Acute Crit Care.
2020 Feb;35(1):16-23. 10.4266/acc.2019.00675.
Utilization of a rapid response team and associated outcomes in patients with malignancy
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Division of Trauma and Surgical Critical Care, Department of Surgery, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4St. Mary’s Advanced Life Support Team, Department of Nursing, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2500946
- DOI: http://doi.org/10.4266/acc.2019.00675
Abstract
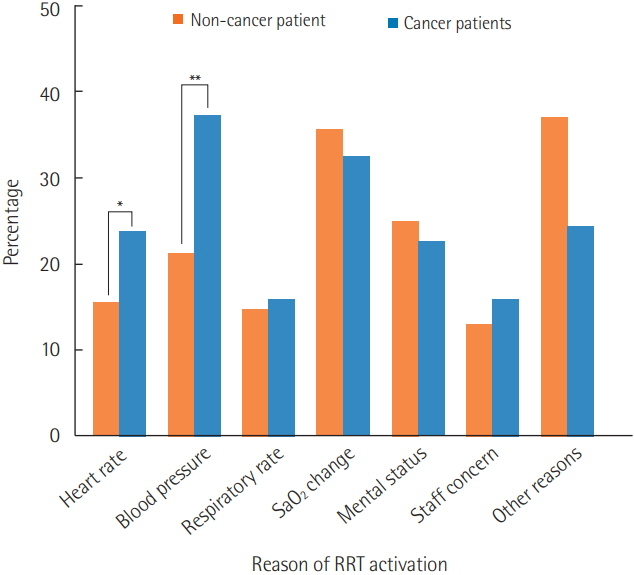
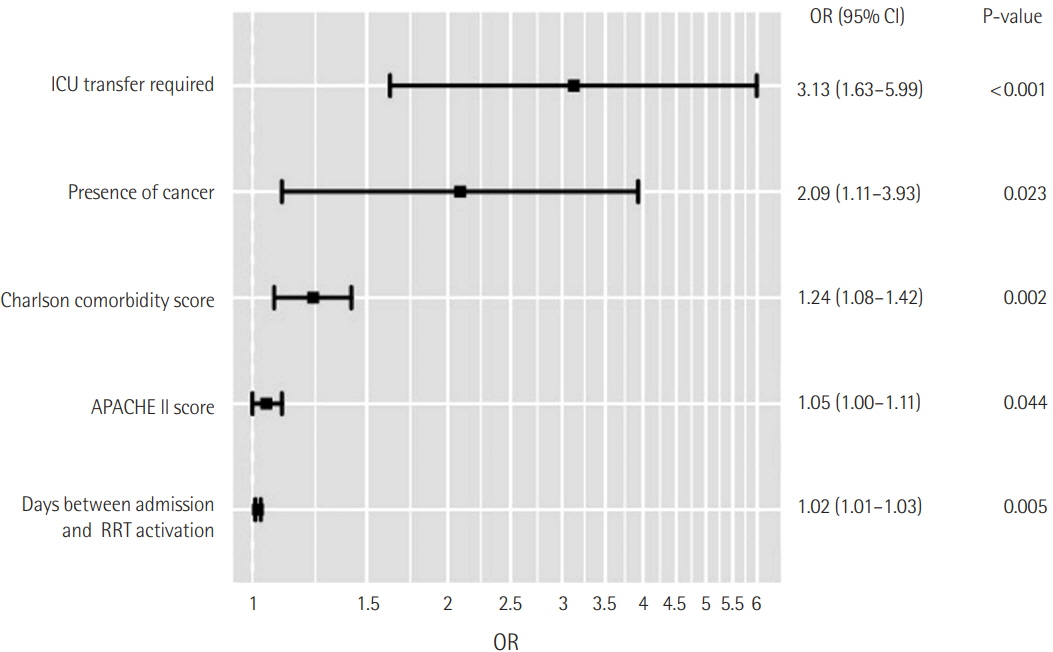
- Background
Recent advances in diagnosis and treatment have improved long-term outcomes in cancer patients. As a result, the requirement for a rapid response team (RRT) for cancer patients is also increasing. This study aimed to analyze utilization of an RRT and the associations between related factors and mortality in a population of cancer patients. Methods: This retrospective cohort study included hospitalized patients at a single academic medical center in Seoul, Korea, who required RRT activation during a 6-year period from June 2013 to December 2018. Results: Overall, 164 of the 457 patients who met the above criteria were cancer patients, and they had a significantly higher Charlson comorbidity score than the non-cancer patients (5.0 vs. 7.0, P<0.001). A significantly larger proportion of cancer patients required intensive care unit transfer (51.8% vs. 41.0%, P=0.032). Cancer patients also had significantly higher in-hospital mortality compared with other patients (39.6% vs. 10.9%, P<0.001). Furthermore, presence of cancer was independently associated with in-hospital mortality (adjusted odds ratio [OR], 2.09; 95% confidence interval [CI], 1.11 to 3.93). Among cancer patients, higher Acute Physiology and Chronic Health Evaluation (APACHE) II at the time of RRT activation was significantly associated with in-hospital mortality regardless of malignancy (adjusted OR, 1.08; 95% CI, 1.01 to 1.15). Conclusions: Cancer patients requiring RRT activation have significantly higher rates of inhospital mortality than patients not using RRT. Higher severity score at the time of RRT activation in patients with malignancy was significantly associated with in-hospital mortality.
Figure
Cited by 1 articles
-
Characteristics and Prognosis of Hospitalized Patients at High Risk of Deterioration Identified by the Rapid Response System: a Multicenter Cohort Study
Sang Hyuk Kim, Ji Young Hong, Youlim Kim
J Korean Med Sci. 2021;36(32):e235. doi: 10.3346/jkms.2021.36.e235.
