Intest Res.
2020 Apr;18(2):238-244. 10.5217/ir.2019.00104.
Clinical profile and outcomes of opioid abuse gastroenteropathy: an underdiagnosed disease entity
- Affiliations
-
- 1Department of Gastroenterology, Dayanand Medical College and Hospital, Ludhiana, India
- 2Department of Internal Medicine, Dayanand Medical College and Hospital, Ludhiana, India
- 3Department of Radiodiagnosis, Dayanand Medical College and Hospital, Ludhiana, India
- 4Department of Pathology, Dayanand Medical College and Hospital, Ludhiana, India
- KMID: 2501389
- DOI: http://doi.org/10.5217/ir.2019.00104
Abstract
- Background/Aims
Opioid-induced bowel dysfunction includes nausea, vomiting, constipation and abdominal distension. We describe patients presenting with gastrointestinal (GI) ulcers and ulcerated strictures secondary to opioid abuse, an entity not well described in literature.
Methods
This retrospective observational study included patients with opioid abuse gastroenteropathy presenting to Dayanand Medical College and Hospital, Ludhiana, India between January 2013 and December 2018. Opioid abuse gastroenteropathy was defined as gastric or small bowel ulcers and ulcerated strictures in patients abusing opioids, where all other possible etiologies of GI ulcers/strictures were excluded. Clinical, biochemical, endoscopic, radiological and histological parameters as well as response to treatment were assessed.
Results
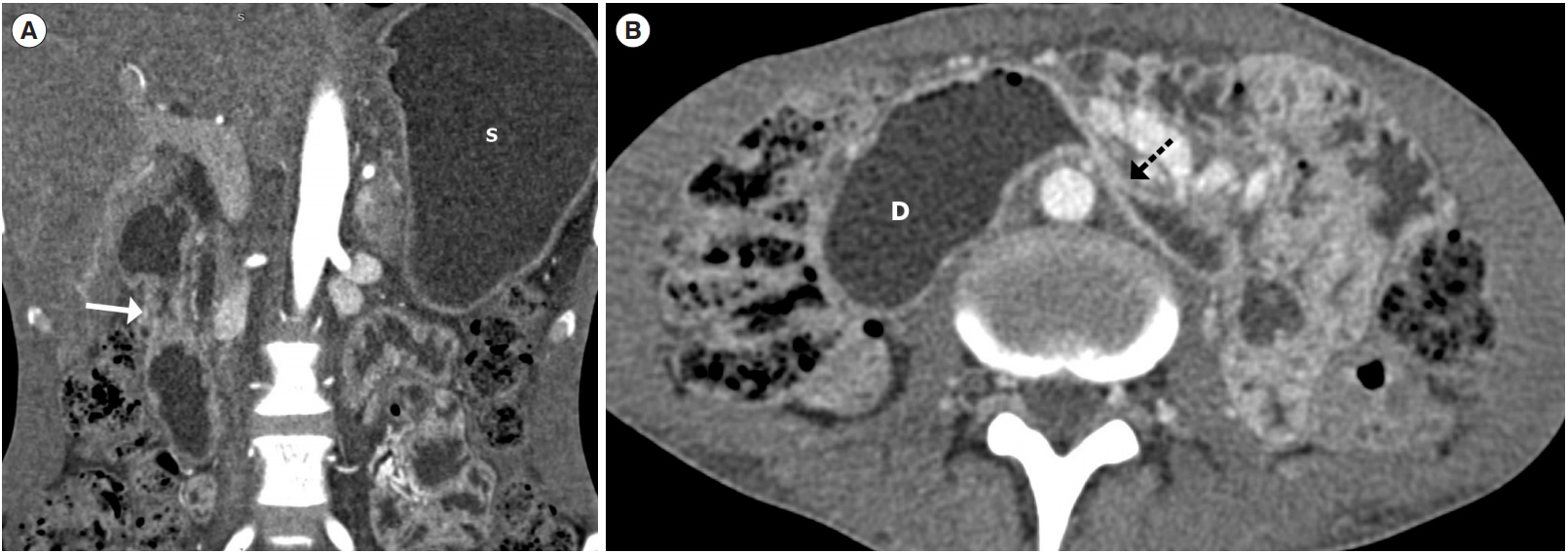
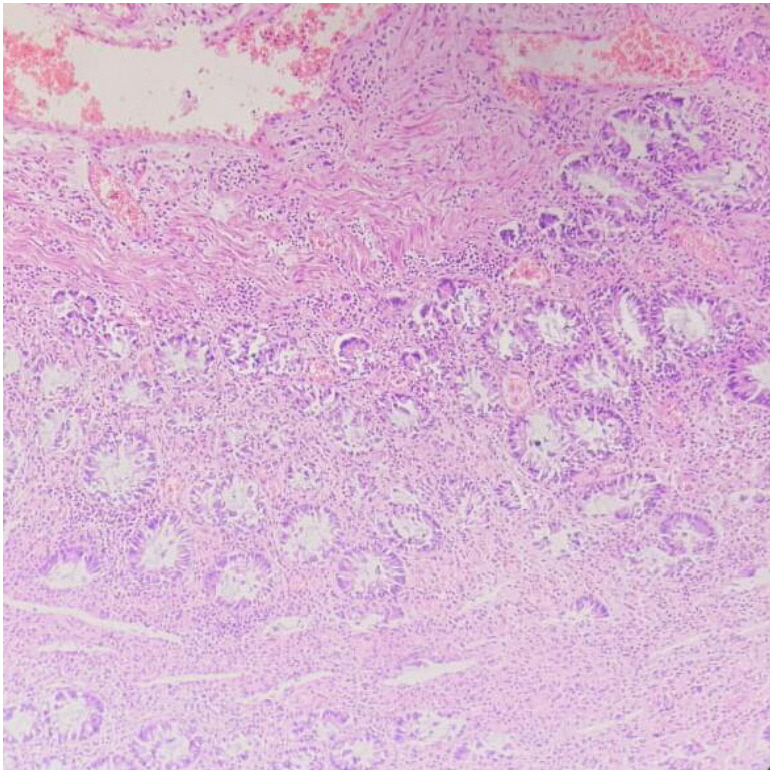
During the study period, 20 patients (mean age, 38.5±14.2 years; 100% males) were diagnosed to have opioid induced GI ulcers and/or ulcerated strictures. The mean duration of opioid consumption was 6.2±3.4 years. The mean duration of symptoms at presentation was 222.1±392.3 days. Thirteen patients (65%) had gastroduodenal involvement, 6 (30%) had a jejunoileal disease and 1 (5%) had an ileocecal stricture. Two patients (10%) presented with upper GI bleeding, 11 (55%) had features of gastric outlet obstruction and 7 (35%) presented with small bowel obstruction. Abdominal pain and iron deficiency anemia were the most common presentations. Only 1 patient (5%) responded to proton pump inhibitors, 3 (15%) had a lasting response to endoscopic balloon dilatation, while all other (80%) required surgical intervention.
