Cancer Res Treat.
2020 Jan;52(1):60-73. 10.4143/crt.2018.660.
Disparities in the Participation Rate of Colorectal Cancer Screening by Fecal Occult Blood Test among People with Disabilities: A National Database Study in South Korea
- Affiliations
-
- 1Department of Family Medicine/Supportive Care Center, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Digital Health, SAIHST, Sungkyunkwan University, Seoul, Korea
- 3Division of Gastroenterology, Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 4Department of Medical Statistics, The Catholic University of Korea, Seoul, Korea
- 5College of Medicine, Chungbuk National University/Chungbuk National University Hospital, Cheongju, Korea
- 6Department of Cancer Control and Population Health, Graduate School of Cancer Science and Policy, National Cancer Center, Goyang, Korea
- 7Department of Preventive Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 8Big Data Steering Department, National Health Insurance Service, Wonju, Korea
- KMID: 2501202
- DOI: http://doi.org/10.4143/crt.2018.660
Abstract
- Purpose
Implementation of screening program may lead to increased health disparity within the population if participation differs by socioeconomic status. In Korea, colorectal cancer screening is provided at no or minimal cost to all people over 50 by National Cancer Screening Program. We investigated colorectal cancer screening participation rate and its trend over the last 10 years in relation to disabilities.
Materials and Methods
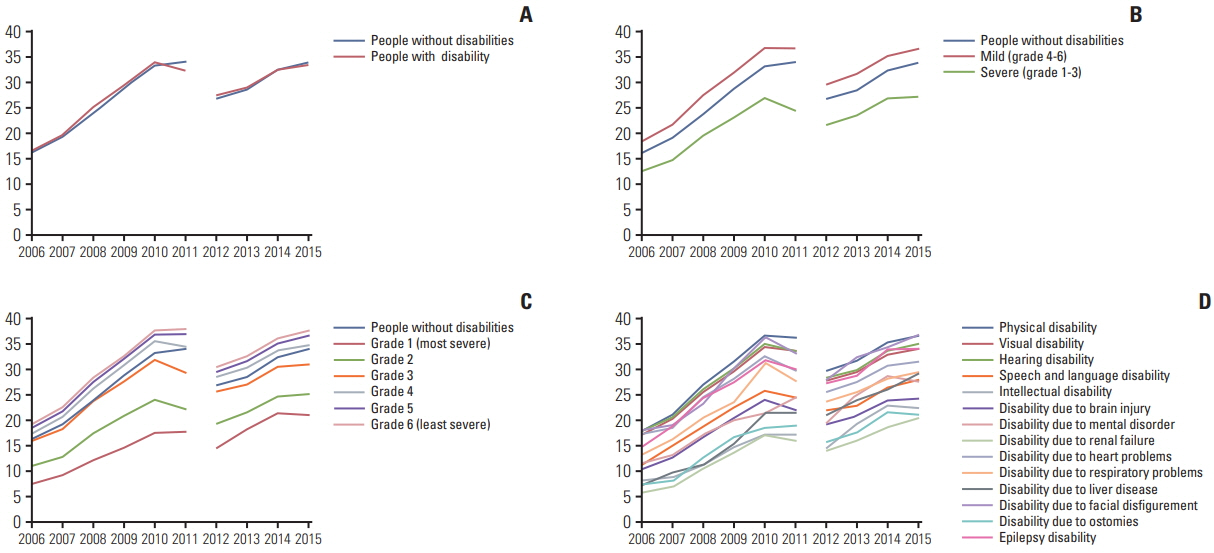
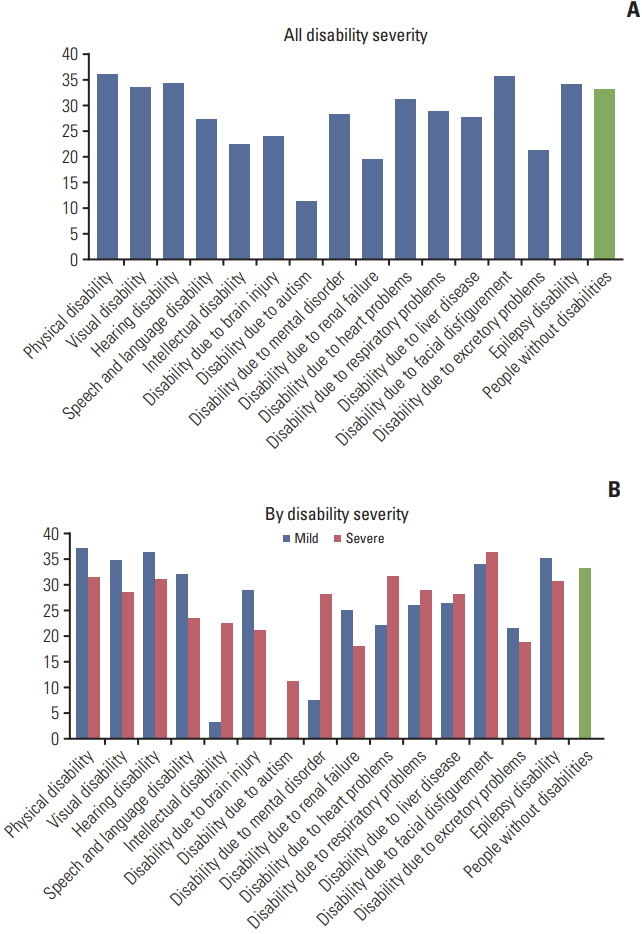
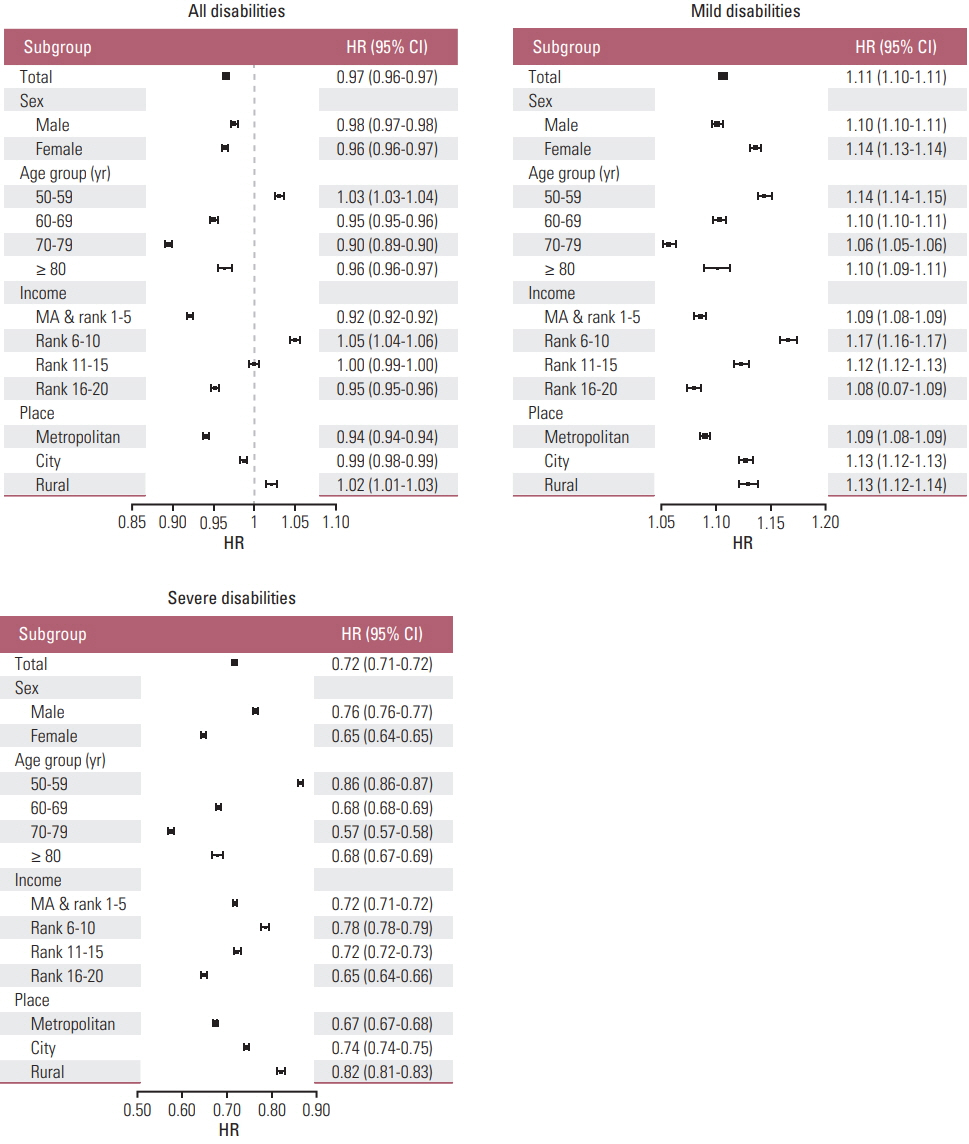
We linked national disability registration data with National Cancer Screening Program data. Age, sex-standardized participation rates were analyzed by type and severity of disability for each year, and factors associated with colorectal cancer screening participation were examined by multivariate logistic regression.
