Korean Circ J.
2020 Jun;50(6):469-475. 10.4070/kcj.2020.0067.
A 2020 Vision of Hypertension
- Affiliations
-
- 1Division of Clinical Pharmacology and Therapeutics, Department of Medicine, The University of Hong Kong, Hong Kong, China
- 2State Key Laboratory of Pharmaceutical Biotechnology, The University of Hong Kong, Hong Kong, China
- 3Institute of Cardiovascular Science and Medicine, The University of Hong Kong, Hong Kong, China
- KMID: 2500914
- DOI: http://doi.org/10.4070/kcj.2020.0067
Abstract
- Hypertension is a common chronic disease affecting a large section of the general population. Hypertension is highly prevalent in the elderly because blood pressure (BP) rises with age. The risk of developing hypertension increases with predisposing genes, intrauterine growth retardation, prematurity and childhood obesity. BP is easier to control in the young. Non-pharmacological treatment through lifestyle changes, such as weight control and leisure-time physical activity, is more likely to be successful in young people. Hypertension in older adults is more difficult to control, requiring the use of more than one antihypertensive drug. Adverse effects and compliance become problematic. Much research is now directed at novel ways of controlling BP such as denervation. The change in definition of hypertension in the American guideline highlights the need to identify and manage hypertension early, at a stage when it is potentially reversible.
Keyword
Figure
Cited by 3 articles
-
Suboptimal Management Status of Younger Hypertensive Population in Korea
Hae-Young Lee, Gyu Chul Oh, Il Suk Sohn, Sungha Park, Jinho Shin, Wook Bum Pyun, Myeong-Chan Cho
Korean Circ J. 2021;51(7):598-606. doi: 10.4070/kcj.2020.0542.Reimbursement of Digital Therapeutics: Future Perspectives in Korea
Jin Han Ju, Boram Sim, Jeongeun Lee, Jin Yong Lee
Korean Circ J. 2022;52(4):265-279. doi: 10.4070/kcj.2022.0014.On-Treatment Diastolic Blood Pressure: When Is It Too High?
Jin Joo Park
Korean Circ J. 2022;52(6):475-477. doi: 10.4070/kcj.2022.0126.
Reference
-
1. Centers for Disease Control and Prevention. Hypertension [Internet]. Atlanta (GA): Centers for Disease Control and Prevention;2018. cited 2020 Feb 18. Available from: https://www.cdc.gov/nchs/fastats/hypertension.htm.2. Wang Z, Chen Z, Zhang L, et al. Status of hypertension in China: results from the China hypertension survey, 2012–2015. Circulation. 2018; 137:2344–2356. PMID: 29449338.3. Cheung BM, Ong KL. The challenge of managing hypertension. In : Finkel ML, editor. Public Health in the 21st Century. Vol. 1. Santa Barbara (CA): Praeger Publishing;2011. p. 117–128.4. Kim HC, Ihm SH, Kim GH, et al. 2018 Korean Society of Hypertension guidelines for the management of hypertension: part I-epidemiology of hypertension. Clin Hypertens. 2019; 25:16. PMID: 31388451.
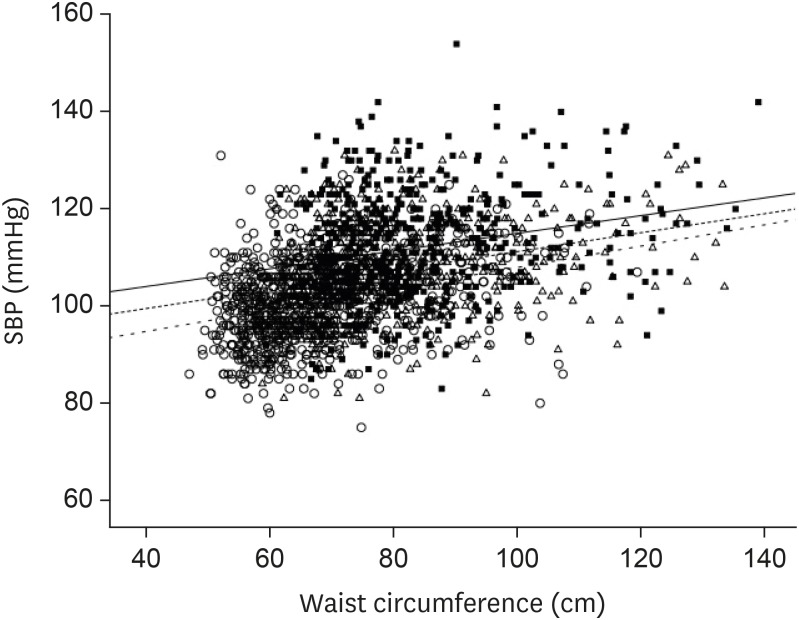
Article5. Cheung BM, Wat NM, Man YB, et al. Relationship between the metabolic syndrome and the development of hypertension in the Hong Kong cardiovascular risk factor prevalence study-2 (CRISPS2). Am J Hypertens. 2008; 21:17–22. PMID: 18091739.
