Anesth Pain Med.
2020 Apr;15(2):226-232. 10.17085/apm.2020.15.2.226.
Vocal cord paralysis following general anesthesia with endotracheal intubation: a clinical review on 43 cases
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Inje University College of Medicine, Busan, Korea
- KMID: 2500976
- DOI: http://doi.org/10.17085/apm.2020.15.2.226
Abstract
- Background
Vocal cord paralysis (VCP) is one of the most stressful experiences for patients undergoing general anesthesia. Moreover, it is a risk factor for aspiration pneumonia and may increase morbidity and mortality. We examined several clinical features of the condition by reviewing the medical records of patients who experienced VCP following general anesthesia.
Methods
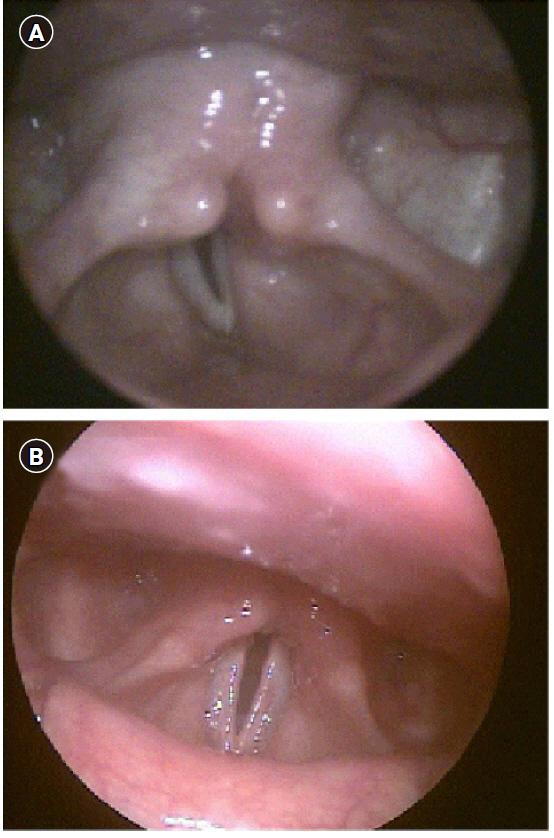
We reviewed the medical records of 321 patients who consulted an otolaryngologist owing to hoarseness, sore throat, throat discomfort, or dysphagia after general anesthesia. Among these, we included in the present study 43 patients who were diagnosed with VCP by laryngoscopy, who did not have symptoms of suspected VCP before surgery, who had no past history of VCP, and for whom endotracheal intubation was not continued after surgery.
Results
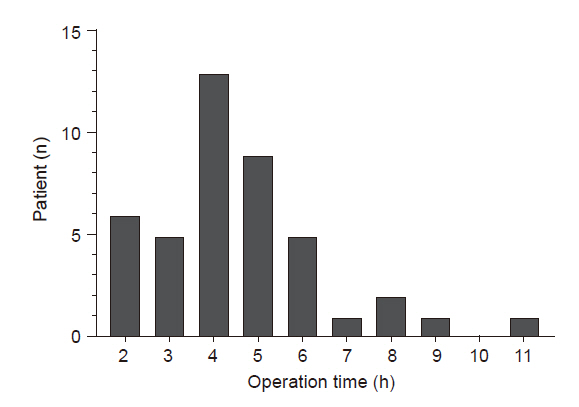
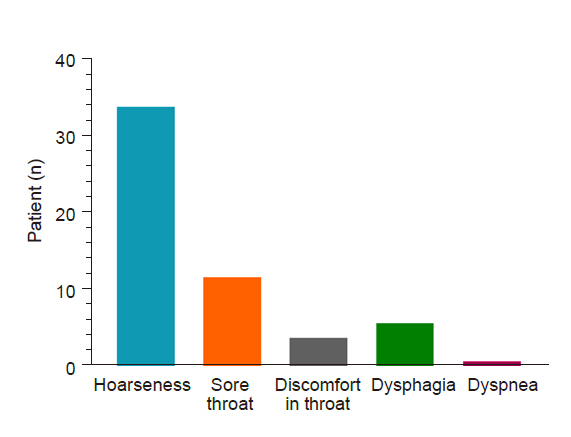
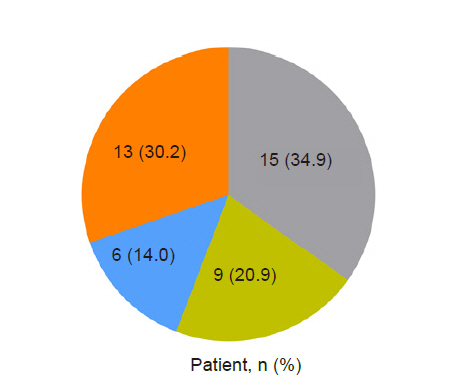
The mean age of patients with VCP was 51.28 years. With respect to surgical site, the most common was upper limb surgery, performed in 12 cases (9 cases were performed in sitting posture. With respect to surgical duration, only 11 cases lasted less than 3 h, whereas 32 cases required a surgical duration longer than 3 h. The most common symptom of VCP was hoarseness. Nine of the patients with VCP recovered spontaneously, but VCP persisted in 13 cases until the final follow-up examination.
