Ann Rehabil Med.
2020 Feb;44(1):38-47. 10.5535/arm.2020.44.1.38.
Characteristics of Patients With Esophageal Dysphagia Assessed by Chest X-Ray Imaging After Videofluoroscopic Swallowing Study
- Affiliations
-
- 1Department of Rehabilitation Medicine, Kangwon National University Hospital, Kangwon National University School of Medicine, Chuncheon, Korea
- 2Division of Gastroenterology and Hepatology, Department of Internal Medicine, Kangwon National University School of Medicine, Chuncheon, Korea
- KMID: 2501044
- DOI: http://doi.org/10.5535/arm.2020.44.1.38
Abstract
Objective
To evaluate the prevalence rate, types, characteristics, and associated factors of esophageal dysphagia detected on chest X-ray images after videofluoroscopic swallowing study (VFSS).
Methods
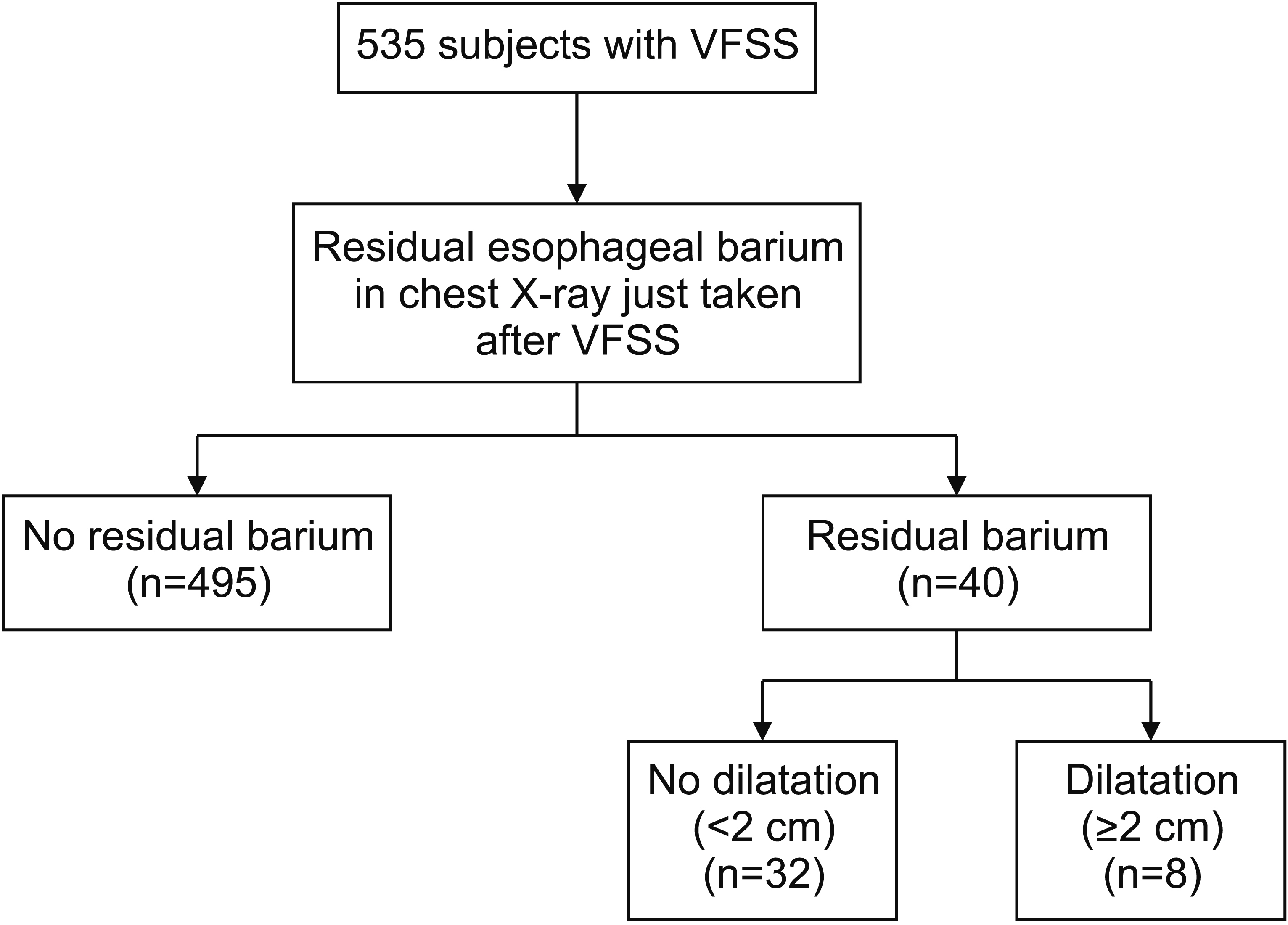
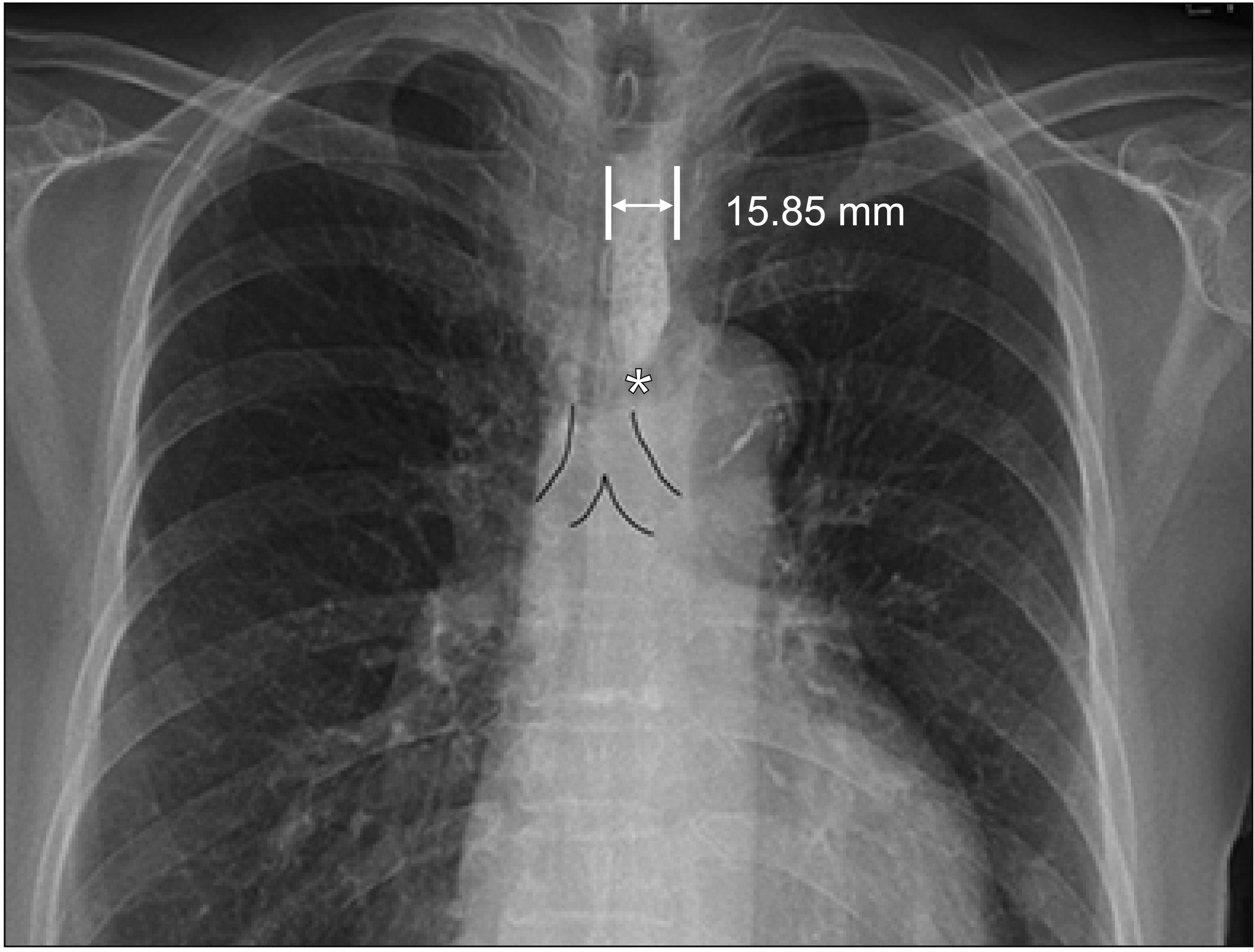
The medical records of 535 adults were reviewed retrospectively. Chest X-ray images taken after barium swallow study were analyzed and presence of any residual barium in the esophagus was considered as esophageal dysphagia. Esophageal dysphagia was classified based on the largest width of barium deposit (mild, <2 cm; severe ≥2 cm) and the anatomic level at which it was located (upper and lower esophagus).