Article6. Cheung BM, Wat NM, Tam S, et al. Components of the metabolic syndrome predictive of its development: a 6-year longitudinal study in Hong Kong Chinese. Clin Endocrinol (Oxf). 2008; 68:730–737. PMID: 17980012.
Article7. Cheung BM, Wat NM, Tso AW, et al. Association between raised blood pressure and dysglycemia in Hong Kong Chinese. Diabetes Care. 2008; 31:1889–1891. PMID: 18556342.
Article8. Janus ED. Epidemiology of cardiovascular risk factors in Hong Kong. Clin Exp Pharmacol Physiol. 1997; 24:987–988. PMID: 9406673.
Article9. Ong KL, Tso AW, Lam KS, Cheung BM. Gender difference in blood pressure control and cardiovascular risk factors in Americans with diagnosed hypertension. Hypertension. 2008; 51:1142–1148. PMID: 18259031.
Article10. Wilber JA, Barrow JG. Hypertension--a community problem. Am J Med. 1972; 52:653–663. PMID: 5027555.
Article11. Kotseva K, Wood D, De Bacquer D, et al. EUROASPIRE IV: a European Society of Cardiology survey on the lifestyle, risk factor and therapeutic management of coronary patients from 24 European countries. Eur J Prev Cardiol. 2016; 23:636–648. PMID: 25687109.12. Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018; 39:3021–3104. PMID: 30165516.13. Bhatt DL, Kandzari DE, O'Neill WW, et al. A controlled trial of renal denervation for resistant hypertension. N Engl J Med. 2014; 370:1393–1401. PMID: 24678939.
Article14. Zhen Z, Liao SY, Zhu ZY, et al. Catheter-based splanchnic denervation for treatment of hypertensive cardiomyopathy. Hypertension. 2019; 74:47–55. PMID: 31132949.
Article15. Lobo MD, Ott C, Sobotka PA, et al. Central iliac arteriovenous anastomosis for uncontrolled hypertension: one-year results from the ROX CONTROL HTN trial. Hypertension. 2017; 70:1099–1105. PMID: 29061728.16. Nakagami H, Morishita R. Recent advances in therapeutic vaccines to treat hypertension. Hypertension. 2018; 72:1031–1036. PMID: 30354822.
Article17. Phillips MI. Gene therapy for hypertension: the preclinical data. Hypertension. 2001; 38:543–548. PMID: 11566928.18. Warren HR, Evangelou E, Cabrera CP, et al. Genome-wide association analysis identifies novel blood pressure loci and offers biological insights into cardiovascular risk. Nat Genet. 2017; 49:403–415. PMID: 28135244.19. Calkins K, Devaskar SU. Fetal origins of adult disease. Curr Probl Pediatr Adolesc Health Care. 2011; 41:158–176. PMID: 21684471.
Article20. Parkinson JR, Hyde MJ, Gale C, Santhakumaran S, Modi N. Preterm birth and the metabolic syndrome in adult life: a systematic review and meta-analysis. Pediatrics. 2013; 131:e1240–63. PMID: 23509172.
Article21. Cheung BM. Hypertension: a weighty problem in children. Postgrad Med J. 2017; 93:647. PMID: 28823997.
Article22. Cheung AJ, Cheung BMY. Association of increased systolic blood pressure in children with obesity and the metabolic syndrome. J Hum Hypertens. 2015; 29(Suppl1):S15.23. Ong KL, Cheung BM, Man YB, Lau CP, Lam KS. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007; 49:69–75. PMID: 17159087.
Article24. Muntner P, Carey RM, Gidding S, et al. Potential U.S. population impact of the 2017 ACC/AHA high blood pressure guideline. J Am Coll Cardiol. 2018; 71:109–118. PMID: 29146532.
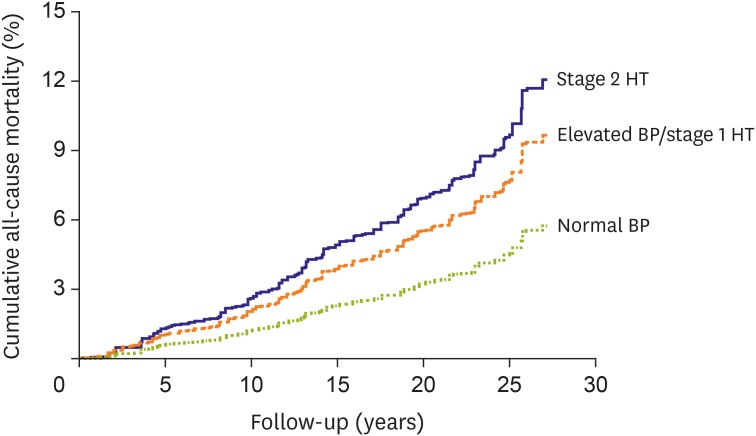
Article25. Son JS, Choi S, Kim K, et al. Association of blood pressure classification in Korean young adults according to the 2017 American College of Cardiology/American Heart Association guidelines with subsequent cardiovascular disease events. JAMA. 2018; 320:1783–1792. PMID: 30398603.