Conclusions
We hope that this study might call attention to the occurrence of VCP following general anesthesia. Moreover, it is necessary to further evaluate the reasons for the higher incidence of VCP in upper limb surgery performed in sitting posture.
Figure
Reference
-
1. David DS, Shah M. Vocal cord paralysis following intubation. JAMA. 1971; 216:1645–6.2. Domino KB, Posner KL, Caplan RA, Cheney FW. Airway injury during anesthesia: a closed claims analysis. Anesthesiology. 1999; 91:1703–11.3. Holley HS, Gildea JE. Vocal cord paralysis after tracheal intubation. JAMA. 1971; 215:281–4.4. Flint P, Haughey B, Lund V, Niparko J, Robbins K, Thomas JR, et al. Cummings otolaryngology: head and neck surgery. 6th ed. Philadelphia: Elsevier;2015.5. Takano S, Nito T, Tamaruya N, Kimura M, Tayama N. Single institutional analysis of trends over 45 years in etiology of vocal fold paralysis. Auris Nasus Larynx. 2012; 39:597–600.6. Hamdan AL, Moukarbel RV, Farhat F, Obeid M. Vocal cord paralysis after open-heart surgery. Eur J Cardiothorac Surg. 2002; 21:671–4.7. Hulscher JB, van Sandick JW, Devriese PP, van Lanschot JJ, Obertop H. Vocal cord paralysis after subtotal oesophagectomy. Br J Surg. 1999; 86:1583–7.8. Kikura M, Suzuki K, Itagaki T, Takada T, Sato S. Age and comorbidity as risk factors for vocal cord paralysis associated with tracheal intubation. Br J Anaesth. 2007; 98:524–30.9. Feierabend RH, Shahram MN. Hoarseness in adults. Am Fam Physician. 2009; 80:363–70.10. Mau T. Diagnostic evaluation and management of hoarseness. Med Clin North Am. 2010; 94:945–60.11. Tasar A, Yanturali S, Topacoglu H, Ersoy G, Unverir P, Sarikaya S. Clinical efficacy of dexamethasone for acute exudative pharyngitis. J Emerg Med. 2008; 35:363–7.12. Quick CA, Merwin GE. Arytenoid dislocation. Arch Otolaryngol. 1978; 104:267–70.13. Rosenthal LH, Benninger MS, Deeb RH. Vocal fold immobility: a longitudinal analysis of etiology over 20 years. Laryngoscope. 2007; 117:1864–70.14. Rudert H. [Uncommon injuries of the larynx following intubation. Recurrent paralysis, torsion and luxation of the cricoarytenoid joints]. HNO. 1984; 32:393–8. German.15. Younes N, Robinson B, Delbridge L. The aetiology, investigation and management of surgical disorders of the thyroid gland. Aust N Z J Surg. 1996; 66:481–90.16. Colton House J, Noordzij JP, Murgia B, Langmore S. Laryngeal injury from prolonged intubation: a prospective analysis of contributing factors. Laryngoscope. 2011; 121:596–600.17. Santos PM, Afrassiabi A, Weymuller EA Jr. Risk factors associated with prolonged intubation and laryngeal injury. Otolaryngol Head Neck Surg. 1994; 111:453–9.18. Weymuller EA Jr. Laryngeal injury from prolonged endotracheal intubation. Laryngoscope. 1988; 98(8 Pt 2 Suppl 45):1–15.19. Gupta J, Varshney S, Bist SS, Bhagat S. Clinico-etiolological study of vocal cord paralysis. Indian J Otolaryngol Head Neck Surg. 2013; 65:16–9.20. Havas T, Lowinger D, Priestley J. Unilateral vocal fold paralysis: causes, options and outcomes. Aust N Z J Surg. 1999; 69:509–13.21. Sulica L. The natural history of idiopathic unilateral vocal fold paralysis: evidence and problems. Laryngoscope. 2008; 118:1303–7.22. Woodson GE, Miller RH. The timing of surgical intervention in vocal cord paralysis. Otolaryngol Head Neck Surg. 1981; 89:264–7.23. Hoffman HT, McCulloch TM. Anatomic considerations in the surgical treatment of unilateral laryngeal paralysis. Head Neck. 1996; 18:174–87.24. Yin SS, Qiu WW, Stucker FJ. Major patterns of laryngeal electromyography and their clinical application. Laryngoscope. 1997; 107:126–36.25. Jung A, Schramm J, Lehnerdt K, Herberhold C. Recurrent laryngeal nerve palsy during anterior cervical spine surgery: a prospective study. J Neurosurg Spine. 2005; 2:123–7.26. Hahn FW Jr, Martin JT, Lillie JC. Vocal-cord paralysis with endotracheal intubation. Arch Otolaryngol. 1970; 92:226–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unilateral Vocal Cord Paralysis Following Endotracheal Intubation - A case report
- A Case of Bilateral Vocal Cord Paralysis Due to Subglottic Pressure Injury after Endotracheal Intubation: A Case Report
- Transient unilateral vocal cord paralysis following endotracheal intubation in elderly patient with the abdominal surgery: A case report
- A case of bilateral vocal cord palsy following short term endotracheal intubation
- Arytenoid Fracture and Vocal Cord Granuloma Resulting from Endotracheal Intubation - 2 cases report