Imaging Sci Dent.
2020 Mar;50(1):53-64. 10.5624/isd.2020.50.1.53.
Incidental findings in a consecutive series of digital panoramic radiographs
- Affiliations
-
- 1Division of Oral and Maxillofacial Radiology, Faculty of Dentistry, University of British Columbia, Vancouver, British Columbia, Canada. dmacdon@dentistry.ubc.ca
- KMID: 2471846
- DOI: http://doi.org/10.5624/isd.2020.50.1.53
Abstract
- PURPOSE
The aim of this study was to determine the prevalence of incidental findings (IFs) on digital dental panoramic radiographs (DPRs) of asymptomatic patients attending a general dental practice.
MATERIALS AND METHODS
This was a retrospective study of 6,252 consecutive digital (photostimulatable phosphor) DPRs of patients who visited a Canadian general dental practice for a complete new patient examination. The IFs were grouped into dental-related anomalies, radiopacities and radiopacities in the jaws, changes in the shape of the condyles, and other findings in the jaws, such as tonsilloliths and mucosal antral pseudocysts. Their prevalence was determined.
RESULTS
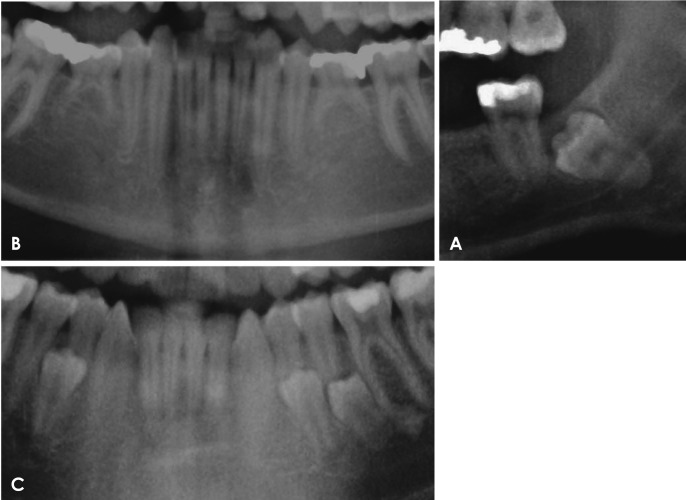
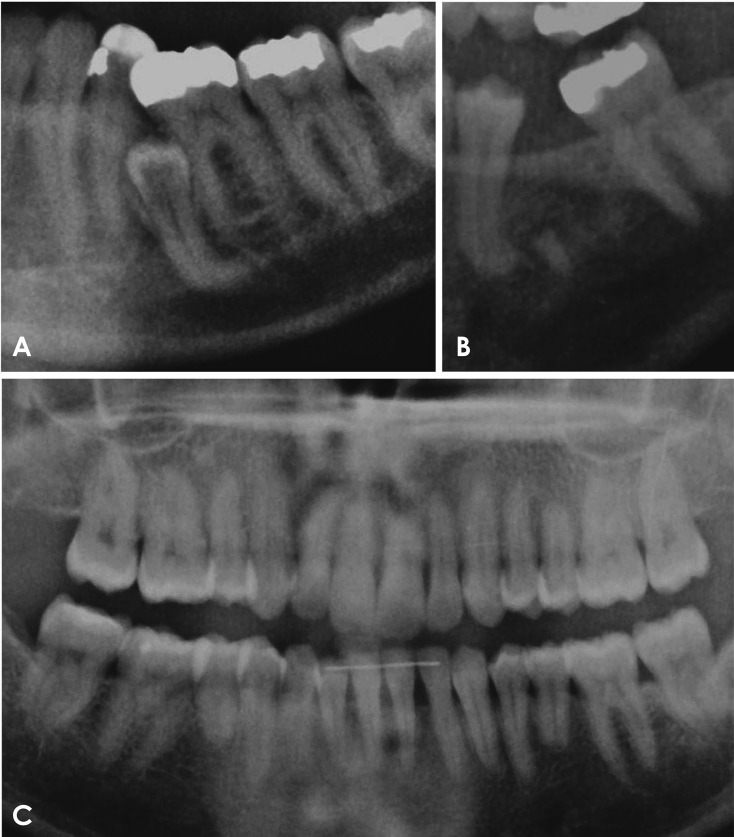
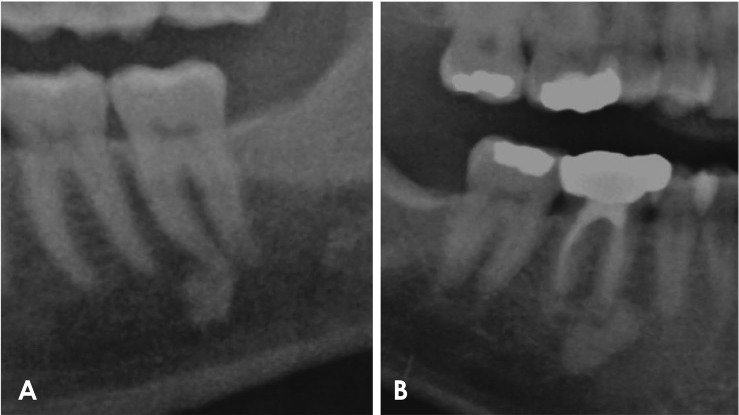
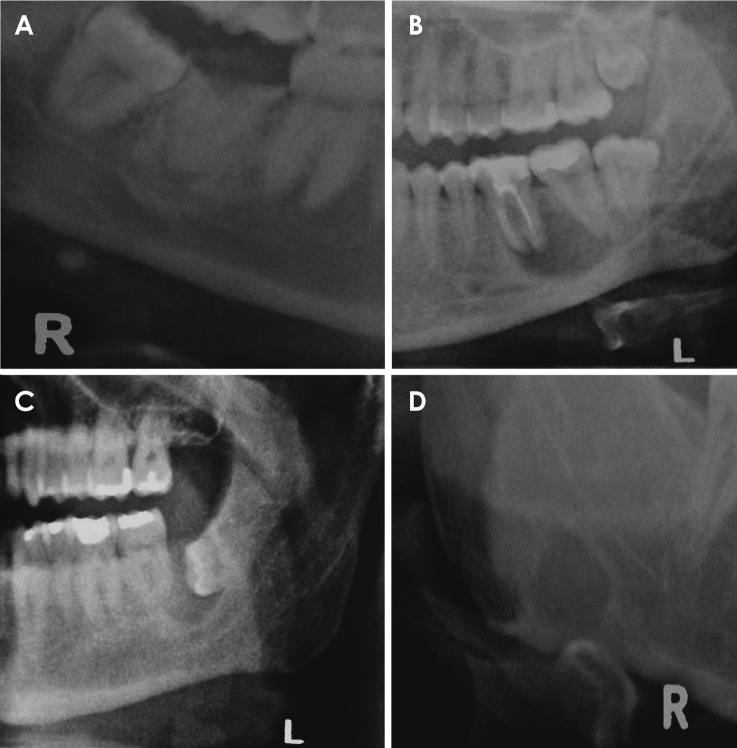
Thirty-two percent of the DPRs showed at least 1 IF. The highest prevalence was found for dental-related anomalies (29% of all DPRs), of which impacted teeth were the most prevalent finding (24% of all DPRs), followed by idiopathic osteosclerosis (6% of all DPRs). A lower prevalence was noted for tonsilloliths (3%), and the prevalence of root tips, mucosal antral pseudocysts, and anomalies in condylar shape was approximately 1% each.
