Ann Hepatobiliary Pancreat Surg.
2020 May;24(2):198-202. 10.14701/ahbps.2020.24.2.198.
Living donor liver retransplantation for primary non-function of liver graft following multivisceral transplantation in a pediatric patient
- Affiliations
-
- 1Division of Hepatobiliary Surgery and Liver Transplantation, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine
- 2Division of Pediatric Surgery, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine
- 3Department of Pediatrics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2500806
- DOI: http://doi.org/10.14701/ahbps.2020.24.2.198
Abstract
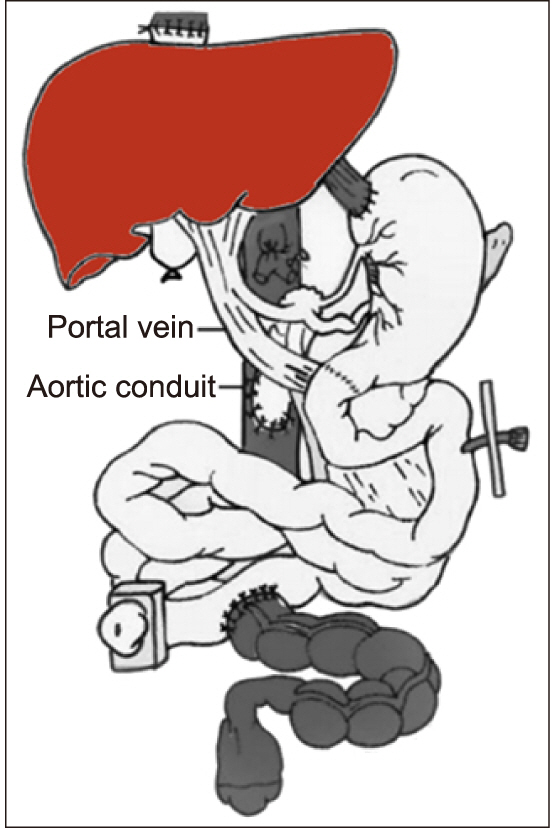
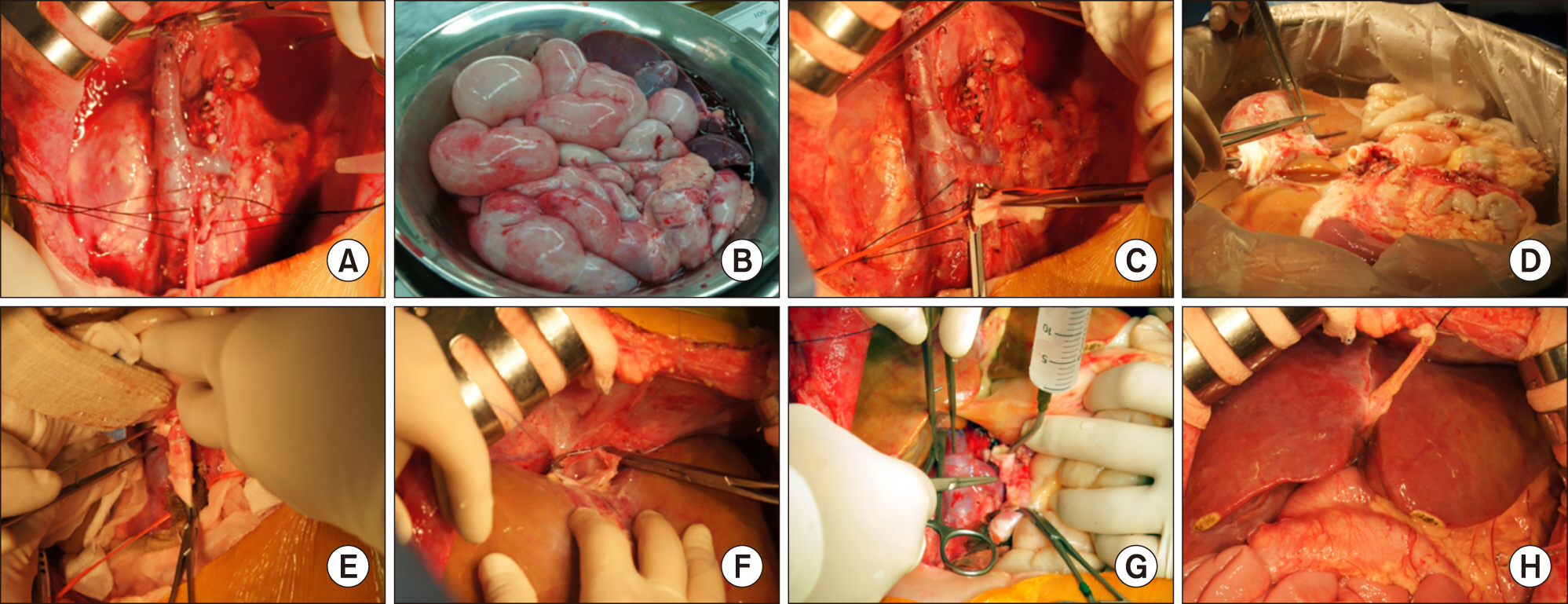
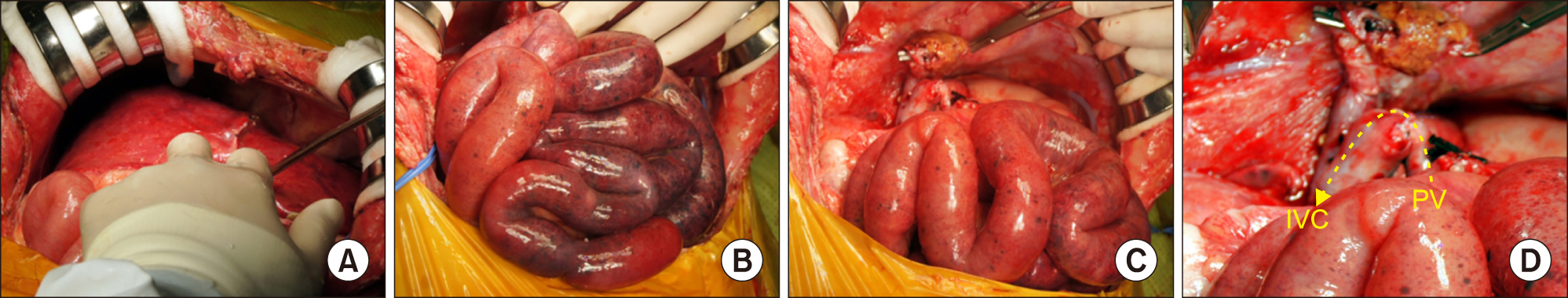
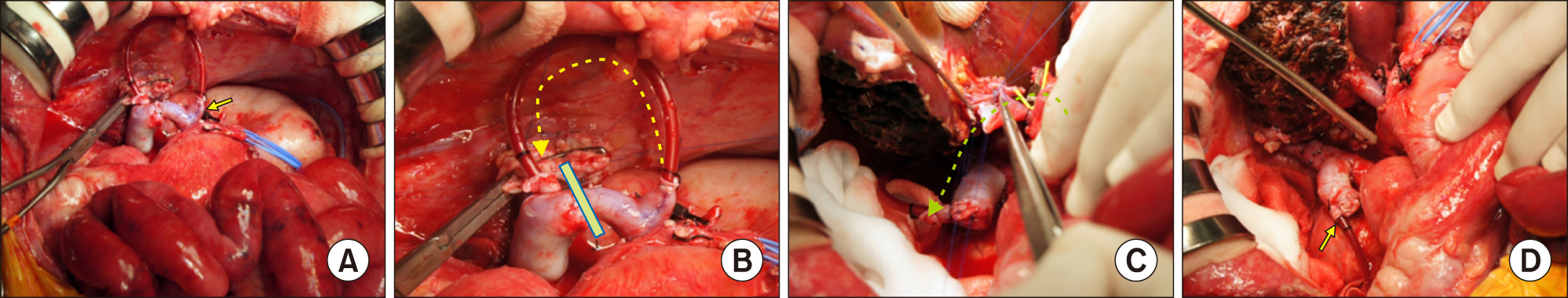
