Anesth Pain Med.
2020 Jan;15(1):83-87. 10.17085/apm.2020.15.1.83.
Decreased analgesic requirement in recipient of liver transplantation from monozygotic twin - A case report -
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2500460
- DOI: http://doi.org/10.17085/apm.2020.15.1.83
Abstract
- Background
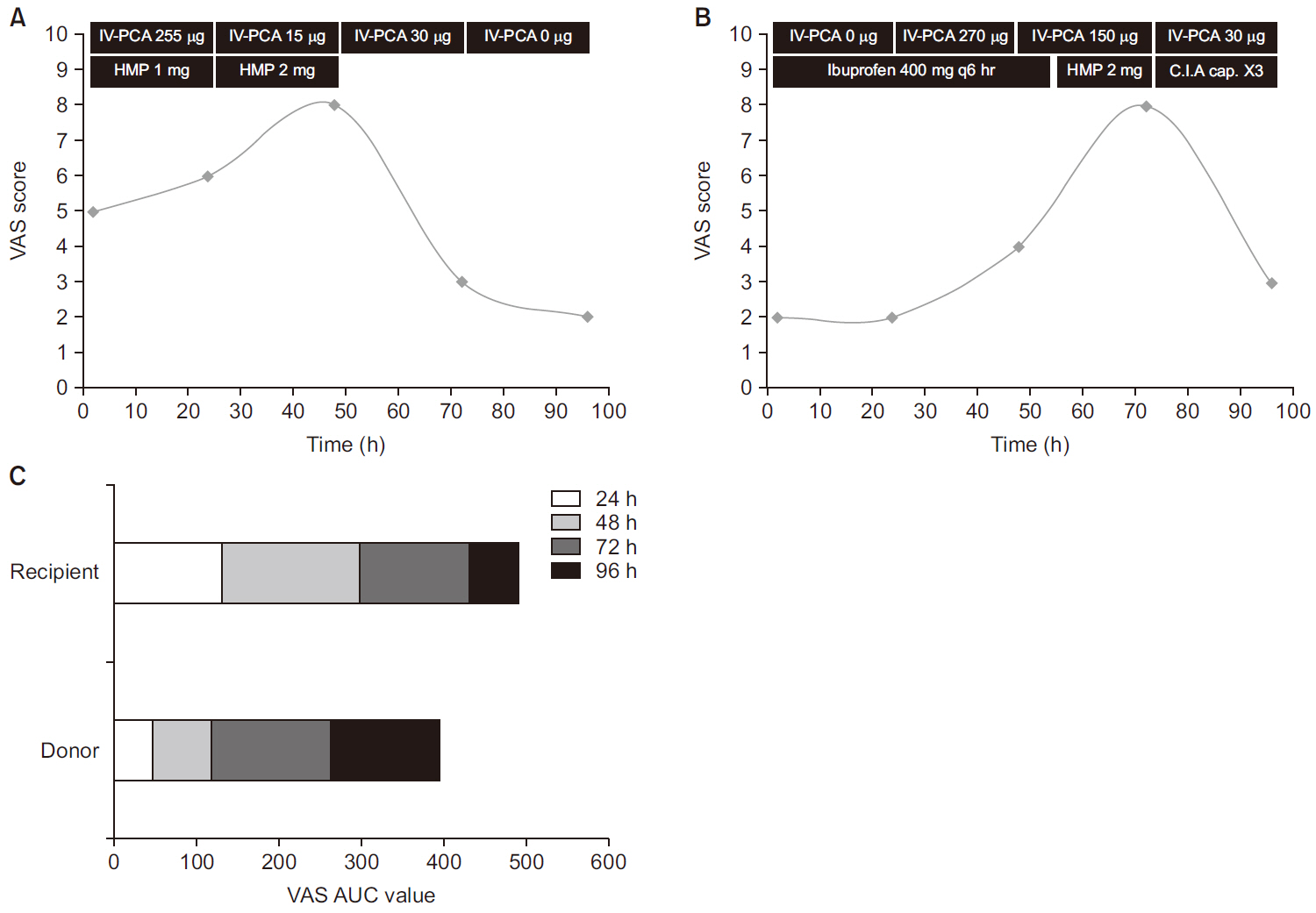
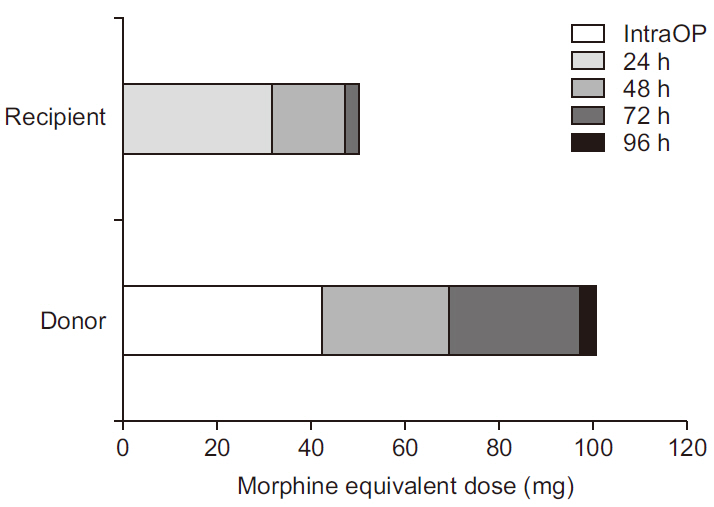
There have been many reports about decreased analgesic requirements in liver transplant recipients compared with patients undergoing other abdominal surgery. Case: Herein we describe a case in which a 42-year-old man underwent living donor liver transplantation from his monozygotic twin. Because innate pain thresholds may be similar in monozygotic twins, we could effectively investigate postoperative pain in the donor and the recipient. Concordant with previous reports, the recipient used less analgesic than the donor in the present study.
