2 per 100000 person-years. The age-standardized incidence of unruptured IA (UIA) in adults was 71.4 per 100000 person-years—increased by 2.6-fold since 2008—while that of ruptured IA (RIA) was 12.6 per 100000 person-years, which had decreased at a rate of 20.3% since 2008. The number of coil embolization (CE) for UIA increased by 3.4-fold over 9 years and exceeded that of clipping since 2008. With respect to RIA, CE increased by 2.0-fold over 9 years and exceeded that of clipping from 2014. As for spontaneous ICH in adults, the age-standardized incidence was 31.3 per 100000 personyears in 2016—decreased by 34.7% since 2008—and 14.6% of patients diagnosed with ICH were treated in 2016, which was not significantly different from the proportion of patients treated since 2008. The age-standardized incidence of unruptured AVM (UAVM) was 2.0 per 100000 person-year in 2016, while that of ruptured AVM (RAVM) was 2.4 per 100000 person-years in 2016, showing a decreasing rate of 17.2% from 2008. The total number of treated patients with AVM declined since 2014.
Conclusion
: In Korea, age-related cerebral vascular diseases, such as RIA, ICH, and RAVM, demonstrated a declining trend in agestandardized incidence; meanwhile, UIA and UAVM demonstrated an increased trend in both crude incidence and age-standardized incidence for 9 years. The increase in the elderly population, management of hypertension, and development of diagnostic and endovascular techniques appear to have influenced this trend.
Keyword
Figure
Cited by 7 articles
-
National Trends in the Treatment of Ruptured Cerebral Aneurysms in Korea Using an Age-adjusted Method
Hye Ran Park, Jae Heon Kim, Suyeon Park, Jae-Chil Chang, Sukh Que Park
J Korean Med Sci. 2020;35(39):e323. doi: 10.3346/jkms.2020.35.e323.Intravenous Fluid Selection for Unruptured Intracranial Aneurysm Clipping : Balanced Crystalloid versus Normal Saline
Jian Kang, Young Joo Song, Sujeong Jeon, Junghwa Lee, Eunsook Lee, Ju-Yeun Lee, Euni Lee, Jae Seung Bang, Si Un Lee, Moon-Ku Han, Chang Wan Oh, Tackeun Kim
J Korean Neurosurg Soc. 2021;64(4):534-542. doi: 10.3340/jkns.2020.0262.Initial severity of aneurysmal subarachnoid hemorrhage (SAH): Trend over time
Seung Bin Sung, Young Deok Kim, Seung Pil Ban, Yong Jae Lee, O-Ki Kwon
J Cerebrovasc Endovasc Neurosurg. 2022;24(4):349-355. doi: 10.7461/jcen.2022.E2022.06.010.Self-Efficacy and Self-Care Behavior in Patients with Unruptured Intracranial Aneurysm after Treatment with Coil Embolization
Hyun Song Shin, Jeong Hye Kim
Korean J Health Promot. 2023;23(2):94-103. doi: 10.15384/kjhp.2023.23.2.94.Clinical Outcomes of Coil Embolization for Unruptured Intracranial Aneurysms Categorized by Region and Hospital Size : A Nationwide Cohort Study in Korea
Bong-Gyu Ryu, Si Un Lee, Hwan Seok Shim, Jeong-Mee Park, Yong Jae Lee, Young-Deok Kim, Tackeun Kim, Seung Pil Ban, Hyoung Soo Byoun, Jae Seung Bang, O-ki Kwon, Chang Wan Oh
J Korean Neurosurg Soc. 2023;66(6):690-702. doi: 10.3340/jkns.2023.0033.The Usefulness of Extradural Anterior Clinoidectomy for Low-Lying Posterior Communicating Artery Aneurysms : A Cadaveric Study
Hyoung Soo Byoun, Kyu-Sun Choi, Min Kyun Na, Sae Min Kwon, Yong Seok Nam
J Korean Neurosurg Soc. 2024;67(4):411-417. doi: 10.3340/jkns.2023.0184.Telemedicine Protocols for the Management of Patients with Acute Spontaneous Intracerebral Hemorrhage in Rural and Medically Underserved Areas in Gangwon State : Recommendations for Doctors with Less Expertise at Local Emergency Rooms
Hyo Sub Jun, Kuhyun Yang, Jongyeon Kim, Jin Pyeong Jeon, Sun Jeong Kim, Jun Hyong Ahn, Seung Jin Lee, Hyuk Jai Choi, In Bok Chang, Jeong Jin Park, Jong-Kook Rhim, Sung-Chul Jin, Sung Min Cho, Sung-Pil Joo, Seung Hun Sheen, Sang Hyung Lee
J Korean Neurosurg Soc. 2024;67(4):385-396. doi: 10.3340/jkns.2023.0199.