Results
Esophageal residual barium on chest X-ray images was identified in 40 patients (7.5%, 40/535). Esophageal dysphagia was more frequent in individuals aged 65–79 years (odds ratio=4.78, p<0.05) than in those aged <65 years. Mild esophageal dysphagia was more frequent (n=32) than its severe form (n=8). Lower esophageal dysphagia was more frequent (n=31) than upper esophageal dysphagia (n=9). Esophageal residual barium in patients diagnosed with esophageal cancer or lung cancer was significantly associated with severe esophageal dysphagia (p<0.05) and at the upper esophagus level (p<0.01).
Conclusion
Esophageal residual barium was observed on chest X-ray imaging after VFSS. Esophageal barium in the upper esophagus with a diameter of ≥2 cm is an important indicator of malignancy, and chest X-ray image taken after VFSS is an important step to evaluate the presence of esophageal disorder.
Figure
Cited by 1 articles
-
Esophageal Motility Disorders in Patients With Esophageal Barium Residue After Videofluoroscopic Swallowing Study
Jintae Park, Sora Baek, Gowun Kim, Seung-Joo Nam, Ji Hyun Kim
Ann Rehabil Med. 2022;46(5):237-247. doi: 10.5535/arm.22039.
Reference
-
1. Chilukuri P, Odufalu F, Hachem C. Dysphagia. Mo Med. 2018; 115:206–10.2. Kruger D. Assessing esophageal dysphagia. JAAPA. 2014; 27:23–30.
Article3. Triadafilopoulos G, Hallstone A, Nelson-Abbott H, Bedinger K. Oropharyngeal and esophageal interrelationships in patients with nonobstructive dysphagia. Dig Dis Sci. 1992; 37:551–7.
Article4. Mendell DA, Logemann JA. A retrospective analysis of the pharyngeal swallow in patients with a clinical diagnosis of GERD compared with normal controls: a pilot study. Dysphagia. 2002; 17:220–6.
Article5. Jones B, Donner MW, Rubesin SE, Ravich WJ, Hendrix TR. Pharyngeal findings in 21 patients with achalasia of the esophagus. Dysphagia. 1987; 2:87–92.
Article6. Martin RE, Letsos P, Taves DH, Inculet RI, Johnston H, Preiksaitis HG. Oropharyngeal dysphagia in esophageal cancer before and after transhiatal esophagectomy. Dysphagia. 2001; 16:23–31.
Article7. Smith DF, Ott DJ, Gelfand DW, Chen MY. Lower esophageal mucosal ring: correlation of referred symptoms with radiographic findings using a marshmallow bolus. AJR Am J Roentgenol. 1998; 171:1361–5.
Article8. Han TR, Paik NJ, Park JW. The safety of videofluoroscopic swallowing study (VFSS). J Korean Acad Rehabil Med. 2000; 24:215–8.9. Kostic SV, Rice TW, Baker ME, Decamp MM, Murthy SC, Rybicki LA, et al. Timed barium esophagogram: a simple physiologic assessment for achalasia. J Thorac Cardiovasc Surg. 2000; 120:935–43.
Article10. Levine MS, Rubesin SE, Laufer I. Barium esophagography: a study for all seasons. Clin Gastroenterol Hepatol. 2008; 6:11–25.
Article11. Lawal A, Shaker R. Esophageal dysphagia. Phys Med Rehabil Clin N Am. 2008; 19:729–45.
Article12. Miles A, McMillan J, Ward K, Allen J. Esophageal visualization as an adjunct to the videofluoroscopic study of swallowing. Otolaryngol Head Neck Surg. 2015; 152:488–93.
Article13. Watts S, Gaziano J, Jacobs J, Richter J. Improving the diagnostic capability of the modified barium swallow study through standardization of an esophageal sweep protocol. Dysphagia. 2019; 34:34–42.