CONCLUSION
The observed prevalence of 32.1% for IFs of any type underscores the need for a dental practitioner to review the entire DPR when a patient presents for an initial dental examination (or check-up) or for dental hygiene. Only a single IF (a central giant cell granuloma) provoked alarm, as it was initially considered malignant. Similarly, impacted teeth and suspected cysts need careful evaluation upon discovery to determine how they may be optimally managed.
Keyword
MeSH Terms
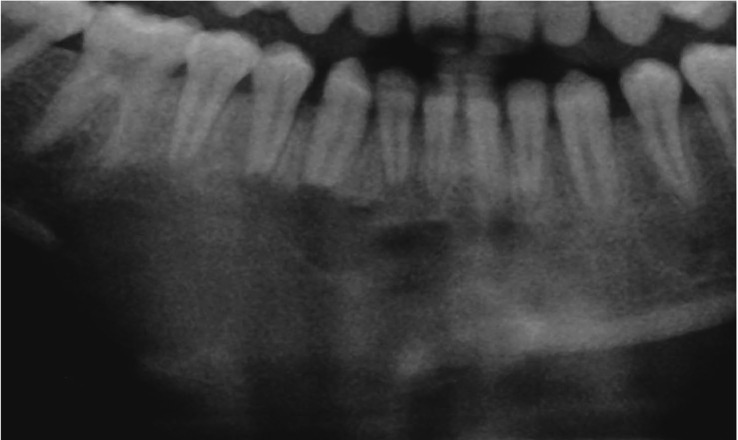
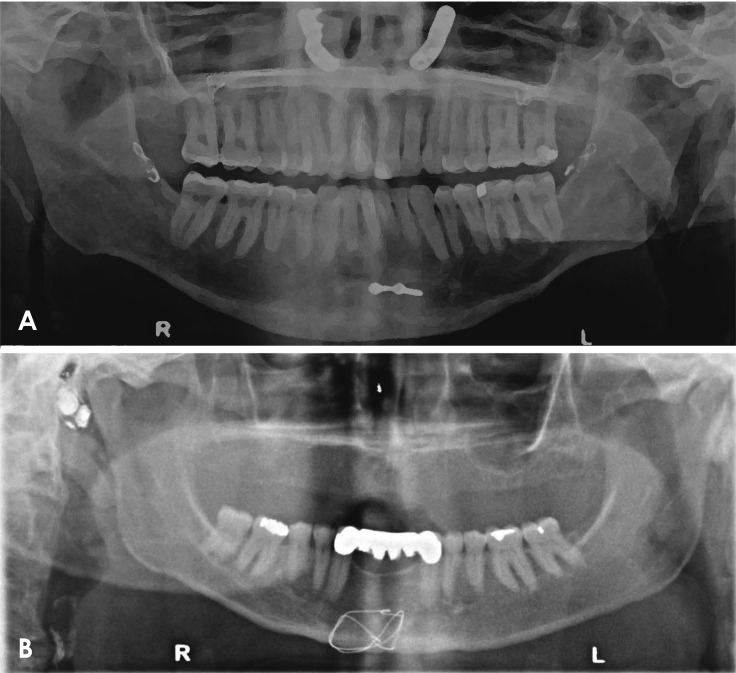
Figure
Reference
-
1. MacDonald D. The most frequent and/or important lesions that affect the face and the jaws. Oral Radiol. 2020; 36:1–17. PMID: 30758774.
Article2. MacDonald D, Li T, Leung SF, Curtin J, Yeung A, Martin MA. Extranodal lymphoma arising within the maxillary alveolus: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol. 2017; 124:e233–e238. PMID: 28624341.
Article3. MacDonald D, Lim S. Extranodal lymphoma arising within the maxillary alveolus: a systematic review. Oral Radiol. 2018; 34:113–126. PMID: 30147235.
Article4. Morris CR, Marano PD, Swimley DC, Runco JG. Abnormalities noted on panoramic radiographs. Oral Surg Oral Med Oral Pathol. 1969; 28:772–782. PMID: 5259463.
