Anesth Pain Med.
2020 Jan;15(1):66-72. 10.17085/apm.2020.15.1.66.
Effect of gastric decompression on postoperative vomiting in pediatric patients undergoing strabismus surgery: a randomized controlled study
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Chosun University Hospital, Gwangju, Korea
- 2Department of Anesthesiology and Pain Medicine, School of Medicine, Chosun University, Gwangju, Korea
- KMID: 2500457
- DOI: http://doi.org/10.17085/apm.2020.15.1.66
Abstract
- Background
Postoperative vomiting (POV) is one of the most serious complications in pediatric patients undergoing strabismus surgery. This study was conducted to test the hypothesis that gastric decompression (GD) could prevent POV caused by gastric distension after mask ventilation.
Methods
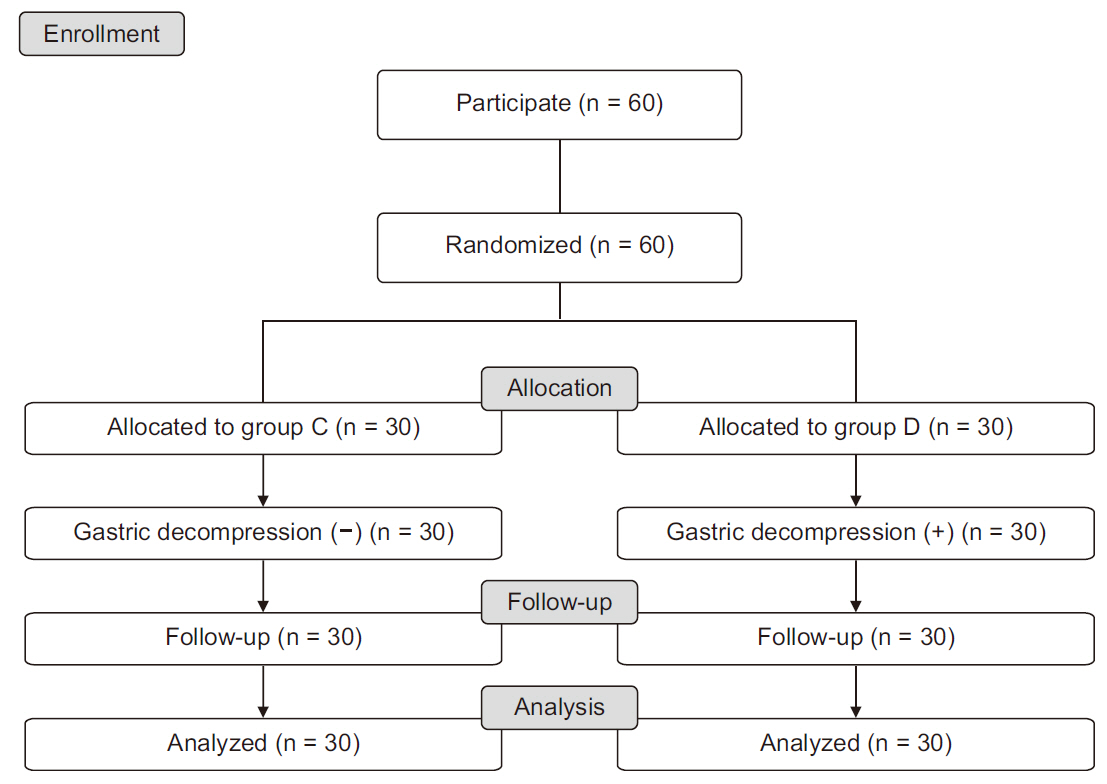
A total of 60 pediatric patients (ASA PS I–II, aged one to 10 years) were randomly allocated to two groups; Group D (n = 30) and Group C (n = 30). Induction of anesthesia was performed with careful face mask ventilation with 100% O2 (3 L/min) and sevoflurane 3 vol% to limit airway pressure below 20 cmH2O. Endotracheal intubation was done after confirming adequate neuromuscular blockade. Then, the patients in Group D received GD, while patients in Group C did not. After the surgery, POV was assessed during the emergence from anesthesia in the operating room and postanesthetic care unit (30 min and 60 min).
Results
During the emergence, POV was significantly decreased in Group D compared to Group C (Group D 3.3% vs. Group C 30.0%, P = 0.006). The odds ratio analysis showed a lower incidence of POV in Group D (odds ratio = 0.080; 95% confidence limit: 0.009–0.685) during the emergence period. There was no significant difference in the incidence of POV in the postanesthetic care unit (Group D 6.7% vs. Group C 4.3% at 30 min, P = 1.000; 0% in both groups at 60 min).
Conclusions
GD reduced the incidence of POV in pediatric patients undergoing strabismus surgery during emergence.
