Brain Tumor Res Treat.
2020 Apr;8(1):53-56. 10.14791/btrt.2020.8.e9.
Primary Gliosarcoma with Extracranial Metastasis
- Affiliations
-
- 1Department of Neurosurgery, Daegu Fatima Hospital, Daegu, Korea
- KMID: 2500122
- DOI: http://doi.org/10.14791/btrt.2020.8.e9
Abstract
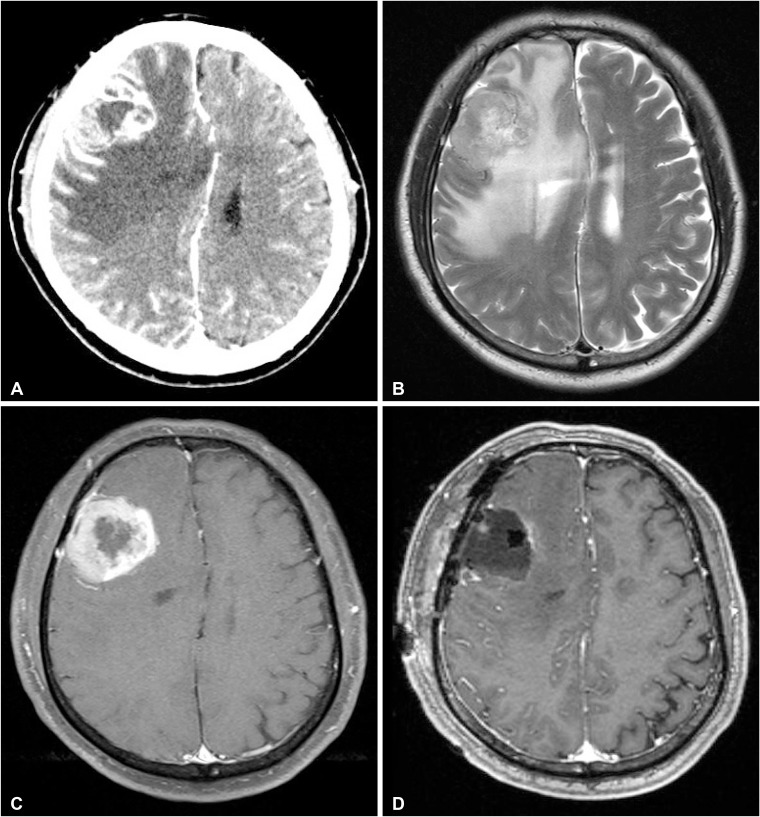
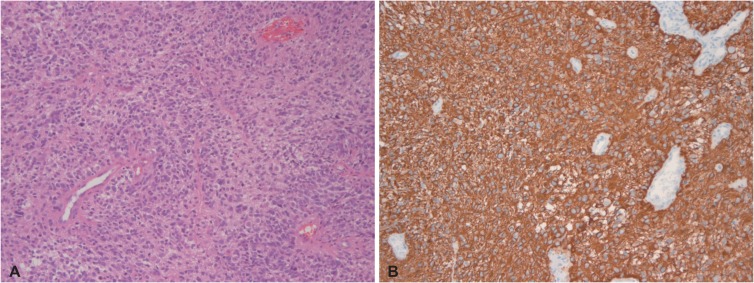
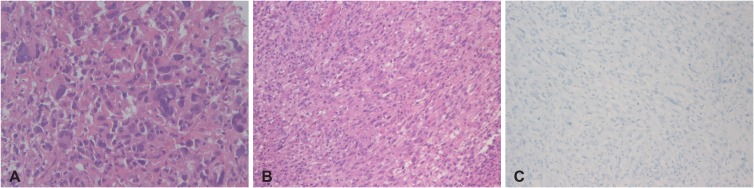
- A 69-year-old male presented with a week of worsening headache, mild dizziness and left side weakness, and the radiological work-up of his brain displayed an enhancing mass on the right frontal lobe. The tumor was totally resected. The patient was initially diagnosed with glioblastoma multiforme. His neurologic symptoms recovered after surgery. He underwent adjuvant radiotherapy with concurrent temozolomide. Approximately 7 months after surgery, the patient complained of epigastric pains. Abdominal CT scan showed multiple hepatic metastasis and multiple lymphadenopathy. Chest CT and Torso positron emission tomography-CT scans for additional metastasis study revealed multiple metastatic lesions in the right lung, left pleura, liver, lymph nodes, bones, and muscles. Percutaneous liver biopsy was performed, and associated pathology was consistent with sarcomatous component. After liver biopsy, brain tumor pathology was reviewed, which revealed typical gliomatous and sarcomatous components. The patient was therefore diagnosed with metastatic gliosarcoma. The patient was in a septic condition with aggravated pleural effusion. The patient died 9 months after the diagnosis of primary gliosarcoma.
