Korean J Gastroenterol.
2020 Mar;75(3):147-156. 10.4166/kjg.2020.75.3.147.
Risk Factors for Liver Function Deterioration after Transarterial Chemoembolization Refractoriness in Child-Pugh Class A Hepatocellular Carcinoma Patients
- Affiliations
-
- 1Department of Internal Medicine, Konkuk University School of Medicine, Seoul, Korea. 93haan@hanmail.net
- 2Department of Radiology, Konkuk University School of Medicine, Seoul, Korea.
- KMID: 2471898
- DOI: http://doi.org/10.4166/kjg.2020.75.3.147
Abstract
- BACKGROUND/AIMS
A switch to systemic therapy, such as sorafenib, should be considered for hepatocellular carcinoma (HCC) patients refractory to transarterial chemoembolization (TACE). On the other hand, treatment changes are difficult if the liver function worsens to Child-Pugh B or C. Therefore, predicting the risk factors for non-responsiveness to TACE and deteriorating liver function may be helpful.
METHODS
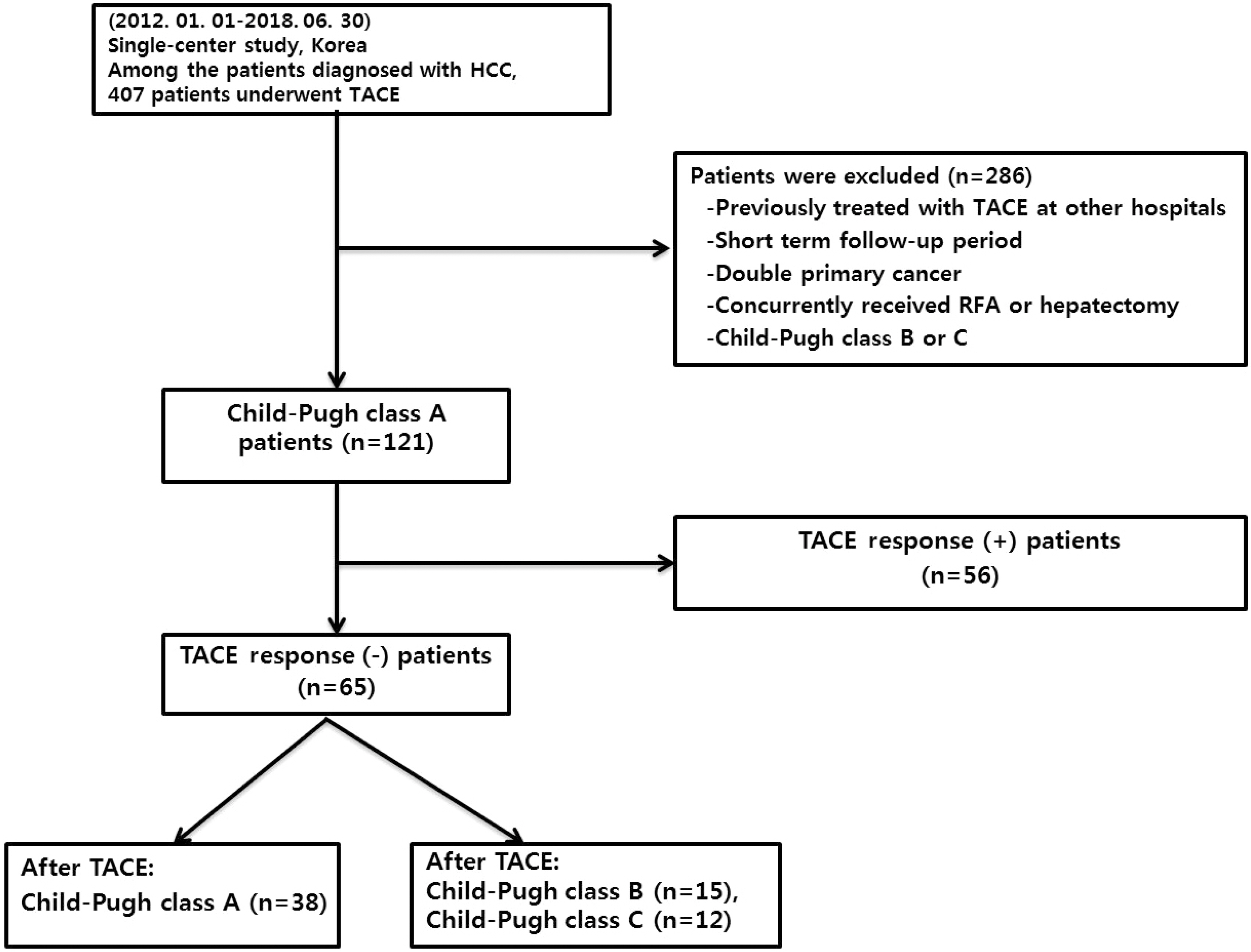
Newly diagnosed Child-Pugh A HCC patients who underwent TACE from January 2012 to June 2018 were included. After 1 year, this study evaluated whether there was a treatment response to TACE and whether the Child-Pugh class had worsened.
