Ann Dermatol.
2020 Apr;32(2):109-114. 10.5021/ad.2020.32.2.109.
Analysis of Adult Patients with Tinea Capitis in Southeastern Korea
- Affiliations
-
- 1Department of Dermatology, School of Medicine, Kyungpook National University, Kyungpook National University Hospital, Daegu, Korea. weonju@knu.ac.kr
- 2Institute of Medical Mycology, Catholic Skin Clinic, Daegu, Korea.
- KMID: 2471336
- DOI: http://doi.org/10.5021/ad.2020.32.2.109
Abstract
- BACKGROUND
Tinea capitis is a cutaneous infection of dermatophytes and predominant in children. Although tinea capitis in Korea is controlled by oral antifungal medications and concerted public health initiatives, it's still a health issue.
OBJECTIVE
To investigate changes in the epidemiological and mycological characteristics of adult patients with tinea capitis in southeastern Korea.
METHODS
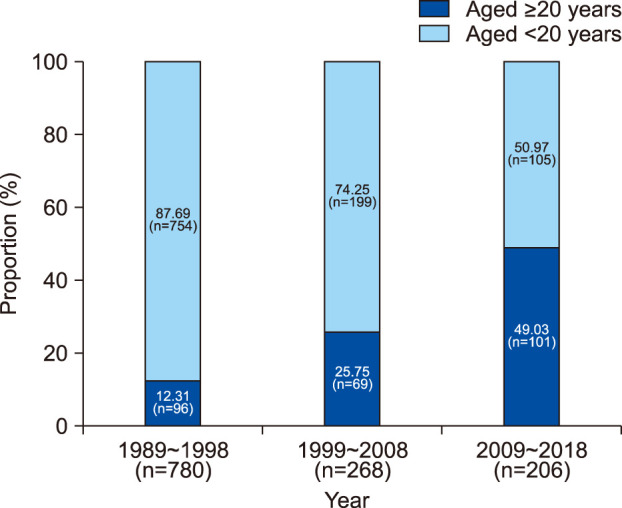
Using medical records from Kyungpook National University Hospital and Catholic Skin Clinic from 1989 to 2018, we retrospectively investigated the epidemiological and mycological characteristics of 266 adult patients (aged over 20) with tinea capitis.
RESULTS
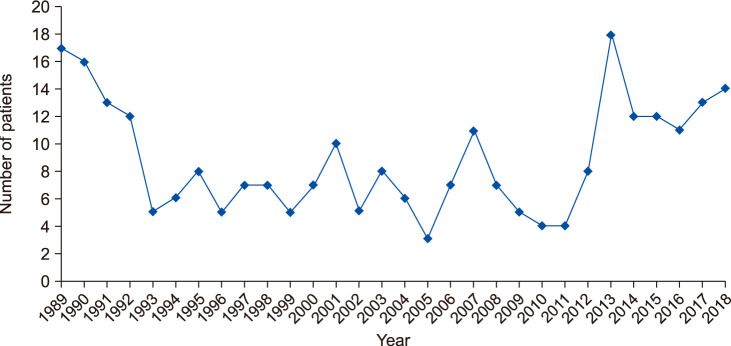
Among total 266 patients, 239 were KOH-positive. The annual incidence of tinea capitis ranged from 3 to 18 between 1989 and 2018. Of the total, 54 (20.30%) were male and 212 (79.70%) were female. Eighty patients (30.08%) were in their seventies, the most commonly affected age group. Of the remaining, 58 (21.80%) were in their sixties, and 41 (15.41%) in eighties. Among all, 77 (28.95%) visited the hospital in summer, 72 (27.07%) in spring, 64 (24.06%) in winter, and 53 (19.92%) in fall. Dermatophytes were cultured from 171 patients. Microsporum canis was the most common dermatophyte (42.48%), while Trichophyton rubrum was the second (15.79%). Of the 266 patients, 186 (69.92%) lived in urban areas and 80 (30.08%) in rural areas.