Article5. MacDonald-Jankowski DS. The detection of abnormalities in the jaws: a radiological survey. Br Dent J. 1991; 170:215–218. PMID: 2021494.
Article6. MacDonald D. Oral and maxillofacial radiology: a diagnostic approach. 2nd ed. Hoboken, NJ: Wiley-Blackwell;2020.7. Mallya S, Lam E. White and Pharoah's oral radiology: principles and interpretation. 8th ed. St. Louis, MO: Elsevier;2019.8. MacDonald-Jankowski DS, Orpe EC. Some current legal issues that may affect oral and maxillofacial radiology. Part 2: digital monitors and cone-beam computed tomography. J Can Dent Assoc. 2007; 73:507–511. PMID: 17672955.9. Alberta Government. Regional economic indicators. Peace Country region [Internet]. Edmonton: Treasury Board and Enterprise;2011. updated 2012 Mar 1. cited 2019 Oct 4. Available from: https://open.alberta.ca/publications/1718-2840.10. Statistics Canada [Internet]. Ottawa: Population and dwelling counts, for Canada, provinces and territories, 2011 and 2006 censuses;modified 2019 Jun 3. cited 2019 Oct 4. Available from: https://www12.statcan.gc.ca/census-recensement/2011/dp-pd/hlt-fst/pd-pl/Table-Tableau.cfm?LANG=Eng&T=101&S=50&O=A.11. Kratz RJ, Nguyen CT, Walton JN, MacDonald D. Dental students' interpretations of digital panoramic radiographs on completely edentate patients. J Dent Educ. 2018; 82:313–321. PMID: 29496811.
Article12. Kratz RJ, Walton JN, MacEntee MI, Nguyen CT, MacDonald D. Panoramic radiographs made before complete removable dental prostheses fabrication: a retrospective study of clinical significance. J Prosthet Dent. 2017; 118:26–30. PMID: 28024823.13. Lowry R. For a 2×2 contingency table [Internet]. Poughkeepsie (NY): VassarStats: website for statistical computation;C1988-2020. cited 2019 Oct 4. Available from: http://vassarstats.net/tab2x2.html.14. McDonnell D. Dense bone island. A review of 107 patients. Oral Surg Oral Med Oral Pathol. 1993; 76:124–128. PMID: 8351108.15. MacDonald-Jankowski DS. Idiopathic osteosclerosis in the jaws of Britons and of the Hong Kong Chinese: radiology and systematic review. Dentomaxillofac Radiol. 1999; 28:357–363. PMID: 10578190.
Article16. Takahashi A, Sugawara C, Kudoh T, Ohe G, Takamaru N, Tamatani T, et al. Prevalence and imaging characteristics of palatine tonsilloliths evaluated on 2244 pairs of panoramic radiographs and CT images. Clin Oral Investig. 2017; 21:85–91.
Article17. Lim HK, Kim SM, Kim MJ, Lee JH. Clinical, statistical and chemical study of sialolithiasis. J Korean Assoc Oral Maxillofac Surg. 2012; 38:44–49.
Article18. MacDonald-Jankowski DS. Mucosal antral cysts observed within a London inner-city population. Clin Radiol. 1994; 49:195–198. PMID: 8143412.
Article19. MacDonald-Jankowski DS. Mucosal antral cysts in a Chinese population. Dentomaxillofac Radiol. 1993; 22:208–210. PMID: 8181649.