Conclusions
Physicians caring for patients who have received liver transplantation should consider their comparatively low requirement for analgesic, to prevent delayed recovery due to excessive use of analgesic.
Keyword
Figure
Reference
-
Moretti EW., Robertson KM., Tuttle-Newhall JE., Clavien PA., Gan TJ. 2002. Orthotopic liver transplant patients require less postoperative morphine than do patients undergoing hepatic resection. J Clin Anesth. 14:416–20. DOI: 10.1016/S0952-8180(02)00390-2. PMID: 12393108.Chen JP., Jawan B., Chen CL., Wang CH., Cheng KW., Wang CC, et al. 2010. Comparison of postoperative morphine requirements in healthy living liver donors, patients with hepatocellular carcinoma undergoing partial hepatectomy, and liver transplant recipients. Transplant Proc. 42:701–2. DOI: 10.1016/j.transproceed.2010.02.024. PMID: 20430150.Eisenach JC., Plevak DJ., Van Dyke RA RA., Southorn PA., Danielson DR., Krom RA, et al. 1989. Comparison of analgesic requirements after liver transplantation and cholecystectomy. Mayo Clin Proc. 64:356–9. DOI: 10.1016/S0025-6196(12)65257-4. PMID: 2649750.Pai SL., Aniskevich S., Rodrigues ES., Shine TS. 2015. Analgesic considerations for liver transplantation patients. Curr Clin Pharmacol. 10:54–65. DOI: 10.2174/1574884709666140212101228. PMID: 24521192.Donovan KL., Janicki PK., Striepe VI., Stoica C., Franks WT., Pinson CW. 1997. Decreased patient analgesic requirements after liver transplantation and associated neuropeptide levels. Transplantation. 63:1423–9. DOI: 10.1097/00007890-199705270-00010. PMID: 9175805.Ko JS., Choi SJ., Gwak MS., Kim GS., Ahn HJ., Kim JA, et al. 2009. Intrathecal morphine combined with intravenous patient-controlled analgesia is an effective and safe method for immediate postoperative pain control in live liver donors. Liver Transpl. 15:381–9. DOI: 10.1002/lt.21625. PMID: 19326422.Haberer JP., Schoeffler P., Couderc E., Duvaldestin P. 1982. Fentanyl pharmacokinetics in anaesthetized patients with cirrhosis. Br J Anaesth. 54:1267–70. DOI: 10.1093/bja/54.12.1267. PMID: 7171414.Wilkinson GR., Shand DG. 1975. Commentary: a physiological approach to hepatic drug clearance. Clin Pharmacol Ther. 18:377–90. DOI: 10.1002/cpt1975184377. PMID: 1164821.Schäfer M., Carter L., Stein C. 1994. Interleukin 1 beta and corticotropin-releasing factor inhibit pain by releasing opioids from immune cells in inflamed tissue. Proc Natl Acad Sci U S A. 91:4219–23. DOI: 10.1073/pnas.91.10.4219. PMID: 7910403. PMCID: PMC43756.Suzuki T., Yoshiike M., Funada M., Mizoguchi H., Kamei J., Misawa M. 1993. Effect of cyclosporine A on the morphine-induced place preference. Neurosci Lett. 160:159–62. DOI: 10.1016/0304-3940(93)90403-8. PMID: 8247348.Wolkowitz OM., Rubinow D., Doran AR., Breier A., Berrettini WH., Kling MA, et al. 1990. Prednisone effects on neurochemistry and behavior. Preliminary findings. Arch Gen Psychiatry. 47:963–8. DOI: 10.1001/archpsyc.1990.01810220079010. PMID: 1977371.Jullien T., Valtier B., Hongnat JM., Dubourg O., Bourdarias JP., Jardin F. 1995. Incidence of tricuspid regurgitation and vena caval backward flow in mechanically ventilated patients. A color Doppler and contrast echocardiographic study. Chest. 107:488–93. DOI: 10.1378/chest.107.2.488. PMID: 7842782.Mandell MS., Lezotte D., Kam I., Zamudio S. 2002. Reduced use of intensive care after liver transplantation: influence of early extubation. Liver Transpl. 8:676–81. DOI: 10.1053/jlts.2002.34379. PMID: 12149759.