Korean J Radiol.
2019 Dec;20(12):1653-1661. 10.3348/kjr.2019.0192.
US-Guided Radiofrequency Ablation for Low-Risk Papillary Thyroid Microcarcinoma: Efficacy and Safety in a Large Population
- Affiliations
-
- 1Department of Radiology, Soonchunhyang University Seoul Hospital, Seoul, Korea.
- 2Department of Radiology and Research Institute of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- 3Department of Otolaryngology-Head and Neck Surgery, Kosin University College of Medicine, Busan, Korea.
- 4Department of Radiology, Korean Association of Health Promotion, Busan, Korea.
- 5Department of Radiology, Haeundae Sharing and Happiness Hospital, Busan, Korea. snhbsm@naver.com
- KMID: 2471678
- DOI: http://doi.org/10.3348/kjr.2019.0192
Abstract
OBJECTIVE
To evaluate the efficacy and safety of radiofrequency ablation (RFA) for low-risk papillary thyroid microcarcinoma (PTMC) in a large population.
MATERIALS AND METHODS
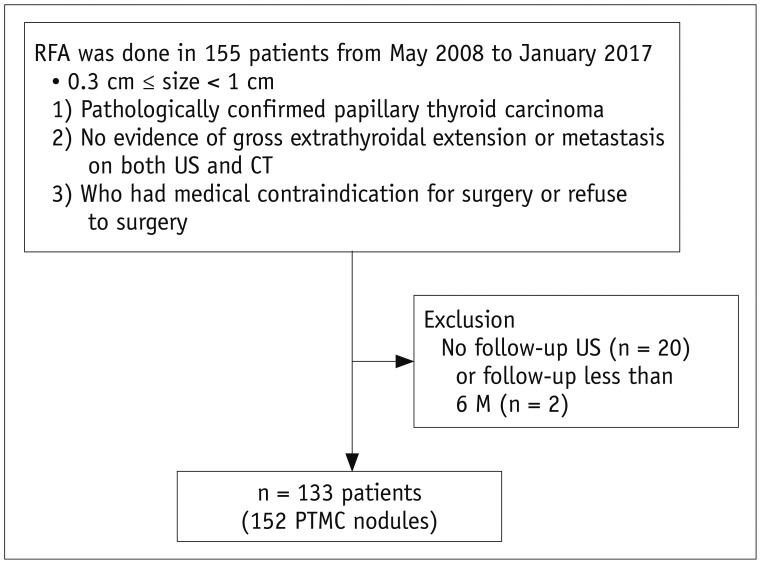
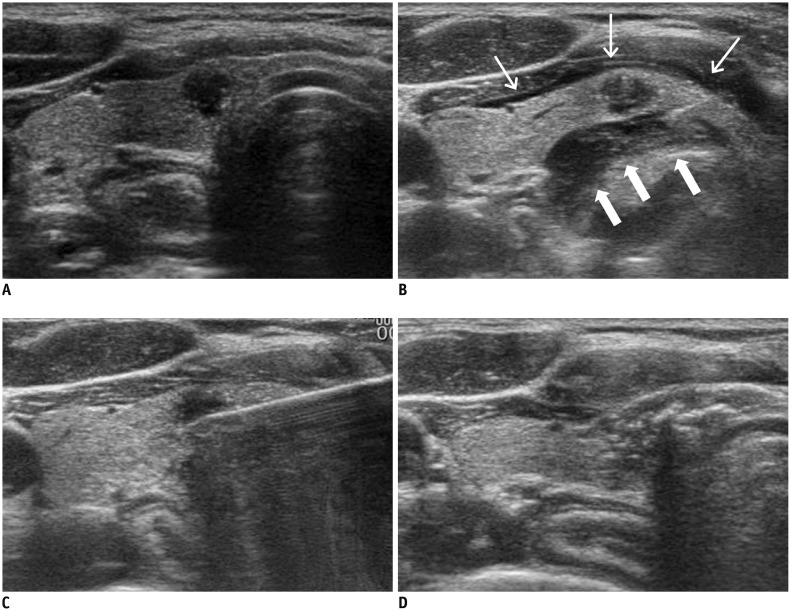
Cases of 152 biopsy-proven PTMCs from 133 patients who had undergone RFA for PTMC between May 2008 and January 2017 were included in this study. All patients were either of high surgical risk or refused to undergo surgery. They were followed up for at least 6 months after initial RFA. Ultrasonography (US) and computed tomography were performed to evaluate the PTMC and the presence of neck metastasis before treatment. RFA was conducted using an internally cooled thyroid-dedicated electrode system. Follow-up US was performed at 1 week, and 2, 6, and 12 months, after the initial RFA, and then at every 6-12 months. We evaluated serial changes of ablated tumors, newly developed cancers, lymph node (LN) or distant metastasis and complications.