Article20. Horner K, MacDonald D. Conventional radiography in TMJ imaging. In : Rozylo-Kalinowska I, Orhan K, editors. Imaging of the temporomandibular joint. Cham: Springer;2019. p. 79–90.21. MacDonald D, Horner K. Conventional radiographic findings of TMJ disorders. In : Rozylo-Kalinowska I, Orhan K, editors. Imaging of the Temporomandibular Joint. Cham: Springer;2019. p. 91–114.22. Health Canada. Report on the findings of the oral health component of the Canadian health measures survey 2007–2009. Ottawa: Publications Health Canada;2010. cited Feb 7, 2020. https://www.caphd.ca/sites/default/files/CHMS-E-tech.pdf.23. Chu FC, Li TK, Lui VK, Newsome PR, Chow RL, Cheung LK. Prevalence of impacted teeth and associated pathologies - a radiographic study of the Hong Kong Chinese population. Hong Kong Med J. 2003; 9:158–163. PMID: 12777649.24. Canadian Dental Association. The state of oral health in Canada [Internet]. Ottawa: Canadian Dental Association;2017. cited 2019 Oct 4. Available from: https://www.cda-adc.ca/stateoforalhealth/_files/TheStateofOralHealthinCanada.pdf.25. Northern Alberta Development Council. Recommendations on health care in northern Alberta [Internet]. Alberta: Northern Alberta Development Council;2007. cited 2019 Oct 4. Available from: http://www.nadc.gov.ab.ca/Docs/Health-Recommendations.pdf.26. Hackbarth D. Report 76-4. Hydrogeology of the Grande Prairie area, Alberta [Internet]. Alberta: Alberta Research Council;1977. cited 2019 Oct 4. Available from: https://ags.aer.ca/document/ESR/ESR_1976_04.pdf.27. MacDonald D. Lesions of the jaws presenting as radiolucencies on cone-beam CT. Clin Radiol. 2016; 71:972–985. PMID: 27371961.
Article28. Assaf AT, Solaty M, Zrnc TA, Fuhrmann AW, Scheuer H, Heiland M, et al. Prevalence of Stafne's bone cavity - retrospective analysis of 14,005 panoramic views. In Vivo. 2014; 28:1159–1164. PMID: 25398816.29. Sisman Y, Miloglu O, Sekerci AE, Yilmaz AB, Demirtas O, Tokmak TT. Radiographic evaluation on prevalence of Stafne bone defect: a study from two centres in Turkey. Dentomaxillofac Radiol. 2012; 41:152–158. PMID: 22074869.
Article30. Correll RW, Jensen JL, Rhyne RR. Lingual cortical mandibular defects: a radiographic incidence study. Oral Surg Oral Med Oral Pathol. 1980; 50:287–291. PMID: 6932004.31. Aoun G, Nasseh I, Diab HA, Bacho R. Palatine tonsilloliths: a retrospective study on 500 digital panoramic radiographs. J Contemp Dent Pract. 2018; 19:1284–1287. PMID: 30498187.
Article32. Sigismund PE, Zenk J, Koch M, Schapher M, Rudes M, Iro H. Nearly 3,000 salivary stones: some clinical and epidemiologic aspects. Laryngoscope. 2015; 125:1879–1882. PMID: 25994240.
Article33. Kim SY, Kim HJ, Lim H, Lim MS, Kim M, Park IS, et al. Association between cholelithiasis and sialolithiasis: two longitudinal follow-up studies. Medicine (Baltimore). 2019; 98:e16153. PMID: 31232971.34. Vallo J, Suominen-Taipale L, Huumonen S, Soikkonen K, Norblad A. Prevalence of mucosal abnormalities of the maxillary sinus and their relationship to dental disease in panoramic radiography: results from the Health 2000 Health Examination Survey. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 109:e80–e87. PMID: 20219592.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- More frequent detection of calcified carotid atherosclerotic plaques and mineralized laryngeal cartilages on digital than on film-based panoramic radiographs
- Comparison of panoramic radiography and cone-beam computed tomography for assessing radiographic signs indicating root protrusion into the maxillary sinus
- Analysis of the Prevalence of Taurodont Deciduous Molars in Children
- Prediction of osteoporosis using fractal analysis on periapical and panoramic radiographs
- Projection angles of mandibular condyles in panoramic and transcranial radiographs