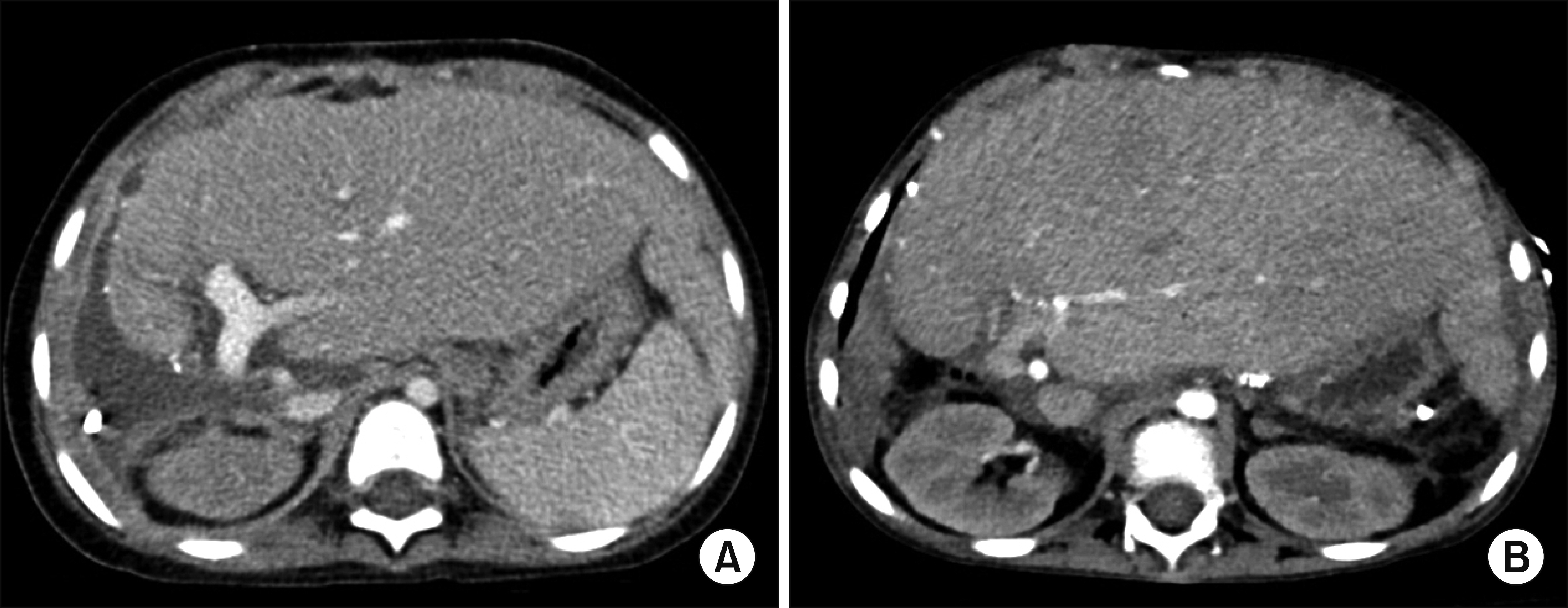
- Multivisceral organ transplantation (MVOT) includes transplantation of three or more abdominal organs, generally including the small bowel, duodenum, stomach, liver, pancreas, and colon. We here presented the detailed procedures of repeat living donor liver transplantation for primary non-function of the first liver graft following MVOT in a pediatric patient. A 6-year-old girl with chronic intestinal pseudo-obstruction underwent MVOT with 5-year-old donor organs. However, the primary non-function of the liver graft developed, and an emergency living donor liver transplantation operation using a left lateral section graft was performed on the third day after MVOT. The donor was the patient’s father. Portal flow interruption induced ischemic congestion of the whole small bowel, thus we used a series of porto- caval shunt to reduce the risk of ischemic splanchnic congestion during recipient hepatectomy and graft implantation. Other surgical procedures were the same as the standardized procedures for left liver graft implantation. The graft-recipient weight ratio was 2.15. The patient was managed conservatively for 3 months and discharged in an improved condition at 4 months after MVOT. She finally passed away at 22 months after MVOT. We think that our experience will be helpful for surgeons to cope with portal vein clamping-associated splanchnic congestion during liver transplantation and other abdominal surgeries.