Reference
-
References
1. Adams HP Jr, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association stroke council, clinical cardiology council, cardiovascular radiology and intervention council, and the atherosclerotic peripheral vascular disease and quality of care outcomes in research interdisciplinary working groups: the American academy of neurology affirms the value of this guideline as an educational tool for neurologists. Stroke. 38:1655–1711. 2007.
Article2. Al-Shahi R, Bhattacharya JJ, Currie DG, Papanastassiou V, Ritchie V, Roberts RC, et al. Prospective, population-based detection of intracranial vascular malformations in adults: the Scottish Intracranial Vascular Malformation Study (SIVMS). Stroke. 34:1163–1169. 2003.
Article3. Berman MF, Sciacca RR, Pile-Spellman J, Stapf C, Connolly ES Jr, Mohr JP, et al. The epidemiology of brain arteriovenous malformations. Neurosurgery. 47:389–396. discussion 397. 2000.
Article4. Beslow LA, Licht DJ, Smith SE, Storm PB, Heuer GG, Zimmerman RA, et al. Predictors of outcome in childhood intracerebral hemorrhage: a prospective consecutive cohort study. Stroke. 41:313–318. 2010.
Article5. Brown RD Jr, Wiebers DO, Torner JC, O’Fallon WM. Incidence and prevalence of intracranial vascular malformations in Olmsted county, Minnesota, 1965 to 1992. Neurology. 46:949–952. 1996.
Article6. Cheng CL, Chien HC, Lee CH, Lin SJ, Yang YH. Validity of in-hospital mortality data among patients with acute myocardial infarction or stroke in National Health Insurance research database in Taiwan. Int J Cardiol. 201:96–101. 2015.
Article7. Cheng CL, Kao YH, Lin SJ, Lee CH, Lai ML. Validation of the National Health Insurance research database with ischemic stroke cases in Taiwan. Pharmacoepidemiol Drug Saf. 20:236–242. 2011.
Article8. Choi JH, Mohr JP. Brain arteriovenous malformations in adults. Lancet Neurol. 4:299–308. 2005.
Article9. Ding D, Starke RM, Kano H, Mathieu D, Huang P, Kondziolka D, et al. Radiosurgery for cerebral arteriovenous malformations in a randomized trial of unruptured brain arteriovenous malformations (ARUBA)-eligible patients: a multicenter study. Stroke. 47:342–349. 2016.
Article10. Garg K, Singh PK, Sharma BS, Chandra PS, Suri A, Singh M, et al. Pediatric intracranial aneurysms--our experience and review of literature. Childs Nerv Syst. 30:873–883. 2014.
Article11. GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 390:1151–1210. 2017.12. Hanley DF, Thompson RE, Muschelli J, Rosenblum M, McBee N, Lane K, et al. Safety and efficacy of minimally invasive surgery plus alteplase in intracerebral haemorrhage evacuation (MISTIE): a randomised, controlled, open-label, phase 2 trial. Lancet Neurol. 15:1228–1237. 2016.
Article13. Hsieh CY, Chen CH, Li CY, Lai ML. Validating the diagnosis of acute ischemic stroke in a National Health Insurance claims database. J Formos Med Assoc. 114:254–259. 2015.
Article14. Jauch EC, Saver JL, Adams HP Jr, Bruno A, Connors JJ, Demaerschalk BM, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 44:870–947. 2013.
Article15. Kim H, Sidney S, McCulloch CE, Poon KY, Singh V, Johnston SC, et al. Racial/Ethnic differences in longitudinal risk of intracranial hemorrhage in brain arteriovenous malformation patients. Stroke. 38:2430–2437. 2007.
Article16. Koton S, Schneider AL, Rosamond WD, Shahar E, Sang Y, Gottesman RF, et al. Stroke incidence and mortality trends in US communities, 1987 to 2011. JAMA. 312:259–268. 2014.
Article17. Krishnamurthi RV, Feigin VL, Forouzanfar MH, Mensah GA, Connor M, Bennett DA, et al. Global and regional burden of first-ever ischaemic and haemorrhagic stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet Glob Health. 1:e259–e281. 2013.
Article18. Laakso A, Hernesniemi J. Arteriovenous malformations: epidemiology and clinical presentation. Neurosurg Clin N Am. 23:1–6. 2012.
Article19. Lackland DT, Roccella EJ, Deutsch AF, Fornage M, George MG, Howard G, et al. Factors influencing the decline in stroke mortality: a statement from the American Heart Association/American Stroke Association. Stroke. 45:315–353. 2014.
Article20. Lee EJ, Lee HJ, Hyun MK, Choi JE, Kim JH, Lee NR, et al. Rupture rate for patients with untreated unruptured intracranial aneurysms in South Korea during 2006-2009. J Neurosurg. 117:53–59. 2012.
