Ann Clin Neurophysiol.
2020 Apr;22(1):24-28. 10.14253/acn.2020.22.1.24.
Febrile Hashimoto’s encephalopathymimicking infectious encephalitis
- Affiliations
-
- 1Department of Neurology, Eulji Medical Center, Eulji University College of Medicine, Seoul, Korea
- KMID: 2500300
- DOI: http://doi.org/10.14253/acn.2020.22.1.24
Abstract
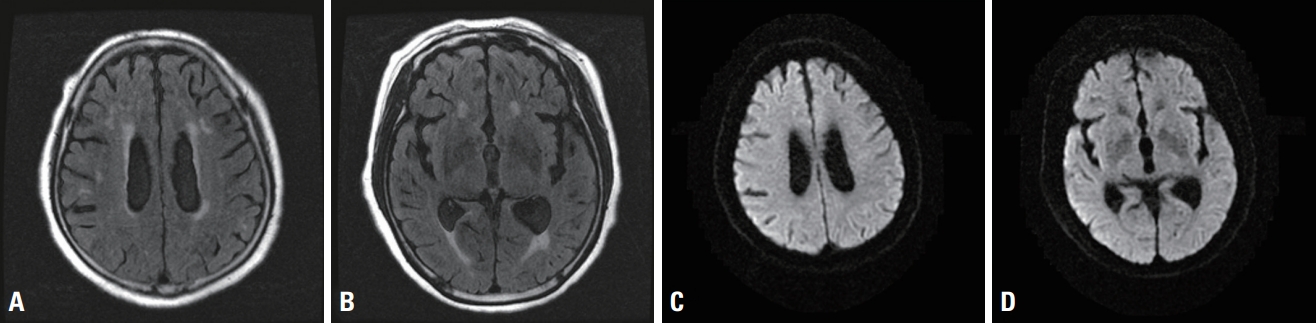
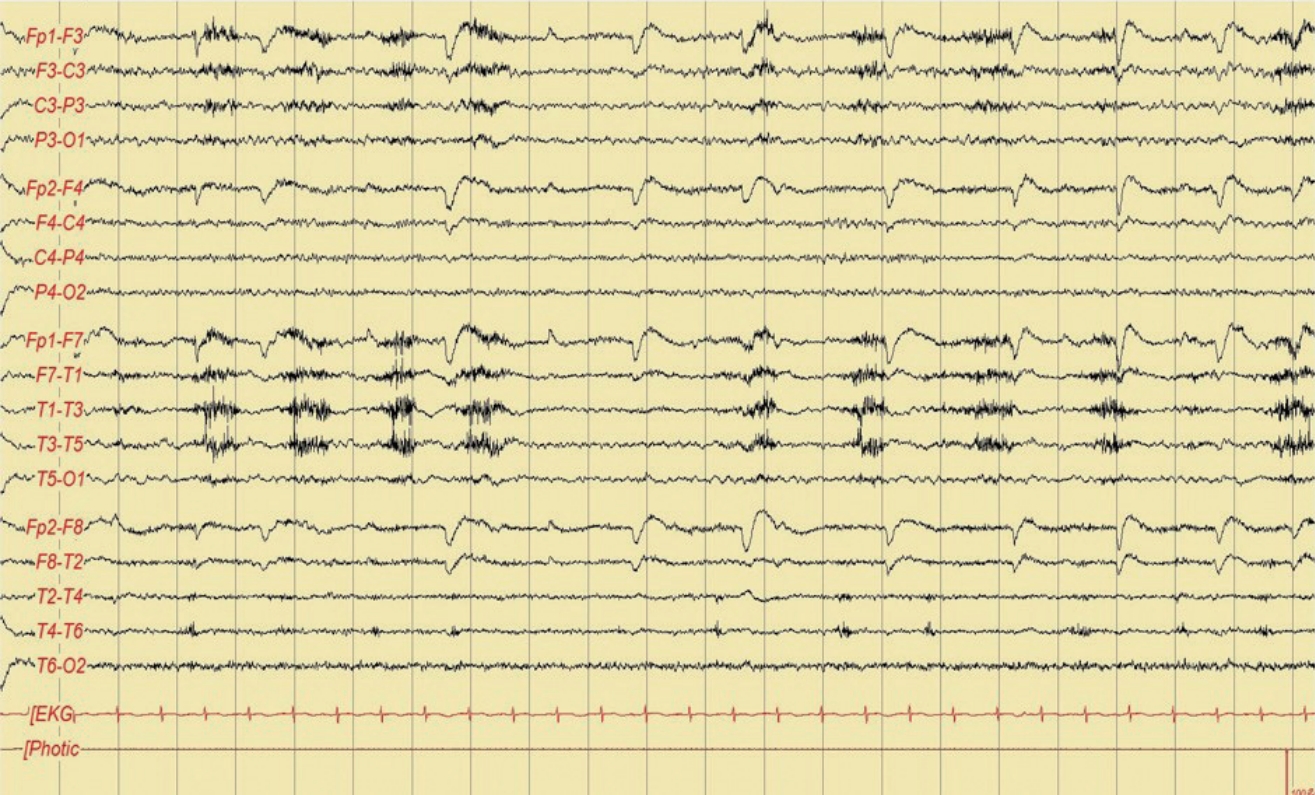
- Hashimoto’s encephalopathy (HE) is a heterogeneous encephalopathy with diverse clinical presentations. Here we report on a 69-year-old woman who presented with confusion, aphasia, fever, and focal ictal discharges. Cerebrospinal fluid analysis and a workup for other fever origins revealed no abnormality and a high level of thyroperoxidase antibody was detected, which findings led to a diagnosis of HE. The symptoms subsided after treatment. This study highlights the importance of considering HE in patients presenting with fever and abnormal EEG findings.
Keyword
Figure
Reference
-
1. Brain L, Jellinek E, Ball K. Hashimoto’s disease and encephalopathy. Lancet. 1966; 2:512–514.
Article2. Chong JY, Rowland LP, Utiger RD. Hashimoto encephalopathy: syndrome or myth? Arch Neurol. 2003; 60:164–171.3. Henchey R, Cibula J, Helveston W, Malone J, Gilmore RL. Electroencephalographic findings in Hashimoto’s encephalopathy. Neurology. 1995; 45:977–981.
Article4. Papathanasopoulos P, Mallioris K, Karanasios P, Dimopoulos D, Papapetropoulos T. Febrile Hashimoto’s encephalopathy. J Neurol Neurosurg Psychiatry. 2000; 68:795.
