J Korean Med Sci.
2020 May;35(20):e158. 10.3346/jkms.2020.35.e158.
Who Are the People Willing to Pay for Physician Home Visits?
- Affiliations
-
- 1Institute of Social Welfare, Sungkonghoe University, Seoul, Korea
- 2Visiting Doctors Program of Medical Home, Seoul, Korea
- 3Red Cross College of Nursing, Chung-Ang University, Seoul, Korea
- KMID: 2500846
- DOI: http://doi.org/10.3346/jkms.2020.35.e158
Abstract
- Background
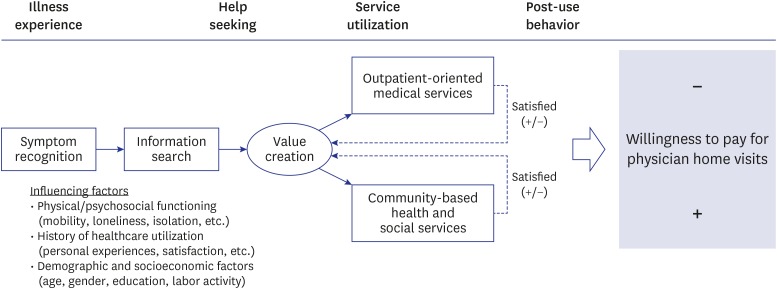
Since the recently announced Community Care Policy, there has been an opinion that Korea needs to establish an alternative medical model such as physician home visits. This study aimed to assess the need and willingness to pay (WTP) for physician home visits among the community-dwelling Korean older population and to determine the most important factors that influence older adults to decide to use a physician home visit service.
Methods
A total of 797 people aged 60 years or older who were randomly selected from a nationwide dataset using a multi-stage stratified sampling method answered a questionnaire on the need and WTP for physician home visits.
Results
A total of 39.3% of participants reported that they would like a physician home visit when they need help. Among older adults who needed physician home visits (n = 313), the WTP amount for physician home visits was 21,982 ± 17,546 KRW. Logit and Tobit regression analyses showed that the higher valuated need and WTP for physician home visits was associated with a lower level of physical/psychosocial functioning measured by EuroQol-five dimensions score (odds ratio [OR], 1.13; 95% confidence interval [CI], 1.01–1.27; P = 0.035) and a higher level of satisfaction when using community-based services such as public health centers (OR, 1.32; 95% CI, 1.02–1.72; P = 0.034), social welfare centers and Gyeong-ro-dang (OR, 1.61; 95% CI, 1.04–2.50; P = 0.033; β = 8.39; standard error, 3.63; P = 0.021).
Conclusion
This study provides evidence that the decision to pay for a physician home visit service is based upon the complex interactions among an individual's physical and psychosocial functioning, personal experiences of service utilization, and demographic factors. The value for physician home visits should be qualified based on the empirical data of WTP, which comes from a consumer-centered perspective.
Keyword
Figure
Reference
-
1. Rich EC, Lipson D, Libersky J, Peikes DN, Parchman ML. Organizing care for complex patients in the patient-centered medical home. Ann Fam Med. 2012; 10(1):60–62. PMID: 22230832.
Article2. Epstein RM, Street RL Jr. The values and value of patient-centered care. Ann Fam Med. 2011; 9(2):100–103. PMID: 21403134.
Article3. Arend J, Tsang-Quinn J, Levine C, Thomas D. The patient-centered medical home: history, components, and review of the evidence. Mt Sinai J Med. 2012; 79(4):433–450. PMID: 22786733.
Article4. Fletcher AE, Price GM, Ng ES, Stirling SL, Bulpitt CJ, Breeze E, et al. Population-based multidimensional assessment of older people in UK general practice: a cluster-randomised factorial trial. Lancet. 2004; 364(9446):1667–1677. PMID: 15530627.
Article5. Huss A, Stuck AE, Rubenstein LZ, Egger M, Clough-Gorr KM. Multidimensional preventive home visit programs for community-dwelling older adults: a systematic review and meta-analysis of randomized controlled trials. J Gerontol A Biol Sci Med Sci. 2008; 63(3):298–307. PMID: 18375879.6. Phelan EA, Williams B, Penninx BW, LoGerfo JP, Leveille SG. Activities of daily living function and disability in older adults in a randomized trial of the health enhancement program. J Gerontol A Biol Sci Med Sci. 2004; 59(8):838–843. PMID: 15345735.
