Arch Hand Microsurg.
2020 Mar;25(1):17-23. 10.12790/ahm.19.0065.
Analysis of Risk Factors for Occult Surgical Neck Fracture Accompanying Isolated Greater Tuberosity Fracture of Humerus
- Affiliations
-
- 1Department of Orthopedic Surgery, Bucheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Bucheon, Korea
- 2Department of Orthopedic Surgery, Bucheon Hi Hospital, Bucheon, Korea
- 3Department of Orthopedic Surgery, Daejeon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Daejeon, Korea
- KMID: 2501105
- DOI: http://doi.org/10.12790/ahm.19.0065
Abstract
- Purpose
An occult surgical neck fracture can be accompanied in isolated greater tuberosity fracture of humerus. The risk factors of occult surgical neck fracture in isolated greater tuberosity fracture were statistically analyzed.
Methods
From 2008 to 2017, 74 patients with isolated greater tuberosity fracture of humerus were selected. The occult surgical neck fracture was evaluated by computed tomography or magnetic resonance imaging. Patients were divided into two groups, those with isolated greater tuberosity fractures (group I) and isolated greater tuberosity fractures with occult surgical neck fracture (group II). For the risk factor analysis, the age, sex, underlying disease, injury mechanism, and body mass index between the two groups were compared. Radiologically, fracture pattern, the amount of displacement, and the presence and direction of the shoulder joint dislocation were compared.
Results
In multivariate analysis, factors independently related to the occurrence of occult surgical neck fractures were gender and whether or not the joint dislocation. In women (odds ratio [OR]=14.806; 95% confidence interval [CI], 1.188–184.503; p=0.036) and in cases where no joint dislocation occult surgical neck fracture (OR=0.018; 95% CI, 0.001–0.271; p=0.004) was accompanied more frequently and occurred statistically.
Conclusion
Care must be taken in cases of female and the absence of shoulder dislocation in isolated greater tuberosity fracture because of the possibility of occult surgical neck fracture.
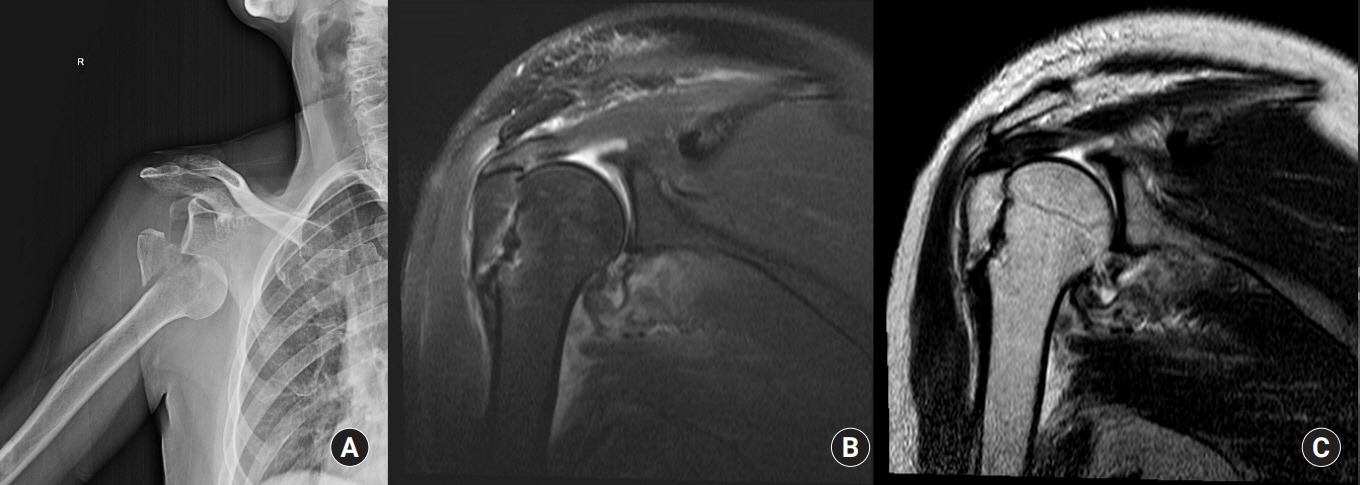
Figure
Reference
-
References
1. Green A, Izzi J Jr. Isolated fractures of the greater tuberosity of the proximal humerus. J Shoulder Elbow Surg. 2003; 12:641–9.
