J Korean Med Sci.
2020 Apr;35(19):e119. 10.3346/jkms.2020.35.e119.
Pregnancy and Epilepsy: a Korean Tertiary Epilepsy Center Review
- Affiliations
-
- 1Department of Neurology, Kyungpook National University Chilgok Hospital, School of Medicine, Kyungpook National University, Daegu, Korea
- 2Department of Obstetrics and Gynecology, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea
- 3Department of Neurology, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea
- KMID: 2500627
- DOI: http://doi.org/10.3346/jkms.2020.35.e119
Abstract
- Background
Pregnancy in women with epilepsy (WWE) is known to have a higher risk for fetal development complications, which may include congenital malformations. Unfortunately, information pertaining to pregnancy in WWE is difficult to obtain because there are considerable ethical issues preventing these studies from being conducted on pregnant women. Therefore, this study investigated the pregnancies of Korean WWE in a tertiary epilepsy center to observe data resulting from the outcome of the pregnancies.
Methods
This was a retrospective study of 48 pregnant WWE who were treated at the regional tertiary epilepsy center. All records of hospital visits before and after the period of pregnancy were analyzed to obtain information about the seizures as well as pregnancy-related outcomes, including the status of the newborns' conditions.
Results
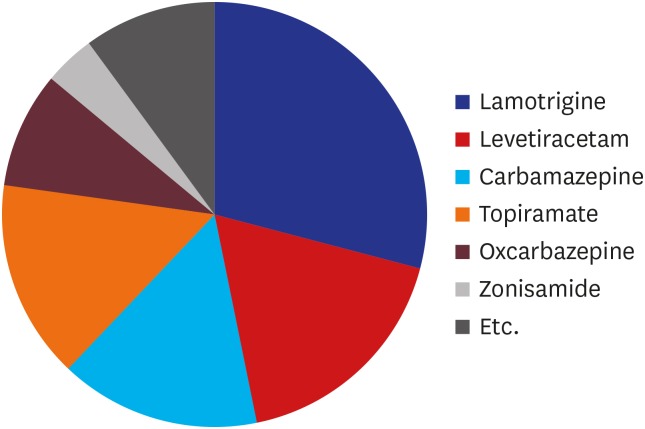
The subject group consisted of 31 (63.3%) with partial epilepsy, 6 (12.5%) with generalized epilepsy, and 11 (22.9%) with unclassified epilepsy. There were 27 subjects who took one antiepileptic drug (AED), and 12 who took two AEDs. The most commonly used drug was lamotrigine (29.8%). Of the 48 WWE involved in the study, 31 underwent caesarian sections and 17 opted for natural birth. Thirty-nine (81.3%) delivered at full-term, but 9 (18.7%) delivered at preterm. Compared to full-term infants, pre-mature infants showed lower birth weight, smaller head circumference, shorter height, and lower 1-minute Apgar scores, but seizure frequencies of the mothers did not differ.
Conclusion
In WWE, epilepsy classification, number of AEDs taken, and frequency of seizures are not significantly correlated with delivery and fetal condition. This data could be used as a clinical reference for physicians to provide useful information to WWE if they are concerned about their pregnancies.
Keyword
Figure
Reference
-
1. Barrett C, Richens A. Epilepsy and pregnancy: report of an Epilepsy Research Foundation Workshop. Epilepsy Res. 2003; 52(3):147–187. PMID: 12536051.
Article2. Battino D, Tomson T, Bonizzoni E, Craig J, Lindhout D, Sabers A, et al. Seizure control and treatment changes in pregnancy: observations from the EURAP epilepsy pregnancy registry. Epilepsia. 2013; 54(9):1621–1627. PMID: 23848605.
Article3. Vélez-Ruiz NJ, Pennell PB. Issues for women with epilepsy. Neurol Clin. 2016; 34(2):411–425. PMID: 27086987.
Article4. He S, Zhu H, Qiu X, Zhu X, Peng A, Duan J, et al. Pregnancy outcome in women with epilepsy in Western China: a prospective hospital based study. Epilepsy Behav. 2017; 74:10–14. PMID: 28666184.
Article5. Kim HY, Moon CS. Integrated care center for high risk pregnancy and neonate - an analysis of process and problems in obstetrics. Korean J Perinatol. 2014; 25(3):140–152.6. Hernández-Díaz S, Smith CR, Shen A, Mittendorf R, Hauser WA, Yerby M, et al. Comparative safety of antiepileptic drugs during pregnancy. Neurology. 2012; 78(21):1692–1699. PMID: 22551726.
Article7. Stephen LJ, Harden C, Tomson T, Brodie MJ. Management of epilepsy in women. Lancet Neurol. 2019; 18(5):481–491. PMID: 30857949.
Article8. Menon S, Siewe Fodjo JN, Weckhuysen S, Bhwana D, Njamnshi AK, Dekker M, et al. Women with epilepsy in sub-Saharan Africa: a review of the reproductive health challenges and perspectives for management. Seizure. 2019; 71:312–317. PMID: 31521949.
Article9. Bardy AH. Incidence of seizures during pregnancy, labor and puerperium in epileptic women: a prospective study. Acta Neurol Scand. 1987; 75(5):356–360. PMID: 3618113.
Article10. Gjerde IO, Strandjord RE, Ulstein M. The course of epilepsy during pregnancy: a study of 78 cases. Acta Neurol Scand. 1988; 78(3):198–205. PMID: 3147566.
Article11. Crump C, Sundquist K, Winkleby MA, Sundquist J. Preterm birth and risk of epilepsy in Swedish adults. Neurology. 2011; 77(14):1376–1382. PMID: 21968843.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary Reading Epilepsy: A Case Report
- Magnetoencephalography in Epilepsy
- Malformations of Cortical Decelopment and Epilepsy
- Sleep and Epilepsy in Clinical Practice "fears, regas, deliria, leaps out of bed and seizures during the night" - Hippocrates
- The Latest Classification of Epilepsy and Clinical Significance of Electroencephalography