Results
Age, sex-standardized participation rate in people without disability increased from 16.2 to 33.9% (change, +17.7), but it increased from 12.7% to 27.2% (change, +14.5) among people with severe disability. People with severe disabilities showed a markedly lower colorectal cancer screening participation rate than people without disability (adjusted odds ratio [aOR], 0.714; 95% confidence interval, 0.713 to 0.720). People with autism (aOR, 0.468), renal failure (aOR, 0.498), brain injury (aOR, 0.581), ostomy (aOR, 0.602), and intellectual disability (aOR, 0.610) showed the lowest participation rates.
Conclusion
Despite the availability of a National Cancer Screening Program and overall increase of its usage in the Korean population, a significant disparity was found in colorectal cancer screening participation, especially in people with severe disabilities and or several specific types of disabilities. Greater effort is needed to identify the barriers faced by these particularly vulnerable groups and develop targeted interventions to reduce inequality.
Figure
Reference
-
References
1. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015; 65:87–108.
Article2. Lin JS, Piper MA, Perdue LA, Rutter CM, Webber EM, O'Connor E, et al. Screening for colorectal cancer: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2016; 315:2576–94.3. Jacob BJ, Moineddin R, Sutradhar R, Baxter NN, Urbach DR. Effect of colonoscopy on colorectal cancer incidence and mortality: an instrumental variable analysis. Gastrointest Endosc. 2012; 76:355–64.
Article4. Horner-Johnson W, Dobbertin K, Lee JC, Andresen EM; Expert Panel on Disability and Health Disparities. Disparities in health care access and receipt of preventive services by disability type: analysis of the medical expenditure panel survey. Health Serv Res. 2014; 49:1980–99.
Article5. Ramirez A, Farmer GC, Grant D, Papachristou T. Disability and preventive cancer screening: results from the 2001 California Health Interview Survey. Am J Public Health. 2005; 95:2057–64.
Article6. Littman AJ, Koepsell TD, Forsberg CW, Haselkorn JK, Boyko EJ. Preventive services in veterans in relation to disability. J Rehabil Res Dev. 2012; 49:339–50.
Article7. Wei W, Findley PA, Sambamoorthi U. Disability and receipt of clinical preventive services among women. Womens Health Issues. 2006; 16:286–96.
Article8. Iezzoni LI, Kurtz SG, Rao SR. Trends in colorectal cancer screening over time for persons with and without chronic disability. Disabil Health J. 2016; 9:498–509.9. Deroche CB, McDermott SW, Mann JR, Hardin JW. Colorectal cancer screening adherence in selected disabilities over 10 years. Am J Prev Med. 2017; 52:735–41.
Article10. Ouellette-Kuntz H, Coo H, Cobigo V, Wilton AS. Uptake of colorectal cancer screening among Ontarians with intellectual and developmental disabilities. PLoS One. 2015; 10:e0118023.
Article11. Shin DW, Lee JW, Jung JH, Han K, Kim SY, Choi KS, et al. Disparities in cervical cancer screening among women with disabilities: a national database study in South Korea. J Clin Oncol. 2018; 36:2778–86.
Article12. Yoo KY. Cancer control activities in the Republic of Korea. Jpn J Clin Oncol. 2008; 38:327–33.
Article13. Choi KS, Lee HY, Jun JK, Shin A, Park EC. Adherence to follow-up after a positive fecal occult blood test in an organized colorectal cancer screening program in Korea, 2004-2008. J Gastroenterol Hepatol. 2012; 27:1070–7.