Keyword
Figure
Reference
-
Munro H. 2000. Postoperative nausea and vomiting in children. J Perianesth Nurs. 15:401–7. DOI: 10.1053/jpan.2000.19470. PMID: 11811264.Rose JB., Watcha MF. 1999. Postoperative nausea and vomiting in paediatric patients. Br J Anaesth. 83:104–17. DOI: 10.1093/bja/83.1.104. PMID: 10616338.Tramèr M., Moore A., McQuay H. 1995. Prevention of vomiting after paediatric strabismus surgery: a systematic review using the numbers-needed-to-treat method. Br J Anaesth. 75:556–61. DOI: 10.1093/bja/75.5.556. PMID: 7577280.Eberhart LH., Geldner G., Kranke P., Morin AM., Schäuffelen A., Treiber H, et al. 2004. The development and validation of a risk score to predict the probability of postoperative vomiting in pediatric patients. Anesth Analg. 99:1630–7. DOI: 10.1213/01.ANE.0000135639.57715.6C. PMID: 15562045.Gan TJ., Diemunsch P., Habib AS., Kovac A., Kranke P., Meyer TA, et al. 2014. Consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg. 118:85–113. DOI: 10.1213/ANE.0000000000000002. PMID: 24356162.Erkalp K., Kalekoglu Erkalp N N., Sevdi MS., Korkut AY., Yeter H., Ege SS, et al. 2014. Gastric decompression decreases postoperative nausea and vomiting in ENT surgery. Int J Otolaryngol. 2014:275860. DOI: 10.1155/2014/275860. PMID: 24803935. PMCID: PMC3996959.Palazzo MG., Strunin L. 1984. Anaesthesia and emesis. I: etiology. Can Anaesth Soc J. 31:178–87. DOI: 10.1007/BF03015257. PMID: 6367902.Scammon RE. 1919. Some graphs and tables illustrating the growth of the human stomach. Am J Dis Child. 17:395–422. DOI: 10.1001/archpedi.1919.04110300020002.Kim SH., An TH. 2018. Oral endotracheal intubation in pediatric anesthesia. Anesth Pain Med. 13:241–7. DOI: 10.17085/apm.2018.13.3.241.Farrington M., Lang S., Cullen L., Stewart S. 2009. Nasogastric tube placement verification in pediatric and neonatal patients. Pediatr Nurs. 35:17–24. PMID: 19378570.Lewis SM., Bucher L., Heitkemper MM., Harding M., Kwong J., Roberts D. 2017. Medical surgical nursing: assessment and management of clinical problems. Elsevier;St. Louis: p. 1104.Cohen J. 1992. A power primer. Psychol Bull. 112:155–9. DOI: 10.1037/0033-2909.112.1.155. PMID: 19565683.Gan T., Sloan F., Dear Gde L L., El-Moalem HE., Lubarsky DA. 2001. How much are patients willing to pay to avoid postoperative nausea and vomiting? Anesth Analg. 92:393–400. DOI: 10.1213/00000539-200102000-00022. PMID: 11159239.Scuderi PE., James RL., Harris L., Mims GR 3rd 3rd. 1999. Antiemetic prophylaxis does not improve outcomes after outpatient surgery when compared to symptomatic treatment. Anesthesiology. 90:360–71. DOI: 10.1097/00000542-199902000-00006. PMID: 9952138.Moroz SP., Espinoza J., Cumming WA., Diamant NE. 1976. Lower esophageal sphincter function in children with and without gastroesophageal reflux. Gastroenterology. 71:236–41. DOI: 10.1016/S0016-5085(76)80194-1. PMID: 939384.Lee JH., Jung H., Kim EH., Song IK., Kim HS., Kim JT. 2018. Optimal inspiratory pressure for face mask ventilation in paralyzed and unparalyzed children to prevent gastric insufflation: a prospective, randomized, non-blinded study. Can J Anaesth. 65:1288–95. DOI: 10.1007/s12630-018-1183-2. PMID: 29998359.Lee JH., Jung H., Jang YE., Kim EH., Song IK., Kim HS, et al. 2019. Manual vs pressure-controlled facemask ventilation during the induction of general anesthesia in children: A prospective randomized controlled study. Paediatr Anaesth. 29:331–7. DOI: 10.1111/pan.13594. PMID: 30714260.Babic T., Browning KN. 2014. The role of vagal neurocircuits in the regulation of nausea and vomiting. Eur J Pharmacol. 722:38–47. DOI: 10.1016/j.ejphar.2013.08.047. PMID: 24184670. PMCID: PMC3893663.Rabey PG., Smith G. 1992. Anaesthetic factors contributing to postoperative nausea and vomiting. Br J Anaesth. 69(7 Suppl 1):40S–45S. DOI: 10.1093/bja/69.supplement_1.40S. PMID: 1486013.Hovorka J., Korttila K., Erkola O. 1990. Gastric aspiration at the end of anaesthesia does not decrease postoperative nausea and vomiting. Anaesth Intensive Care. 18:58–61. DOI: 10.1177/0310057X9001800110. PMID: 2186661.Trépanier CA., Isabel L. 1993. Perioperative gastric aspiration increases postoperative nausea and vomiting in outpatients. Can J Anaesth. 40:325–8. DOI: 10.1007/BF03009630. PMID: 8485792.Chukudebelu O., Leonard DS., Healy A., McCoy D., Charles D., Hone S, et al. 2010. The effect of gastric decompression on postoperative nausea and emesis in pediatric, tonsillectomy patients. Int J Pediatr Otorhinolaryngol. 74:674–6. DOI: 10.1016/j.ijporl.2010.03.021. PMID: 20381174.Jones JE., Tabaee A., Glasgold R., Gomillion MC. 2001. Efficacy of gastric aspiration in reducing posttonsillectomy vomiting. Arch Otolaryngol Head Neck Surg. 127:980–4. DOI: 10.1001/archotol.127.8.980. PMID: 11493210.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effects of Clonidine and Midazolam to Prevent Vomiting after Strabismus Surgery in Childeren
- The Prevention of Postoperative Nausea and Vomiting after Strabismus Surgery in Children
- Oculocardiac Reflex and Postoperative Recovery in Pediatric Strabismus Surgery: A Randomized Trial Comparing Four Anesthetic Techniques
- Comparative Study of Ondansetron versus Droperidol versus Placebo to Prevent Postoperative Nausea and Vomiting after Strabismus in Children
- The Effect of Previous Orbital Decompression on Outcome of Strabismus Surgery in Patients with Thyroid Ophthalmopathy