Keyword
Figure
Cited by 2 articles
-
Korea-nationwide incidence of pediatric deceased donors and single-institutional status of liver transplantation using pediatric donor liver grafts
Jung-Man Namgung, Shin Hwang, Chul-Soo Ahn, Ki-Hun Kim, Deok-Bog Moon, Tae-Yong Ha, Gi-Won Song, Dong-Hwan Jung, Gil-Chun Park, Dea-Yeon Kim, Kyung Mo Kim, Seak Hee Oh, Sung-Gyu Lee
Korean J Transplant. 2020;34(3):178-184. doi: 10.4285/kjt.2020.34.3.178.Pediatric liver transplantation using a hepatitis B surface antigen-positive donor liver graft for congenital absence of the portal vein
Jung-Man Namgoong, Shin Hwang, Dae-Yeon Kim, Tae-Yong Ha, Gi-Won Song, Dong-Hwan Jung, Kyung Mo Kim, Seak Hee Oh
Korean J Transplant. 2021;35(1):59-65. doi: 10.4285/kjt.20.0038.
Reference
-
1. Spechtenhauser B, Königsraner A, Steurer W, Riedmann B, Pomarolli A, Hörmann C, et al. 1999; Multivisceral transplantation. Transplant Proc. 31:3175–3176. DOI: 10.1016/S0041-1345(99)00775-7.
Article2. Loinaz C, Mittal N, Kato T, Miller B, Rodriguez M, Tzakis A. 2004; Multivisceral transplantation for pediatric intestinal pseudo-obstruction: single center's experience of 16 cases. Transplant Proc. 36:312–313. DOI: 10.1016/j.transproceed.2004.01.084. PMID: 15050142.
Article3. Abu-Elmagd KM, Costa G, Bond GJ, Soltys K, Sindhi R, Wu T, et al. 2009; Five hundred intestinal and multivisceral transplantations at a single center: major advances with new challenges. Ann Surg. 250:567–581. DOI: 10.1097/SLA.0b013e3181b67725. PMID: 19730240.4. Park YS, Oh JY, Hwang BY, Moon Y, Lee HM, Hwang GS. 2014; Prolonged post-reperfusion syndrome during multivisceral organ transplantation in a pediatric patient: a case report. Korean J Anesthesiol. 66:467–471. DOI: 10.4097/kjae.2014.66.6.467. PMID: 25006372. PMCID: PMC4085269.
Article5. Moon DB, Lee SG, Hwang S, Kim KH, Ahn CS, Ha TY, et al. 2013; More than 300 consecutive living donor liver transplants a year at a single center. Transplant Proc. 45:1942–1947. DOI: 10.1016/j.transproceed.2013.02.041. PMID: 23769079.
Article6. Moon DB, Lee SG, Hwang S, Kim KH, Ahn CS, Ha TY, et al. 2013; Toward more than 400 liver transplantations a year at a single center. Transplant Proc. 45:1937–1941. DOI: 10.1016/j.transproceed.2012.12.015. PMID: 23769078.
Article7. Cai J. 2009; Intestine and multivisceral transplantation in the United States: a report of 20-year national registry data (1990-2009). Clin Transpl. 83–101. PMID: 20524278.8. Namgoong JM, Hwang S, Oh SH, Kim KM, Park GC, Ahn CS, et al. 2020; Living donor liver transplantation with total pancreatectomy and portal vein homograft replacement in a pediatric patient with advanced pancreatoblastoma. Ann Hepatobiliary Pancreat Surg. 24:78–84. DOI: 10.14701/ahbps.2020.24.1.78. PMID: 32181434. PMCID: PMC7061052.
Article9. Chang HK, Kim SY, Kim JI, Kim SI, Whang JK, Choi JY, et al. 2016; Ten-year experience with bowel transplantation at Seoul St. Mary's Hospital. Transplant Proc. 48:473–478. DOI: 10.1016/j.transproceed.2015.12.065. PMID: 27109981.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Liver retransplantation for adult recipients
- Living donor liver transplantation-associated retransplantation in adult patients
- Left at right heterotopic implantation of left liver graft in adult-to-adult living donor liver transplantation: the technical concern for decision-making
- Prolonged post-reperfusion syndrome during multivisceral organ transplantation in a pediatric patient: a case report
- Pediatric liver transplantation in Korea: long-term outcomes and allocations