Article14. Kostic S, Andersson M, Hellstrom M, Lonroth H, Lundell L. Timed barium esophagogram in the assessment of patients with achalasia: reproducibility and observer variation. Dis Esophagus. 2005; 18:96–103.
Article15. Kuo B, Urma D. Esophagus-anatomy and development. GI Motil Online 2006. [Epub]. https://www.nature.com/gimo/contents/pt1/full/gimo6.html.16. Chikwe J, Cooke D, Weiss A. Esophagus. Cardiothoracic surgery. 2nd ed. Oxford, UK: Oxford University Press;2013.17. Thorek P. Esophagogastrointestinal tract. In : . New York, NY: Springer;1985. p. 418–513.18. Skandalakis JE, Skandalakis LJ. Esophagus. In : Skandalakis JE, Skandalakis PN, Skandalakis LJ, editors. Surgical anatomy and technique: a pocket manual. 2nd ed. New York, NY: Springer;2000.19. Khan TA, Shragge BW, Crispin JS, Lind JF. Esophageal motility in the elderly. Am J Dig Dis. 1977; 22:1049–54.
Article20. Lee J, Anggiansah A, Anggiansah R, Young A, Wong T, Fox M. Effects of age on the gastroesophageal junction, esophageal motility, and reflux disease. Clin Gastroenterol Hepatol. 2007; 5:1392–8.
Article21. Shim YK, Kim N, Park YH, Lee JC, Sung J, Choi YJ, et al. Effects of age on esophageal motility: use of highresolution esophageal impedance manometry. J Neurogastroenterol Motil. 2017; 23:481.
Article22. Gutschow CA, Leers JM, Schroder W, Prenzel KL, Fuchs H, Bollschweiler E, et al. Effect of aging on esophageal motility in patients with and without GERD. Ger Med Sci. 2011; 9:Doc22.23. Andrews JM, Fraser RJ, Heddle R, Hebbard G, Checklin H. Is esophageal dysphagia in the extreme elderly (>or=80 years) different to dysphagia younger adults? A clinical motility service audit. Dis Esophagus. 2008; 21:656–9.24. International Agency for Research on Cancer. Cancer fact sheets [Internet]. Lyon, France: International Agency for Research on Cancer;c2018; [cited 2020 Jan 15]. http://gco.iarc.fr/today/fact-sheets-cancers.25. Pennathur A, Gibson MK, Jobe BA, Luketich JD. Oesophageal carcinoma. Lancet. 2013; 381:400–12.
Article26. Napier KJ, Scheerer M, Misra S. Esophageal cancer: a review of epidemiology, pathogenesis, staging workup and treatment modalities. World J Gastrointest Oncol. 2014; 6:112–20.
Article27. Abbas G, Krasna M. Overview of esophageal cancer. Ann Cardiothorac Surg. 2017; 6:131–6.
Article28. Shin A, Won YJ, Jung HK, Kong HJ, Jung KW, Oh CM, et al. Trends in incidence and survival of esophageal cancer in Korea: analysis of the Korea Central Cancer Registry Database. J Gastroenterol Hepatol. 2018; 33:1961–8.
Article29. Makker HK, Chisholm R, Rate AJ, Bancewicz J, Bernstein A. Dysphagia due to secondary achalasia as an early manifestation of squamous cell carcinoma. Postgrad Med J. 1995; 71:502–4.
Article30. Camidge DR. The causes of dysphagia in carcinoma of the lung. J R Soc Med. 2001; 94:567–72.
Article31. Neyaz Z, Gupta M, Ghoshal UC. How to perform and interpret timed barium esophagogram. J Neurogastroenterol Motil. 2013; 19:251–6.
Article32. Gray C, Sivaloganathan S, Simpkins KC. Aspiration of high-density barium contrast medium causing acute pulmonary inflammation--report of two fatal cases in elderly women with disordered swallowing. Clin Radiol. 1989; 40:397–400.33. Katsanoulas C, Passakiotou M, Mouloudi E, Georgopoulou V, Gritsi-Gerogianni N. Severe barium sulphate aspiration: a report of two cases and review of the literature. Signa Vitae. 2007; 2:25–8.