J Korean Med Sci.
2020 May;35(20):e134. 10.3346/jkms.2020.35.e134.
Syncope after Influenza Virus Infection
- Affiliations
-
- 1Department of Neurology, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea
- 2Department of Neurology, Jeonbuk National University Hospital, Jeonju, Korea
- 3Department of Neurology, Asan Medical Center, University of Ulsan, College of Medicine Seoul, Korea
- KMID: 2500844
- DOI: http://doi.org/10.3346/jkms.2020.35.e134
Abstract
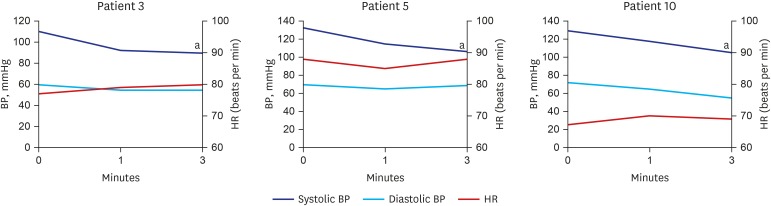
- Influenza is an epidemical acute respiratory disease caused by viral infection. Several complications in the respiratory tract, such as pneumonia can occur. However, rare but serious neurological complications are also observed. Here, we described the prevalence, characteristics and suggestive pathomechanism of syncope after influenza infection season. Of 2.2% of patients diagnosed as influenza experienced syncope. None of the patients had severe cough, low blood pressure (BP) or dehydration. Patients suffered with frequent dizziness before syncope. Patient with long duration of loss of consciousness was more observed in those with high fever or positive orthostatic BP drop.
Keyword
Figure
Reference
-
1. Morishima T, Togashi T, Yokota S, Okuno Y, Miyazaki C, Tashiro M, et al. Encephalitis and encephalopathy associated with an influenza epidemic in Japan. Clin Infect Dis. 2002; 35(5):512–517. PMID: 12173123.
Article2. Maricich SM, Neul JL, Lotze TE, Cazacu AC, Uyeki TM, Demmler GJ, et al. Neurologic complications associated with influenza A in children during the 2003–2004 influenza season in Houston, Texas. Pediatrics. 2004; 114(5):e626–33. PMID: 15520093.
Article3. Lee YJ, Hwang SK, Kwon S. Acute necrotizing encephalopathy in children: a long way to go. J Korean Med Sci. 2019; 34(19):e143. PMID: 31099193.
Article4. Hooper L, Abdelhamid A, Attreed NJ, Campbell WW, Channell AM, Chassagne P, et al. Clinical symptoms, signs and tests for identification of impending and current water-loss dehydration in older people. Cochrane Database Syst Rev. 2015; (4):CD009647. PMID: 25924806.
Article5. Koski CL. Guillain-Barré syndrome and chronic inflammatory demyelinating polyneuropathy: pathogenesis and treatment. Semin Neurol. 1994; 14(2):123–130. PMID: 7984827.
Article6. Koski CL. Humoral mechanisms in immune neuropathies. Neurol Clin. 1992; 10(3):629–649. PMID: 1501599.
Article7. Ludlow M, Kortekaas J, Herden C, Hoffmann B, Tappe D, Trebst C, et al. Neurotropic virus infections as the cause of immediate and delayed neuropathology. Acta Neuropathol. 2016; 131(2):159–184. PMID: 26659576.
Article8. Bradshaw MJ, Venkatesan A. Herpes simplex virus-1 encephalitis in adults: pathophysiology, diagnosis, and management. Neurotherapeutics. 2016; 13(3):493–508. PMID: 27106239.
Article9. Sen N, Tanwar S. H1N1 positive case represent as cardiogenic syncope in cardiac emergency department. Int J Sci Res. 2016; 5(4):524–525.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Benign Acute Childhood Myositis Associated with Influenza B Virus
- Prevention and Treatment of Influenza
- Atypical Kawasaki Disease Presenting as Acute Kidney Injury in a Patient with Influenza B Virus Infection
- Influenza Associated Pneumonia
- Reversible Splenial Lesion in a Patient with Influenza B Virus Infection