Article21. Lee JH, Yang DH, Park HS, Cho Y, Jun JE, Park WH, et al. Incidence of hypertension in Korea: 5-year follow-up study. J Korean Med Sci. 26:1286–1292. 2011.
Article22. Liang J, Bao Y, Zhang H, Wrede KH, Zhi X, Li M, et al. The clinical features and treatment of pediatric intracranial aneurysm. Childs Nerv Syst. 25:317–324. 2009.
Article23. Magro E, Gentric JC, Batista AL, Kotowski M, Chaalala C, Roberge D, et al. The Treatment of Brain AVMs Study (TOBAS): an all-inclusive framework to integrate clinical care and research. J Neurosurg. 128:1823–1829. 2018.
Article24. Mehrotra A, Nair AP, Das KK, Srivastava A, Sahu RN, Kumar R. Clinical and radiological profiles and outcomes in pediatric patients with intracranial aneurysms. J Neurosurg Pediatr. 10:340–346. 2012.
Article25. Mendelow AD, Gregson BA, Rowan EN, Murray GD, Gholkar A, Mitchell PM, et al. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial lobar intracerebral haematomas (STICH II): a randomised trial. Lancet. 382:397–408. 2013.
Article26. Mould WA, Carhuapoma JR, Muschelli J, Lane K, Morgan TC, McBee NA, et al. Minimally invasive surgery plus recombinant tissue-type plasminogen activator for intracerebral hemorrhage evacuation decreases perihematomal edema. Stroke. 44:627–634. 2013.
Article27. Osbun JW, Reynolds MR, Barrow DL. Arteriovenous malformations: epidemiology, clinical presentation, and diagnostic evaluation. Handb Clin Neurol. 143:25–29. 2017.28. Park JK, Kim KS, Kim CB, Lee TY, Lee KS, Lee DH. The accuracy of ICD codes for cerebrovascular diseases in medical insurance claims. Korean J Prev Med. 33:76–82. 2000.29. Potts MB, Lau D, Abla AA, Kim H, Young WL, Lawton MT, et al. Current surgical results with low-grade brain arteriovenous malformations. J Neurosurg. 122:912–920. 2015.
Article30. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 49:e46–e110. 2018.
Article31. Rothwell PM, Coull AJ, Giles MF, Howard SC, Silver LE, Bull LM, et al. Change in stroke incidence, mortality, case-fatality, severity, and risk factors in Oxfordshire, UK from 1981 to 2004 (Oxford Vascular Study). Lancet. 363:1925–1933. 2004.
Article32. Sivenius J, Tuomilehto J, Immonen-Räihä P, Kaarisalo M, Sarti C, Torppa J, et al. Continuous 15-year decrease in incidence and mortality of stroke in Finland: the FINSTROKE study. Stroke. 35:420–425. 2004.
Article33. Steiner T, Rosand J, Diringer M. Intracerebral hemorrhage associated with oral anticoagulant therapy: current practices and unresolved questions. Stroke. 37:256–262. 2006.
Article34. Teo M, St George J, Lawton MT. Time for BARBADOS after ARUBA trial. Br J Neurosurg. 29:635–636. 2015.
Article35. Tonetti DA, Gross BA, Atcheson KM, Jankowitz BT, Kano H, Monaco EA 3rd, et al. The benefit of radiosurgery for ARUBA-eligible arteriovenous malformations: a practical analysis over an appropriate follow-up period. J Neurosurg. 128:1850–1854. 2018.
Article36. Tsai CF, Thomas B, Sudlow CL. Epidemiology of stroke and its subtypes in Chinese vs white populations: a systematic review. Neurology. 81:264–272. 2013.
Article37. Wong J, Slomovic A, Ibrahim G, Radovanovic I, Tymianski M. Microsurgery for ARUBA trial (a randomized trial of unruptured brain arteriovenous malformation)-eligible unruptured brain arteriovenous malformations. Stroke. 48:136–144. 2017.
Article38. Xia Z, Wu X, Li J, Liu Z, Chen F, Zhang L, et al. Minimally invasive surgery is superior to conventional craniotomy in patients with spontaneous supratentorial intracerebral hemorrhage: a systematic review and meta-analysis. World Neurosurg. 115:266–273. 2018.
Article39. Yang W, Caplan JM, Ye X, Wang JY, Braileanu M, Rigamonti D, et al. Racial associations with hemorrhagic presentation in cerebral arteriovenous malformations. World Neurosurg. 84:461–469. 2015.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intracranial Arteriovenous Malformation Associated Intracranial Aneurysms
- Cerebral Arteriovenous Malformation Associated with Intracranial Meningioma and Aneurysm: Case Report
- Ruptured Cerebral Arteriovenous Malformation with Giant Venous Aneurysm: Case Report
- Clinical Analysis of Spontaneous Intracranial Hemorrhage(from Jan.-'80 to Sep.-'87)
- Clinical Study on the Intracranial Arteriovenous Malformation