Reference
-
1. Devita MA, Bellomo R, Hillman K, Kellum J, Rotondi A, Teres D, et al. Findings of the first consensus conference on medical emergency teams. Crit Care Med. 2006; 34:2463–78.
Article2. Bellomo R, Goldsmith D, Uchino S, Buckmaster J, Hart GK, Opdam H, et al. A prospective before-and-after trial of a medical emergency team. Med J Aust. 2003; 179:283–7.
Article3. Chen J, Bellomo R, Flabouris A, Hillman K, Finfer S; MERIT Study Investigators for the Simpson Centre, et al. The relationship between early emergency team calls and serious adverse events. Crit Care Med. 2009; 37:148–53.
Article4. Buist MD, Moore GE, Bernard SA, Waxman BP, Anderson JN, Nguyen TV. Effects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: preliminary study. BMJ. 2002; 324:387–90.
Article5. Jones D, Bellomo R, Bates S, Warrillow S, Goldsmith D, Hart G, et al. Long term effect of a medical emergency team on cardiac arrests in a teaching hospital. Crit Care. 2005; 9:R808–15.6. Maharaj R, Raffaele I, Wendon J. Rapid response systems: a systematic review and meta-analysis. Crit Care. 2015; 19:254.
Article7. Chan PS, Jain R, Nallmothu BK, Berg RA, Sasson C. Rapid response teams: a systematic review and meta-analysis. Arch Intern Med. 2010; 170:18–26.8. Winters BD, Pham JC, Hunt EA, Guallar E, Berenholtz S, Pronovost PJ. Rapid response systems: a systematic review. Crit Care Med. 2007; 35:1238–43.
Article9. Brenner H. Long-term survival rates of cancer patients achieved by the end of the 20th century: a period analysis. Lancet. 2002; 360:1131–5.
Article10. Azoulay E, Soares M, Darmon M, Benoit D, Pastores S, Afessa B. Intensive care of the cancer patient: recent achievements and remaining challenges. Ann Intensive Care. 2011; 1:5.
Article11. Song JU, Suh GY, Park HY, Lim SY, Han SG, Kang YR, et al. Early intervention on the outcomes in critically ill cancer patients admitted to intensive care units. Intensive Care Med. 2012; 38:1505–13.
Article12. Austin CA, Hanzaker C, Stafford R, Mayer C, Culp L, Lin FC, et al. Utilization of rapid response resources and outcomes in a comprehensive cancer center. Crit Care Med. 2014; 42:905–9.
Article13. Jones D, Moran J, Winters B, Welch J. The rapid response system and end-of-life care. Curr Opin Crit Care. 2013; 19:616–23.
Article14. Dargin JM, Mackey CG, Lei Y, Liesching TN. Resource utilization and end-of-life care in a US hospital following medical emergency team-implemented do not resuscitate orders. J Hosp Med. 2014; 9:372–8.
Article15. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40:373–83.
Article16. Lee A, Bishop G, Hillman KM, Daffurn K. The medical emergency team. Anaesth Intensive Care. 1995; 23:183–6.
Article17. Jones D, Warrillow S. Clinical deterioration in cancer patients: the role of the rapid response team. Crit Care Med. 2014; 42:997–8.18. Needham DM, Scales DC, Laupacis A, Pronovost PJ. A systematic review of the Charlson comorbidity index using Canadian administrative databases: a perspective on risk adjustment in critical care research. J Crit Care. 2005; 20:12–9.
Article19. Staudinger T, Stoiser B, Müllner M, Locker GJ, Laczika K, Knapp S, et al. Outcome and prognostic factors in critically ill cancer patients admitted to the intensive care unit. Crit Care Med. 2000; 28:1322–8.
Article20. Taccone FS, Artigas AA, Sprung CL, Moreno R, Sakr Y, Vincent JL. Characteristics and outcomes of cancer patients in European ICUs. Crit Care. 2009; 13:R15.
Article21. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985; 13:818–29.22. Xing X, Gao Y, Wang H, Huang C, Qu S, Zhang H, et al. Performance of three prognostic models in patients with cancer in need of intensive care in a medical center in China. PLoS One. 2015; 10:e0131329.
Article23. Abbott RR, Setter M, Chan S, Choi K. APACHE II: prediction of outcome of 451 ICU oncology admissions in a community hospital. Ann Oncol. 1991; 2:571–4.
Article24. Hillman K, Chen J, Cretikos M, Bellomo R, Brown D, Doig G, et al. Introduction of the medical emergency team (MET) system: a cluster-randomised controlled trial. Lancet. 2005; 365:2091–7.25. Coventry C, Flabouris A, Sundararajan K, Cramey T. Rapid response team calls to patients with a pre-existing not for resuscitation order. Resuscitation. 2013; 84:1035–9.
Article26. Sebat F, Musthafa AA, Johnson D, Kramer AA, Shoffner D, Eliason M, et al. Effect of a rapid response system for patients in shock on time to treatment and mortality during 5 years. Crit Care Med. 2007; 35:2568–75.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of a Rapid Response Team on the Clinical Outcomes of Cardiopulmonary Resuscitation of Patients Hospitalized in General Wards
- Factors Influencing the Activation Time of the Rapid Response Team
- The Same Middle East Respiratory Syndrome-Coronavirus (MERS-CoV) yet Different Outbreak Patterns and Public Health Impacts on the Far East Expert Opinion from the Rapid Response Team of the Republic of Korea
- Experiences and lessons of the disaster medical assistance in Korea
- Rapid response systems in Korea