RESULTS
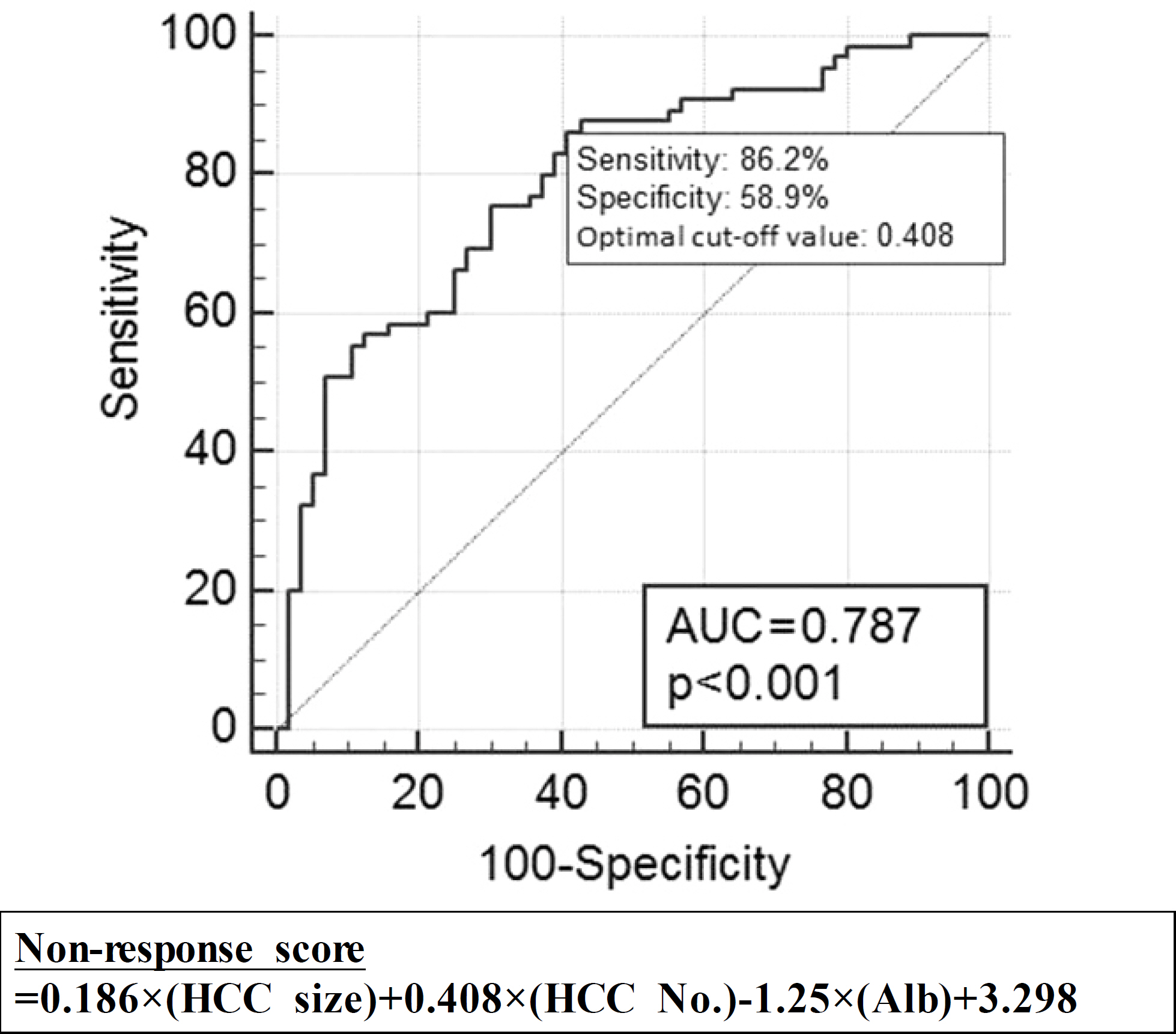
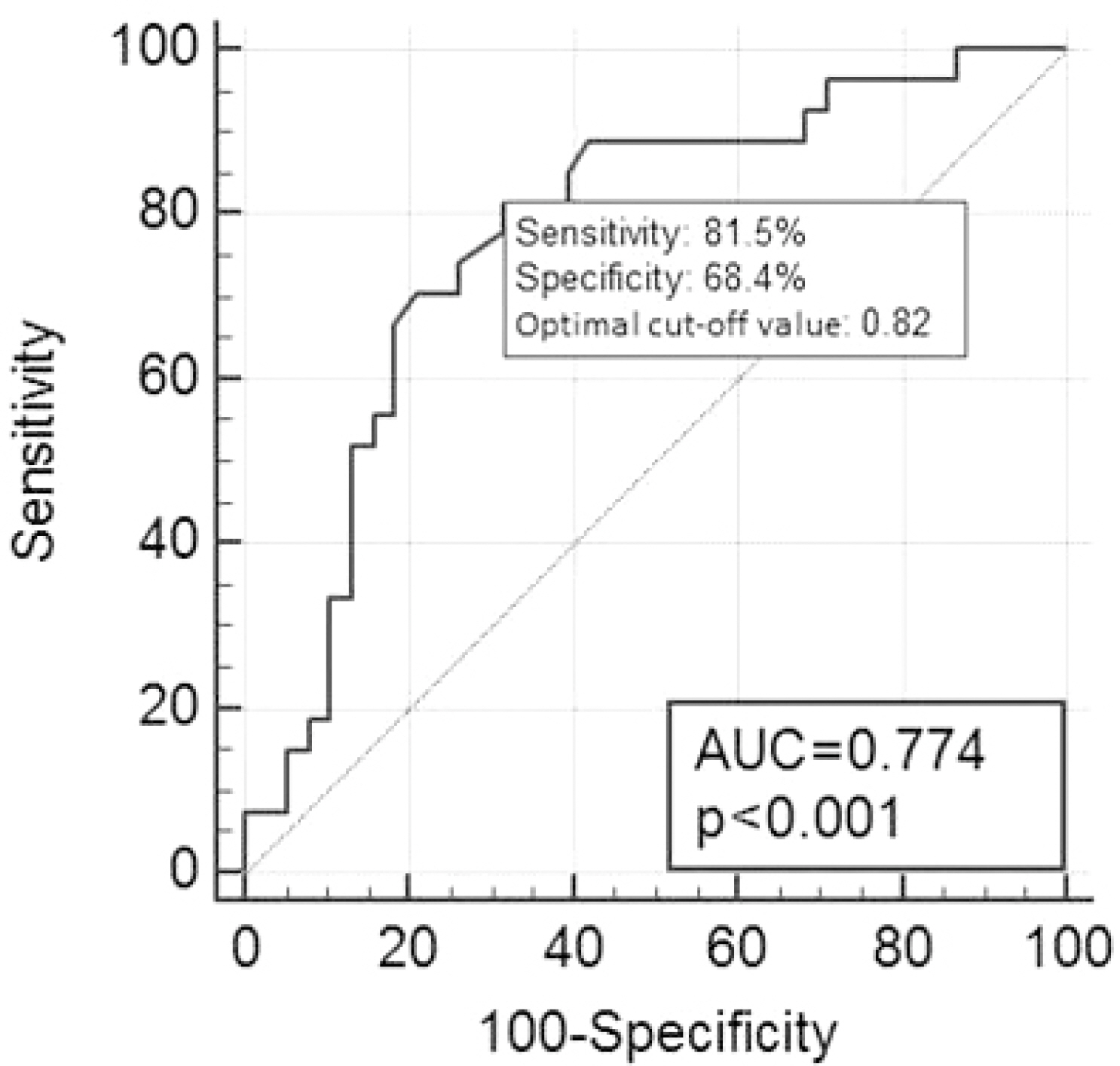
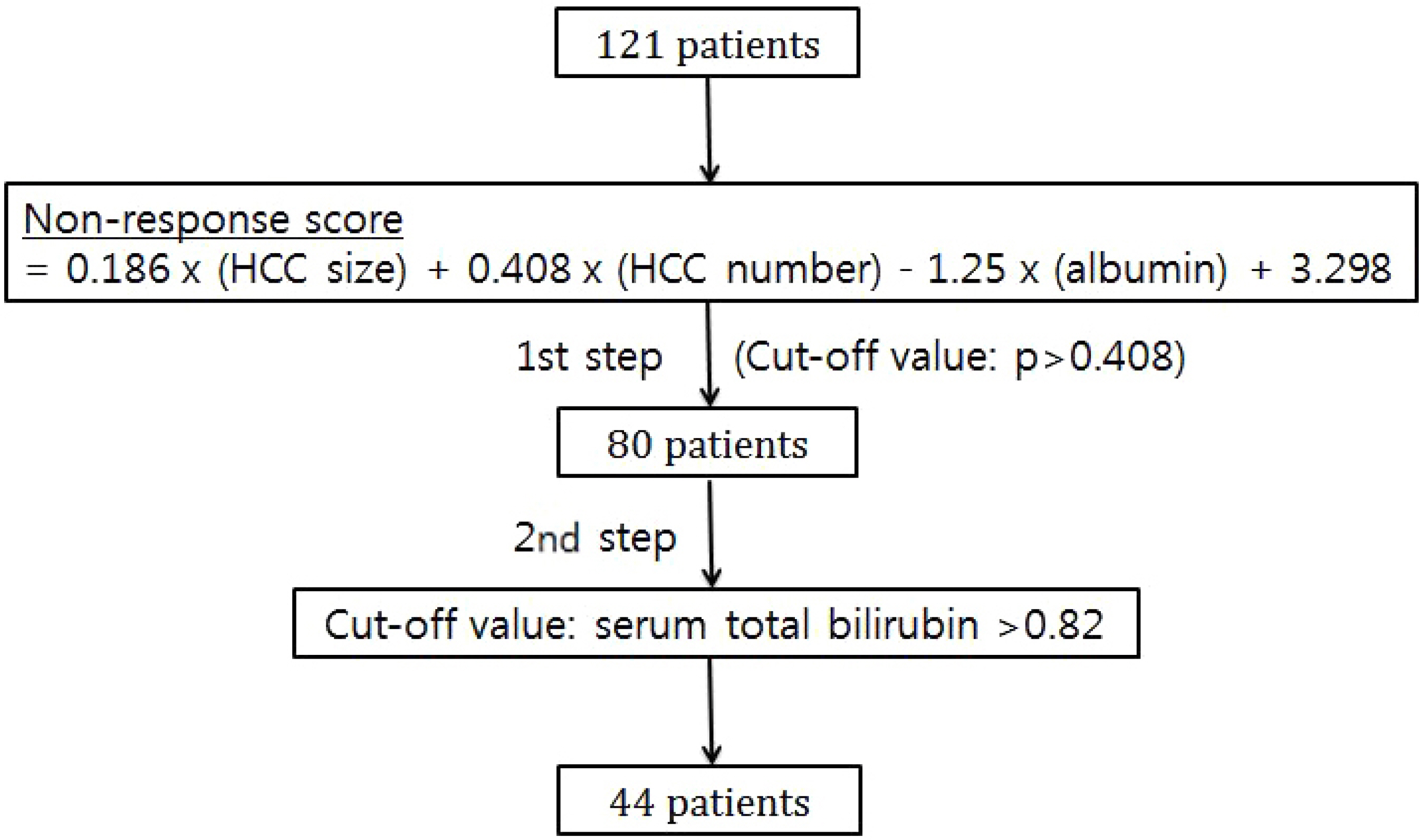
Among 121 patients, 65 were refractory and 56 responded to TACE. In multivariable logistic regression analysis, the tumor size, tumor number, and albumin at the time of the diagnosis of HCC were significant prognostic factors for the treatment response to TACE. Among 65 patients who presented TACE-refractoriness, 27 showed liver function deterioration from Child-Pugh class A to class B or C after TACE. In multivariable logistic regression analysis, bilirubin at the diagnosis of HCC was a significant prognostic factor for liver function deterioration. A predictive algorithm based on the regression equations revealed a sensitivity, specificity, positive predictive value, and negative predictive value of 74.1%, 74.5%, 45.5%, and 90.9%, respectively, for TACE-refractoriness and liver function deterioration.