Conclusions
Opioid abuse gastroenteropathy presents as ulcers and ulcerated strictures which respond poorly to medical management and endoscopic balloon dilatation. A majority of these cases need surgical intervention.
Figure
Reference
-
1. Khullar SK, DiSario JA. Gastric outlet obstruction. Gastrointest Endosc Clin N Am. 1996; 6:585–603.
Article2. Gill RS, Kaffes AJ. Small bowel stricture characterization and outcomes of dilatation by double-balloon enteroscopy: a single-centre experience. Therap Adv Gastroenterol. 2014; 7:108–114.
Article3. Joshi A, Falodia S, Kumar N, Solanki RL. Small intestine strictures in opium addicts: an unrecognized cause of intestinal obstruction. Indian J Gastroenterol. 2018; 37:169–173.
Article4. Mohan D, Sundaram KR, Sharma HK. A study of drug abuse in rural areas of Punjab (India). Drug Alcohol Depend. 1986; 17:57–66.
Article5. Chaturvedi HK, Mahanta J, Bajpai RC, Pandey A. Correlates of opium use: retrospective analysis of a survey of tribal communities in Arunachal Pradesh, India. BMC Public Health. 2013; 13:325.
Article6. Pulimood AB, Amarapurkar DN, Ghoshal U, et al. Differentiation of Crohn’s disease from intestinal tuberculosis in India in 2010. World J Gastroenterol. 2011; 17:433–443.
Article7. Frye JM, Hansel SL, Dolan SG, et al. NSAID enteropathy: appearance at CT and MR enterography in the age of multi-modality imaging and treatment. Abdom Imaging. 2015; 40:1011–1025.
Article8. Berterame S, Erthal J, Thomas J, et al. Use of and barriers to access to opioid analgesics: a worldwide, regional, and national study. Lancet. 2016; 387:1644–1656.
Article9. Ray R, Kattimani S, Sharma HK. Opium abuse and its management: global scenario. WHO Web site. https://www.who.int/substance_abuse/activities/opium_abuse_and_its_management.pdf. Accessed August 1, 2019.10. Farhat S, Hussain SS, Rather YH, Hussain SK. Sociodemographic profile and pattern of opioid abuse among patients presenting to a de-addiction centre in tertiary care hospital of Kashmir. J Basic Clin Pharm. 2015; 6:94–97.
Article11. Khansari M, Sohrabi M, Zamani F. The useage of opioids and their adverse effects in gastrointestinal practice: a review. Middle East J Dig Dis. 2013; 5:5–16.12. Charney DS, Redmond DE Jr, Galloway MP, et al. Naltrexone precipitated opiate withdrawal in methadone addicted human subjects: evidence for noradrenergic hyperactivity. Life Sci. 1984; 35:1263–1272.
Article13. Reece AS, Hulse GK. Impact of lifetime opioid exposure on arterial stiffness and vascular age: cross-sectional and longitudinal studies in men and women. BMJ Open. 2014; 4:e004521.
Article14. Darke S, Duflou J, Torok M. The comparative toxicology and major organ pathology of fatal methadone and heroin toxicity cases. Drug Alcohol Depend. 2010; 106:1–6.
Article15. Ebdali RT, Tabaee SS, Tabaei S. Cardiovascular complications and related risk factors underlying opium consumption. J Cell Physiol. 2019; 234:8487–8495.
Article16. Masoudkabir F, Sarrafzadegan N, Eisenberg MJ. Effects of opium consumption on cardiometabolic diseases. Nat Rev Cardiol. 2013; 10:733–740.
Article17. Purohit P, Nebhinani N, Sharma P. Evaluation of antioxidant status, high sensitivity C-reactive protein, and insulin resistance in male chronic opiate users without comorbidities. Indian J Psychol Med. 2017; 39:299–305.
Article18. Ambekar A, Murthy P, Basu D, Rao GP, Mohan A. Challenges in the scale-up of opioid substitution treatment in India. Indian J Psychiatry. 2017; 59:6–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- 99mTc-HSA-DTPA Scintigraphy of Protein-Losing Gastroenteropathy Associated with Mixed Connective Tissue Disease Before and After Immunosuppressive Therapy
- Child sexual abuse and pediatricians
- Recovery outcomes of Korean adolescents with substance Abuse problems
- Validation of Nursing-sensitive Patient Outcomes: Focused on Abuse Outcomes
- Medical environment and drug abuse among physicians: current state and problems in Korea