RESULTS
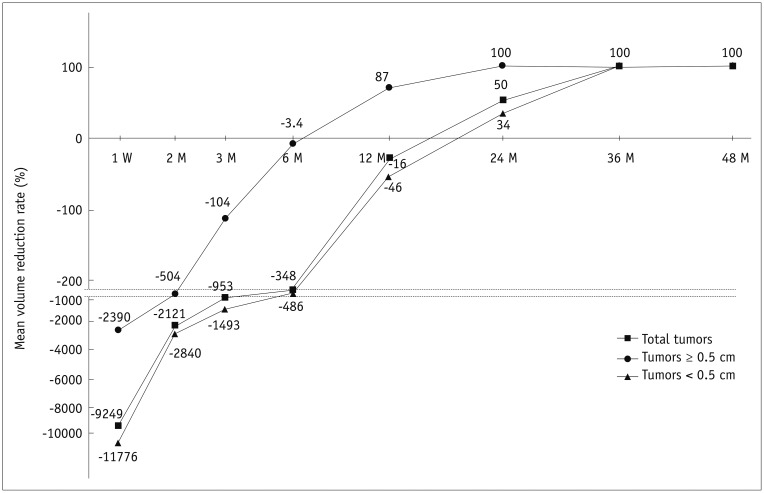
Complete disappearance was found in 91.4% (139/152) of ablated tumors. Among the 13 tumors in patients who did not show complete disappearance, no tumor displayed any regrowth of the residual ablated lesion during the follow-up period. The mean follow-up period was 39 months. During the follow-up period, there were no local recurrence, no LN or distant metastasis, and no newly developed thyroid cancers. No patients were referred to surgery. The overall complication rate was 3% (4/133) of patients, including one voice change. There were no life-threatening complications or procedure-related deaths.
CONCLUSION
Our results suggest that RFA is an effective and safe option for treating low-risk PTMC patients who are of high surgical risk or refuse surgery.
MeSH Terms
Figure
Reference
-
1. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016; 26:1–133. PMID: 26462967.
Article2. Hay ID, Thompson GB, Grant CS, Bergstralh EJ, Dvorak CE, Gorman CA, et al. Papillary thyroid carcinoma managed at the Mayo Clinic during six decades (1940–1999): temporal trends in initial therapy and long-term outcome in 2444 consecutively treated patients. World J Surg. 2002; 26:879–885. PMID: 12016468.
Article3. Iñiguez-Ariza NM, Brito JP. Management of low-risk papillary thyroid cancer. Endocrinol Metab (Seoul). 2018; 33:185–194. PMID: 29947175.
Article4. Yue W, Wang S, Yu S, Wang B. Ultrasound-guided percutaneous microwave ablation of solitary T1N0M0 papillary thyroid microcarcinoma: initial experience. Int J Hyperthermia. 2014; 30:150–157. PMID: 24571178.
Article5. Zhang M, Luo Y, Zhang Y, Tang J. Efficacy and safety of ultrasound-guided radiofrequency ablation for treating low-risk papillary thyroid microcarcinoma: a prospective study. Thyroid. 2016; 26:1581–1587. PMID: 27445090.
Article6. Kim JH, Baek JH, Sung JY, Min HS, Kim KW, Hah JH, et al. Radiofrequency ablation of low-risk small papillary thyroidcarcinoma: preliminary results for patients ineligible for surgery. Int J Hyperthermia. 2017; 33:212–219. PMID: 27590679.
Article7. Zhou W, Jiang S, Zhan W, Zhou J, Xu S, Zhang L. Ultrasound-guided percutaneous laser ablation of unifocal T1N0M0 papillary thyroid microcarcinoma: preliminary results. Eur Radiol. 2017; 27:2934–2940. PMID: 27853812.
Article8. Zhang L, Zhou W, Zhan W, Peng Y, Jiang S, Xu S. Percutaneous laser ablation of unifocal papillary thyroid microcarcinoma: utility of conventional ultrasound and contrast-enhanced ultrasound in assessing local therapeutic response. World J Surg. 2018; 42:2476–2484. PMID: 29488064.