Article2. White EA, Skalski MR, Patel DB, et al. Isolated greater tuberosity fractures of the proximal humerus: anatomy, injury patterns, multimodality imaging, and approach to management. Emerg Radiol. 2018; 25:235–46.
Article3. Shaw L, Hong CK, Kuan FC, Lin CL, Wang PH, Su WR. The incidence of occult and missed surgical neck fractures in patients with isolated greater tuberosity fracture of the proximal humerus. BMC Musculoskelet Disord. 2019; 20:482.
Article4. Platzer P, Thalhammer G, Oberleitner G, et al. Displaced fractures of the greater tuberosity: a comparison of operative and nonoperative treatment. J Trauma. 2008; 65:843–8.
Article5. Rath E, Alkrinawi N, Levy O, Debbi R, Amar E, Atoun E. Minimally displaced fractures of the greater tuberosity: outcome of non-operative treatment. J Shoulder Elbow Surg. 2013; 22:e8–11.
Article6. Mattyasovszky SG, Burkhart KJ, Ahlers C, et al. Isolated fractures of the greater tuberosity of the proximal humerus: a long-term retrospective study of 30 patients. Acta Orthop. 2011; 82:714–20.7. Mutch J, Laflamme GY, Hagemeister N, Cikes A, Rouleau DM. A new morphological classification for greater tuberosity fractures of the proximal humerus: validation and clinical implications. Bone Joint J. 2014; 96-B:646–51.8. Gruson KI, Ruchelsman DE, Tejwani NC. Isolated tuberosity fractures of the proximal humeral: current concepts. Injury. 2008; 39:284–98.9. Court-Brown CM, Garg A, McQueen MM. The epidemiology of proximal humeral fractures. Acta Orthop Scand. 2001; 72:365–71.
Article10. Wu J, Han Z, Wang Q, Wu X. Inferior displacement of greater tuberosity fracture suggests an occult humeral neck fracture: a retrospective single-centre study. Int Orthop. 2019; 43:1429–34.11. Court-Brown CM, Cattermole H, McQueen MM. Impacted valgus fractures (B1.1) of the proximal humerus: the results of non-operative treatment. J Bone Joint Surg Br. 2002; 84:504–8.12. Court-Brown CM, McQueen MM. The impacted varus (A2.2) proximal humeral fracture: prediction of outcome and results of nonoperative treatment in 99 patients. Acta Orthop Scand. 2004; 75:736–40.
Article13. Hanson B, Neidenbach P, de Boer P, Stengel D. Functional outcomes after nonoperative management of fractures of the proximal humerus. J Shoulder Elbow Surg. 2009; 18:612–21.14. Haubro M, Stougaard C, Torfing T, Overgaard S. Sensitivity and specificity of CT- and MRI-scanning in evaluation of occult fracture of the proximal femur. Injury. 2015; 46:1557–61.
Article15. Gumina S, Carbone S, Postacchini F. Occult fractures of the greater tuberosity of the humerus. Int Orthop. 2009; 33:171–4.
Article16. Cuomo F. Two-part displaced tuberosity fractures of the proximal humerus. In : Flatow EL, Ulrich C, editors. Humerus. Oxford, UK: Butterworth-Heinemann;1996. p. 23–36.17. Flatow EL, Cuomo F, Maday MG, Miller SR, McIlveen SJ, Bigliani LU. Open reduction and internal fixation of two-part displaced fractures of the greater tuberosity of the proximal part of the humerus. J Bone Joint Surg Am. 1991; 73:1213–8.
Article18. Hebert-Davies J, Mutch J, Rouleau D, Laflamme GY. Delayed migration of greater tuberosity fractures associated with anterior shoulder dislocation. J Orthop Trauma. 2015; 29:e396–400.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Shoulder Quadruple Dislocation Fracture: Fracture of Glenoid Rim, Coracoid Process, Greater Tuberosity, Surgical Neck of Humerus Associated with Anterior Shoulder Dislocation: A Case Report
- Isolated Avulsion Fracture of the Lesser Tuberosity of the Humerus: A Case Report
- The Surgical Outcomes of Isolated Greater Tuberosity Fractures of the Proximal Humerus Fixed with the Spring Plate
- Luxatio Erecta Associated with Greater Tuberosity and Neck Fracture: A Case Report
- Isolated Avulsion Fracture of the Subscapularis from the Lesser Tuberosity of the Humerus in a 12-Year-Old Boy - A Case Report -