Article7. Gill TM, Baker DI, Gottschalk M, Gahbauer EA, Charpentier PA, de Regt PT, et al. A prehabilitation program for physically frail community-living older persons. Arch Phys Med Rehabil. 2003; 84(3):394–404. PMID: 12638108.
Article8. Szanton SL, Xue QL, Leff B, Guralnik J, Wolff JL, Tanner EK, et al. Effect of a biobehavioral environmental approach on disability among low-income older adults: a randomized clinical trial. JAMA Intern Med. 2019; 179(2):204–211. PMID: 30615024.9. Bouman A, van Rossum E, Nelemans P, Kempen GI, Knipschild P. Effects of intensive home visiting programs for older people with poor health status: a systematic review. BMC Health Serv Res. 2008; 8(1):74. PMID: 18387184.
Article10. Stuck A, Kane RL. Whom do preventive home visits help? J Am Geriatr Soc. 2008; 56(3):561–563. PMID: 18179507.
Article11. Stuck AE, Aronow HU, Steiner A, Alessi CA, Büla CJ, Gold MN, et al. A trial of annual in-home comprehensive geriatric assessments for elderly people living in the community. N Engl J Med. 1995; 333(18):1184–1189. PMID: 7565974.
Article12. Naylor MD, Brooten D, Campbell R, Jacobsen BS, Mezey MD, Pauly MV, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. JAMA. 1999; 281(7):613–620. PMID: 10029122.13. Yoon JL, Jung S, Seo Kh, Lim JY, Kim SW, Kim ES. Development of Post-acute Transitional Care System for Frail Older Persons. Chuncheon: Hallym University;2017.14. Kim CO, Lee KR. Preventive effect of protein-energy supplementation on the functional decline of frail older adults with low socioeconomic status: a community-based randomized controlled study. J Gerontol A Biol Sci Med Sci. 2013; 68(3):309–316. PMID: 22879453.
Article15. Kim CO, Jang SN. Home-based primary care for homebound older adults: literature review. Ann Geriatr Med Res. 2018; 22(2):62–72.
Article16. Kim CO. Time to conduct community-oriented researches in geriatrics. Ann Geriatr Med Res. 2018; 22(23):109–110.
Article17. Lee K. Health care perspectives on community care. J Korean Med Assoc. 2018; 61(10):586–589.
Article18. Vargo SL, Lusch RF. The four service marketing myths: remnants of a goods-based, manufacturing model. J Serv Res. 2004; 6(4):324–335.19. Park JS. The causal relationship of health service quality, satisfaction, intention to revisit and intention to recommend perceived by health center visitors. Health Policy Manag. 2005; 15(3):60–78.20. Reuben DB. Better ways to care for older persons: is anybody listening? J Am Geriatr Soc. 2009; 57(12):2348–2349. PMID: 20121994.
Article21. Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press;2015.22. Tobin J. Estimation of relationships for limited dependent variables. Econometrica. 1958; 26(1):24–36.
Article23. Lee JK, Jang SN. Place of death and associated gender difference in Korea 2006-2014: Evidence from exit interviews of the Korean Longitudinal Study of Ageing. Arch Gerontol Geriatr. 2018; 78(1):196–202. PMID: 30006212.
Article24. Stuck AE, Egger M, Hammer A, Minder CE, Beck JC. Home visits to prevent nursing home admission and functional decline in elderly people: systematic review and meta-regression analysis. JAMA. 2002; 287(8):1022–1028. PMID: 11866651.25. Totten AM, White-Chu EF, Wasson N, Morgan E, Kansagara D, Davis-O'Reilly C, et al. Home-based Primary Care Interventions. AHRQ Publication No. 15(16)-EHC036-EF. Rockville, MD: Agency for Healthcare Research and Quality;2016.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Home Visits in an Office Practice in Seoul
- Demand and willing to pay for oral hygiene service in long-term care insurance of elderly
- Lived Experiences of Nursing Home Residents in Korea
- Impact of increasing the level of copayments on the number of physician visits
- Development and Effects of Head-Mounted Display-Based Home-Visits Virtual Reality Simulation Program for Nursing Students