Article9. Jeong SY, Baek JH, Choi YJ, Chung SR, Sung TY, Kim WG, et al. Radiofrequency ablation of primary thyroid carcinoma: efficacy according to the types of thyroid carcinoma. Int J Hyperthermia. 2018; 34:611–616. PMID: 29322881.
Article10. Na DG, Baek JH, Jung SL, Kim JH, Sung JY, Kim KS, et al. Korean Society of Thyroid Radiology (KSThR) and Korean Society of Radiology. Core needle biopsy of the thyroid: 2016 consensus statement and recommendations from Korean Society of Thyroid Radiology. Korean J Radiol. 2017; 18:217–237. PMID: 28096731.
Article11. Ha EJ, Lim HK, Yoon JH, Baek JH, Do KH, Choi M, et al. Korean Society of Thyroid Radiology (KSThR) and Korean Society of Radiology. Primary imaging test and appropriate biopsy methods for thyroid nodules: guidelines by Korean Society of Radiology and National Evidence-Based Healthcare Collaborating Agency. Korean J Radiol. 2018; 19:623–631. PMID: 29962869.
Article12. Tuttle RM, Haugen B, Perrier ND. Updated American Joint Committee on Cancer/tumor-node-metastasis staging system for differentiated and anaplastic thyroid cancer (eighth edition): what changed and why? Thyroid. 2017; 27:751–756. PMID: 28463585.
Article13. Kim HJ. Updated guidelines on the preoperative staging of thyroid cancer. Ultrasonography. 2017; 36:292–299. PMID: 28607324.
Article14. Shin JH, Baek JH, Chung J, Ha EJ, Kim JH, Lee YH, et al. Korean Society of Thyroid Radiology (KSThR) and Korean Society of Radiology. Ultrasonography diagnosis and imaging-based management of thyroid nodules: revised Korean Society of Thyroid Radiology consensus statement and recommendations. Korean J Radiol. 2016; 17:370–395. PMID: 27134526.
Article15. Jung SL, Baek JH, Lee JH, Shong YK, Sung JY, Kim KS, et al. Efficacy and safety of radiofrequency ablation for benign thyroid nodules: a prospective multicenter study. Korean J Radiol. 2018; 19:167–174. PMID: 29354014.
Article16. Baek JH, Kim YS, Sung JY, Choi H, Lee JH. Locoregional control of metastatic well-differentiated thyroid cancer by ultrasound-guided radiofrequency ablation. AJR Am J Roentgenol. 2011; 197:W331–W336. PMID: 21785061.
Article17. Kim JH, Baek JH, Lim HK, Ahn HS, Baek SM, Choi YJ, et al. Guideline committee for the Korean Society of Thyroid Radiology (KSThR) and Korean Society of Radiology. 2017 thyroid radiofrequency ablation guideline: Korean Society of Thyroid Radiology. Korean J Radiol. 2018; 19:632–655. PMID: 29962870.
Article18. Na DG, Lee JH, Jung SL, Kim JH, Sung JY, Shin JH, et al. Korean Society of Thyroid Radiology (KSThR). Korean Society of Radiology. Radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers: consensus statement and recommendations. Korean J Radiol. 2012; 13:117–125. PMID: 22438678.
Article19. Baek JH, Kim YS, Lee D, Huh JY, Lee JH. Benign predominantly solid thyroid nodules: prospective study of efficacy of sonographically guided radiofrequency ablation versus control condition. AJR Am J Roentgenol. 2010; 194:1137–1142. PMID: 20308523.
Article20. Jeong WK, Baek JH, Rhim H, Kim YS, Kwak MS, Jeong HJ, et al. Radiofrequency ablation of benign thyroid nodules: safety and imaging follow-up in 236 patients. Eur Radiol. 2008; 18:1244–1250. PMID: 18286289.
Article21. Park HS, Baek JH, Park AW, Chung SR, Choi YJ, Lee JH. Thyroid radiofrequency ablation: updates on innovative devices and techniques. Korean J Radiol. 2017; 18:615–623. PMID: 28670156.
Article22. Ahmed M, Solbiati L, Brace CL, Breen DJ, Callstrom MR, Charboneau JW, et al. International Working Group on Image-Guided Tumor Ablation. Interventional Oncology Sans Frontières Expert Panel. Technology Assessment Committee of the Society of Interventional Radiology. Standard of Practice Committee of the Cardiovascular and Interventional Radiological Society of Europe. Image-guided tumor ablation: standardization of terminology and reporting criteria--a 10-year update. J Vasc Interv Radiol. 2014; 25:1691–1705.e4. PMID: 25442132.