CONCLUSION
The epidemiological and mycological characteristics of adult patients with tinea capitis were different from those of children in terms of annual incidence, sex distribution, and isolated dermatophytes. These results provide useful information for the treatment and prevention of tinea capitis.
MeSH Terms
Figure
Reference
-
1. Michaels BD, Del Rosso JQ. Tinea capitis in infants: recognition, evaluation, and management suggestions. J Clin Aesthet Dermatol. 2012; 5:49–59.3. Hong JK. A supplementary study on tinea capitis in Taegu city. Korean J Dermatol. 1962; 2:7–14.4. Oh SH, Kim SH, Suh SB. Tinea capitis of adults in Taegu city for 11 years (1978~1988). Korean J Dermatol. 1989; 27:666–671.5. Kim SL, Lee KC, Jang YH, Lee SJ, Kim DW, Lee WJ, et al. The epidemiology of dermatophyte infection in Southeastern Korea (1979~2013). Ann Dermatol. 2016; 28:524–527. PMID: 27489448.
Article6. Cheon SJ, Lee JH, Lee YW, Park J, Suh MK, Kim H, et al. Epidemiology and identification of organisms causing superficial dermatomycoses at tertiary hospitals in Korea: a prospective multicenter study. J Mycol Infect. 2018; 23:45–53.7. Kim SM, Lee YW, Ahn KJ. A clinical and mycological study of tinea capitis. Korean J Med Mycol. 2006; 11:184–190.8. Shin DH, Kim KS, Kim KH. Clinical and mycologic studies of tinea capitis in Taegu. Korean J Med Mycol. 1998; 3:132–138.9. Chun IK, Lim MH, Lee SC, Won YH. Clinical and mycological studies of tinea capitis in Chonnam area (1986–1995). Korean J Med Mycol. 1996; 1:83–89.10. Kim SM, Kim YA, Cho NJ. A descriptive review of kerion and non-inflammatory tinea capitis. Korean J Dermatol. 2019; 57:182–190.11. Lee WJ, Kim SL, Jang YH, Lee SJ, Kim DW, Bang YJ, et al. Increasing prevalence of trichophyton rubrum identified through an analysis of 115,846 cases over the last 37 years. J Korean Med Sci. 2015; 30:639–643. PMID: 25931797.
Article12. Zhan P, Liu W. The changing face of dermatophytic infections worldwide. Mycopathologia. 2017; 182:77–86. PMID: 27783316.
Article13. Lee WJ, Sim HB, Jang YH, Lee SJ, Kim DW, Jun JB, et al. Skin infection due to Trichophyton tonsurans still occurs in people in Korea but not as outbreaks. J Korean Med Sci. 2016; 31:296–300. PMID: 26839486.
Article14. Cáceres-Ríos H, Rueda M, Ballona R, Bustamante B. Comparison of terbinafine and griseofulvin in the treatment of tinea capitis. J Am Acad Dermatol. 2000; 42(1 Pt 1):80–84. PMID: 10607324.15. López-Gómez S, Del Palacio A, Van Cutsem J, Soledad Cuétara M, Iglesias L, et al. Itraconazole versus griseofulvin in the treatment of tinea capitis: a double-blind randomized study in children. Int J Dermatol. 1994; 33:743–747. PMID: 8002149.
Article16. Jahangir M, Hussain I, Ul Hasan M, Haroon TS. A double-blind, randomized, comparative trial of itraconazole versus terbinafine for 2 weeks in tinea capitis. Br J Dermatol. 1998; 139:672–674. PMID: 9892912.
Article17. Gupta AK, Alexis ME, Raboobee N, Hofstader SL, Lynde CW, Adam P, et al. Itraconazole pulse therapy is effective in the treatment of tinea capitis in children: an open multicentre study. Br J Dermatol. 1997; 137:251–254. PMID: 9292075.
Article18. Gan VN, Petruska M, Ginsburg CM. Epidemiology and treatment of tinea capitis: ketoconazole vs. griseofulvin. Pediatr Infect Dis J. 1987; 6:46–49. PMID: 3822616.