Article26. Yano Y, Reis JP, Colangelo LA, et al. Association of blood pressure classification in young adults using the 2017 American College of Cardiology/American Heart Association blood pressure guideline with cardiovascular events later in life. JAMA. 2018; 320:1774–1782. PMID: 30398601.
Article27. Or B, Tsoi MF, Cheung TT, Cheung BM. Decreased survival in young adults with stage 1 and 2 hypertension in the National Health and Nutrition Examination Survey III. Hong Kong Med J. 2020; 26(Suppl 1):14.28. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension. 2018; 71:1269–1324. PMID: 29133354.
Article29. SPRINT Research Group, Wright JT Jr, Williamson JD, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015; 373:2103–2116. PMID: 26551272.
Article30. Fei Y, Tsoi MF, Cheung BM. Determining the optimal systolic blood pressure for hypertensive patients: a network meta-analysis. Can J Cardiol. 2018; 34:1581–1589. PMID: 30414702.
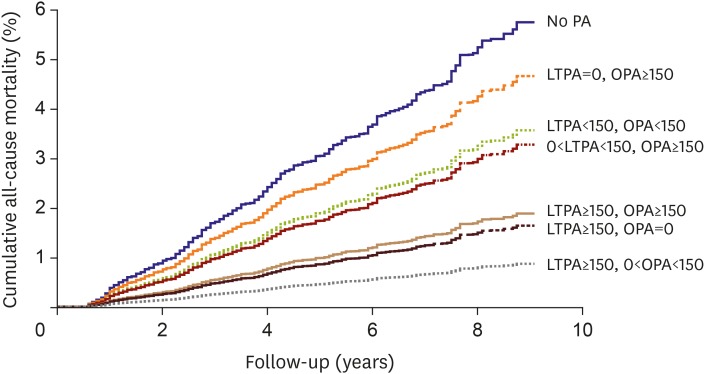
Article31. Tsoi MF, Fei Y, Cheung TT, Cheung BM. Characteristics of Americans with stage-1 hypertension: United States National Health Nutrition and Examination Survey 2011–2016. Hong Kong Med J. 2018; 24(Suppl 1):54.32. Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014; 384:766–781. PMID: 24880830.33. Or B, Tsoi MF, Cheung TT, Cheung BM. Leisure time, occupational aerobic physical activity, and mortality risk in adults of United States: National Health and Nutrition Examination Survey 2007–2016. Hong Kong Med J. 2020; 26(Suppl 1):13.34. Ludwig DS. The glycemic index: physiological mechanisms relating to obesity, diabetes, and cardiovascular disease. JAMA. 2002; 287:2414–2423. PMID: 11988062.35. Chan HM, Brand-Miller JC, Holt SH, Wilson D, Rozman M, Petocz P. The glycaemic index values of Vietnamese foods. Eur J Clin Nutr. 2001; 55:1076–1083. PMID: 11781674.
Article36. Cheung BM. The cardiovascular continuum in Asia--a new paradigm for the metabolic syndrome. J Cardiovasc Pharmacol. 2005; 46:125–129. PMID: 16044022.
Article37. National Heart, Lung, and Blood Institute (US). The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Bethesda (MD): National Heart, Lung, and Blood Institute;2004.38. Vest AR, Heneghan HM, Agarwal S, Schauer PR, Young JB. Bariatric surgery and cardiovascular outcomes: a systematic review. Heart. 2012; 98:1763–1777. PMID: 23077152.
Article39. Sharma AM, Golay A. Effect of orlistat-induced weight loss on blood pressure and heart rate in obese patients with hypertension. J Hypertens. 2002; 20:1873–1878. PMID: 12195131.
Article40. Wang B, Zhong J, Lin H, et al. Blood pressure-lowering effects of GLP-1 receptor agonists exenatide and liraglutide: a meta-analysis of clinical trials. Diabetes Obes Metab. 2013; 15:737–749. PMID: 23433305.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary Spinal Cord Astrocytoma Presenting as Intracranial Hypertension: A Case Report
- Clinical Analysis of 100 Low Vision Patients
- Clinical Effect of Low Vision Aids
- Quality of Life Assessment in Patients with Wet Age-Related Macular Degeneration
- Clinical Experience on the Visual Rehabilitation of Low Vision Patients