Article23. Baek JH, Lee JH, Sung JY, Bae JI, Kim KT, Sim J, et al. Korean Society of Thyroid Radiology. Complications encountered in the treatment of benign thyroid nodules with US-guided radiofrequency ablation: a multicenter study. Radiology. 2012; 262:335–342. PMID: 21998044.
Article24. Mauri G, Cova L, Ierace T, Baroli A, Di Mauro E, Pacella CM, et al. Treatment of metastatic lymph nodes in the neck from papillary thyroid carcinoma with percutaneous laser ablation. Cardiovasc Intervent Radiol. 2016; 39:1023–1030. PMID: 26911732.
Article25. Persichetti A, Bizzarri G, Guglielmi R, Barnabei A, Bianchini A, Coccaro C, et al. Ultrasound-guided laser ablation for local control of neck recurrences of medullary thyroid cancer. A feasibility study. Int J Hyperthermia. 2018; 35:480–492. PMID: 30204004.
Article26. Mazzeo S, Cervelli R, Elisei R, Tarantini G, Cappelli C, Molinaro E, et al. mRECIST criteria to assess recurrent thyroid carcinoma treatment response after radiofrequency ablation: a prospective study. J Endocrinol Invest. 2018; 41:1389–1399. PMID: 29687416.
Article27. Suh CH, Baek JH, Choi YJ, Lee JH. Efficacy and safety of radiofrequency and ethanol ablation for treating locally recurrent thyroid cancer: a systematic review and meta-analysis. Thyroid. 2016; 26:420–428. PMID: 26782174.
Article28. Kim C, Lee JH, Choi YJ, Kim WB, Sung TY, Baek JH. Complications encountered in ultrasonography-guided radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers. Eur Radiol. 2017; 27:3128–3137. PMID: 27975148.
Article29. Chung SR, Suh CH, Baek JH, Park HS, Choi YJ, Lee JH. Safety of radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers: a systematic review and meta-analysis. Int J Hyperthermia. 2017; 33:920–930. PMID: 28565997.
Article30. Oda H, Miyauchi A, Ito Y, Yoshioka K, Nakayama A, Sasai H, et al. Incidences of unfavorable events in the management of low-risk papillary microcarcinoma of the thyroid by active surveillance versus immediate surgery. Thyroid. 2016; 26:150–155. PMID: 26426735.
Article31. Ito Y, Miyauchi A, Kihara M, Higashiyama T, Kobayashi K, Miya A. Patient age is significantly related to the progression of papillary microcarcinoma of the thyroid under observation. Thyroid. 2014; 24:27–34. PMID: 24001104.
Article32. Oh HS, Ha J, Kim HI, Kim TH, Kim WG, Lim DJ, et al. Active surveillance of low-risk papillary thyroid microcarcinoma: a multi-center cohort study in Korea. Thyroid. 2018; 28:1587–1594. PMID: 30226447.
Article33. Valcavi R, Piana S, Bortolan GS, Lai R, Barbieri V, Negro R. Ultrasound-guided percutaneous laser ablation of papillary thyroid microcarcinoma: a feasibility study on three cases with pathological and immunohistochemical evaluation. Thyroid. 2013; 23:1578–1582. PMID: 23978269.
Article34. Ma B, Wei W, Xu W, Wang Y, Guan H, Fan J, et al. Surgical confirmation of incomplete treatment for primary papillary thyroid carcinoma by percutaneous thermal ablation: a retrospective case review and literature review. Thyroid. 2018; 28:1134–1142. PMID: 29962285.
Article35. Zhan J, Ding H. Application of contrast-enhanced ultrasound for evaluation of thyroid nodules. Ultrasonography. 2018; 37:288–297. PMID: 30213158.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasound-guided radiofrequency ablation for the treatment of papillary thyroid carcinoma: a review of the current state and future perspectives
- A Review of Active Surveillance of Papillary Thyroid Microcarcinoma
- Comparison of Thermal Ablation and Surgery for Low-Risk Papillary Thyroid Microcarcinoma: A Systematic Review and Meta-Analysis
- Application of Radiofrequency Ablation to Thyroid Cancer: Past, Present, and Future
- RE: Management of Low-Risk Papillary Thyroid Microcarcinoma