Article14. Robertson DJ, Lee JK, Boland CR, Dominitz JA, Giardiello FM, Johnson DA, et al. Recommendations on fecal immunochemical testing to screen for colorectal neoplasia: a consensus statement by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2017; 152:1217–37.
Article15. Suh M, Song S, Cho HN, Park B, Jun JK, Choi E, et al. Trends in participation rates for the National Cancer Screening Program in Korea, 2002-2012. Cancer Res Treat. 2017; 49:798–806.
Article16. Choi YJ, Kang JK, Lee SH, Cho YS, Yook TM. An analysis of the compliance to colorectal cancer screening using the data from national cancer screening program. Goyang: National Health Insurance Service Ilsan Hospital;2015.17. Lee H, Cho J, Shin DW, Lee SP, Hwang SS, Oh J, et al. Association of cardiovascular health screening with mortality, clinical outcomes, and health care cost: a nationwide cohort study. Prev Med. 2015; 70:19–25.
Article18. Shin DW, Cho B, Guallar E. Korean National Health Insurance Database. JAMA Intern Med. 2016; 176:138.
Article19. Soeng SC, Kim YY, Khang YH, Park JH, Kang HJ, Lee H, et al. Data resource profile: the National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol. 2017; 46:799–800.20. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46:e15.
Article21. Carlos CA, McCulloch CE, Hsu CY, Grimes B, Pavkov ME, Burrows NR, et al. Colon cancer screening among patients receiving dialysis in the United States: are we choosing wisely? J Am Soc Nephrol. 2017; 28:2521–8.
Article22. Yoon NH, Lee HY, Kwak MS, Choi KS, Jun JK, Kim MK, et al. Comparison of satisfaction with cancer screening at mobile van and static sites: National Cancer Screening Program in Korea. Jpn J Clin Oncol. 2009; 39:169–74.
Article23. Baker DW, Brown T, Buchanan DR, Weil J, Balsley K, Ranalli L, et al. Comparative effectiveness of a multifaceted intervention to improve adherence to annual colorectal cancer screening in community health centers: a randomized clinical trial. JAMA Intern Med. 2014; 174:1235–41.24. Goldman SN, Liss DT, Brown T, Lee JY, Buchanan DR, Balsley K, et al. Comparative effectiveness of multifaceted outreach to initiate colorectal cancer screening in community health centers: a randomized controlled trial. J Gen Intern Med. 2015; 30:1178–84.
Article25. de Klerk CM, Gupta S, Dekker E, Essink-Bot ML; Expert Working Group ‘Coalition to reduce inequities in colorectal cancer screening’ of the World Endoscopy Organization. Socioeconomic and ethnic inequities within organised colorectal cancer screening programmes worldwide. Gut. 2018; 67:679–87.
Article26. Church TR, Yeazel MW, Jones RM, Kochevar LK, Watt GD, Mongin SJ, et al. A randomized trial of direct mailing of fecal occult blood tests to increase colorectal cancer screening. J Natl Cancer Inst. 2004; 96:770–80.
Article27. Kim S, Kwon S, Subramanian SV. Has the National Cancer Screening Program reduced income inequalities in screening attendance in South Korea? Cancer Causes Control. 2015; 26:1617–25.
Article28. Hahm MI, Chen HF, Miller T, O'Neill L, Lee HY. Why do some people choose opportunistic rather than organized cancer screening? The Korean National Health and Nutrition Examination Survey (KNHANES) 2010-2012. Cancer Res Treat. 2017; 49:727–38.
Article29. World Health Organization. Towards a common language for functioning, disability and health: ICF, The Internatinoal Classification of Functioning, Disability and Health. Geneva: World Health Organization;2002.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- National cancer screening program for colorectal cancer in Korea
- Performance Evaluation of the HM-JACKarc Analyser for Fecal Occult Blood Test
- Usefulness of Fecal Occult Blood Test as a Colorectal Cancer Screening Method
- Results of Colorectal Cancer Screening of the National Cancer Screening Program in Korea, 2008
- Evaluation of Hemo Techt NS-plus C15 Automatic Analyzer for Fecal Occult Blood Test