Article5. Kayser L, Broholm H, Francis D, Perrild H, Olsen BE, Bendtzen K, et al. Immunocytochemical localisation of tumour necrosis factor alpha in thyroid tissues from patients with neoplastic or autoimmune thyroid disorders. Autoimmunity. 1996; 23:91–97.6. Semel JD. Complex partial status epilepticus presenting as fever of unknown origin. Arch Intern Med. 1987; 147:1571–1572.
Article7. el-Ad B, Neufeld MY. Periodic febrile confusion as a presentation of complex partial status epilepticus. Acta Neurol Scand. 1990; 82:350–352.
Article8. Matsuda N, Akanuma J, Shimizu S, Shibano K, Nakahara T, Sugiyama Y, et al. Recurrent episodes of fever of unknown origin as temporal lobe epilepsy. Rinsho Shinkeigaku. 2000; 40:999–1002.9. Leitinger M, Beniczky S, Rohracher A, Gardella E, Kalss G, Qerama E, et al. Salzburg Consensus Criteria for Non-Convulsive Status Epilepticus–approach to clinical application. Epilepsy Behav. 2015; 49:158–163.10. Ch’ien LT, Boehm RM, Robinson H, Liu C, Frenkel LD. Characteristic early electro-encephalographic changes in herpes simplex encephalitis. Arch Neurol. 1977; 34:361–364.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of Hashimoto's encephalopathy presenting with seizures and psychosis
- Anti-GABA-B Receptor Autoimmune Encephalitis
- Predictive and Prognostic Factors of Viral Encephalitis in Pediatric Patients
- Corticosteroid Treatment in Autoimmune Encephalitis
- Statistical Analyses of the Diseases of the Nervous system: With Special Reference to the Annual Change of the Incidence