CONCLUSIONS
The prognostic model incorporating the tumor size, tumor number, albumin, and bilirubin at the diagnosis of HCC may help identify patients who show a poor response to TACE and aggravation of liver function after TACE, who may benefit from early switching into systemic therapy before liver function aggravation.
MeSH Terms
Figure
Reference
-
References
1. Sotiropoulos GC, Lang H, Frilling A, et al. Resectability of hepatocellular carcinoma: evaluation of 333 consecutive cases at a single hepatobiliary specialty center and systematic review of the literature. Hepatogastroenterology. 2006; 53:322–329.2. Park JW, Chen M, Colombo M, et al. Global patterns of hepatocellular carcinoma management from diagnosis to death: the BRIDGE Study. Liver Int. 2015; 35:2155–2166.3. Llovet JM, Bruix J. Systematic review of randomized trials for unresectable hepatocellular carcinoma: chemoembolization improves survival. Hepatology. 2003; 37:429–442.
Article4. Bruix J, Sala M, Llovet JM. Chemoembolization for hepatocellular carcinoma. Gastroenterology. 2004; 127(5 Suppl 1):S179–S188.
Article5. Ogasawara S, Chiba T, Ooka Y, et al. Efficacy of sorafenib in inter-mediate-stage hepatocellular carcinoma patients refractory to transarterial chemoembolization. Oncology. 2014; 87:330–341.
Article6. Korean Liver Cancer Association, National Cancer Center. 2018 Korean Liver Cancer Association-National Cancer Center Korea practice guidelines for the management of hepatocellular carcinoma. Gut Liver. 2019; 13:227–299.7. Yamanaka K, Hatano E, Kitamura K, et al. Early evaluation of transcatheter arterial chemoembolization-refractory hepatocellular carcinoma. J Gastroenterol. 2012; 47:343–346.
Article8. Kim HY, Park JW, Joo J, et al. Severity and timing of progression predict refractoriness to transarterial chemoembolization in hepatocellular carcinoma. J Gastroenterol Hepatol. 2012; 27:1051–1056.
Article9. Kudo M, Izumi N, Kokudo N, et al. Management of hepatocellular carcinoma in Japan: consensus-based clinical practice guidelines proposed by the Japan Society of Hepatology (JSH) 2010 updated version. Dig Dis. 2011; 29:339–364.
Article10. European Association For The Study Of The Liver, European Organisation For Research And Treatment Of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012; 56:908–943.11. Sieghart W, Hucke F, Pinter M, et al. The ART of decision making: retreatment with transarterial chemoembolization in patients with hepatocellular carcinoma. Hepatology. 2013; 57:2261–2273.