Keyword
Figure
Reference
-
1. Ben Nsir A, Thai QA, Kassar AZ, Ben Said I, Jemel H. Primary cerebellar gliosarcoma with extracranial metastases: an orphan differential diagnosis. World Neurosurg. 2015; 84:2076.e13–2076.e17.2. Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. 2016; 131:803–820. PMID: 27157931.3. Han SJ, Yang I, Tihan T, Prados MD, Parsa AT. Primary gliosarcoma: key clinical and pathologic distinctions from glioblastoma with implications as a unique oncologic entity. J Neurooncol. 2010; 96:313–320. PMID: 19618114.4. Tabibkhooei A, Fattahi A, Ebrahimnia F. Gliosarcoma with long progression free survival: a case report and literature review. Surg Neurol Int. 2018; 9:227. PMID: 30533274.5. Sun Q, Xu R, Xu H, Wang G, Shen X, Jiang H. Extracranial metastases of high-grade glioma: the clinical characteristics and mechanism. World J Surg Oncol. 2017; 15:181. PMID: 28985756.6. Weaver D, Vandenberg S, Park TS, Jane JA. Selective peripancreatic sarcoma metastases from primary gliosarcoma. case report. J Neurosurg. 1984; 61:599–601. PMID: 6747700.7. Ray A, Manjila S, Hdeib AM, et al. Extracranial metastasis of gliobastoma: three illustrative cases and current review of the molecular pathology and management strategies. Mol Clin Oncol. 2015; 3:479–486. PMID: 26137254.8. Mentrikoski M, Johnson MD, Korones DN, Scott GA. Glioblastoma multiforme in skin: a report of 2 cases and review of the literature. Am J Dermatopathol. 2008; 30:381–384. PMID: 18645311.9. Lin ZX, Yang LJ, Huang Q, Fu J. Activated vascular endothelia regulate invasion of glioma cells through expression of fibronectin. Chin Med J (Engl). 2010; 123:1754–1761. PMID: 20819642.10. Beaumont TL, Kupsky WJ, Barger GR, Sloan AE. Gliosarcoma with multiple extracranial metastases: case report and review of the literature. J Neurooncol. 2007; 83:39–46. PMID: 17171442.11. Smith DR, Hardman JM, Earle KM. Contiguous glioblastoma multiforme and fibrosarcoma with extracranial metastasis. Cancer. 1969; 24:270–276. PMID: 4307749.12. Gjerdrum LM, Bojsen-Møller M. 61 year old male with brain tumor and oral, lung, and palpebral masses. Brain Pathol. 1999; 9:421–422. PMID: 10219754.13. Ojeda VJ, Sterrett GF. Cerebral gliosarcoma, pulmonary adenoid-cystic carcinoma, and pulmonary metastatic gliosarcoma: report of an untreated case. Pathology. 1984; 16:217–221. PMID: 6087260.14. Wu W, Zhong D, Zhao Z, Wang W, Li J, Zhang W. Postoperative extracranial metastasis from glioblastoma: a case report and review of the literature. World J Surg Oncol. 2017; 15:231. PMID: 29284526.