Article12. Bruix J, Raoul JL, Sherman M, et al. Efficacy and safety of sorafenib in patients with advanced hepatocellular carcinoma: sub-analyses of a phase III trial. J Hepatol. 2012; 57:821–829.
Article13. Hollebecque A, Cattan S, Romano O, et al. Safety and efficacy of sorafenib in hepatocellular carcinoma: the impact of the Child-Pugh score. Aliment Pharmacol Ther. 2011; 34:1193–1201.
Article14. Kim JE, Ryoo BY, Ryu MH, et al. Sorafenib for hepatocellular carcinoma according to Child-Pugh class of liver function. Cancer Chemother Pharmacol. 2011; 68:1285–1290.
Article15. Marrero JA, Kudo M, Venook AP, et al. Observational registry of sorafenib use in clinical practice across Child-Pugh subgroups: the GIDEON study. J Hepatol. 2016; 65:1140–1147.
Article16. Lencioni R, Llovet JM. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis. 2010; 30:52–60.
Article17. Kadalayil L, Benini R, Pallan L, et al. A simple prognostic scoring system for patients receiving transarterial embolisation for hepatocellular cancer. Ann Oncol. 2013; 24:2565–2570.
Article18. Pinato DJ, Arizumi T, Allara E, et al. Validation of the hepatoma arterial embolization prognostic score in European and Asian populations and proposed modification. Clin Gastroenterol Hepatol. 2015; 13:1204–1208.e2.19. Chan AO, Yuen MF, Hui CK, Tso WK, Lai CL. A prospective study regarding the complications of transcatheter intraarterial lip-iodol chemoembolization in patients with hepatocellular carcinoma. Cancer. 2002; 94:1747–1752.
Article20. Hwang JI, Chow WK, Hung SW, et al. Development of a safety index of transarterial chemoembolization for hepatocellular carcinoma to prevent acute liver damage. Anticancer Res. 2005; 25(3c):2551–2554.21. Kudo M. A new era of systemic therapy for hepatocellular carcinoma with regorafenib and lenvatinib. Liver Cancer. 2017; 6:177–184.
Article22. Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet. 2018; 391:1301–1314.
Article23. Kim DY. New systemic therapies for advanced hepatocellular carcinoma. Korean J Gastroenterol. 2019; 73:10–15.
Article24. Dika IE, Abou-Alfa GK. Treatment options after sorafenib failure in patients with hepatocellular carcinoma. Clin Mol Hepatol. 2017; 23:273–239.
Article25. Kudo M, Finn RS, Qin S, et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet. 2018; 391:1163–1173.
Article26. Bruix J, Qin S, Merle P, et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017; 389:56–66.
Article27. Villanueva A. Hepatocellular carcinoma. N Engl J Med. 2019; 380:1450–1462.
Article28. Chung JW. Recent advance in international management of hepatocellular carcinoma. J Korean Med Assoc. 2013; 56:972–982.
Article29. Miyayama S, Yamashiro M, Ikuno M, Okumura K, Yoshida M. Ultraselective transcatheter arterial chemoembolization for small hepatocellular carcinoma guided by automated tumor-feeders detection software: technical success and short-term tumor response. Abdom Imaging. 2014; 39:645–656.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The effect of Transarterial Chemoembolization(TAE) on Lung metastasis of Hepatocellular Carcinoma
- Analysis of Survival Rates by Surgical Resection or Transarterial Chemo-embolization as the Initial Treatment for the Patients with Hepatocellular Carcinoma (UICC T stage 1, 2, 3) and Child-Pugh Class A Liver Function
- Ruptured Massive Hepatocellular Carcinoma Cured by Transarterial Chemoembolization
- Rare Case of Pyogenic Brain Abscess after Transarterial Chemoembolization in a Patient with Hepatocellular Carcinoma: Case Report and Literature Review
- Optimizing the management of intermediate-stage hepatocellular carcinoma: Current trends and prospects