Ann Hepatobiliary Pancreat Surg.
2020 Feb;24(1):24-32. 10.14701/ahbps.2020.24.1.24.
Long-term outcome of intraoperative radiofrequency ablation for hepatocellular carcinoma and its efficacy as a primary treatment
- Affiliations
-
- 1Department of Surgery, Chungnam National University Hospital, Daejeon, Korea. oxali@daum.net
- KMID: 2471185
- DOI: http://doi.org/10.14701/ahbps.2020.24.1.24
Abstract
- BACKGROUNDS/AIMS
We conducted this study to identify long-term outcomes following intraoperative radiofrequency ablation (IO-RFA) for hepatocellular carcinoma (HCC) and to reveal independent prognostic factors for survival.
METHODS
From December 1998 to February 2019, 183 patients underwent IO-RFA for HCC. These patients were divided into two groups according to whether RFA was done as a first-line (1-RFA group, n=106) or secondary-line (2-RFA group, n=77) treatment. Furthermore, we compared the survival outcomes between the 1-RFA and 2-RFA groups.
RESULTS
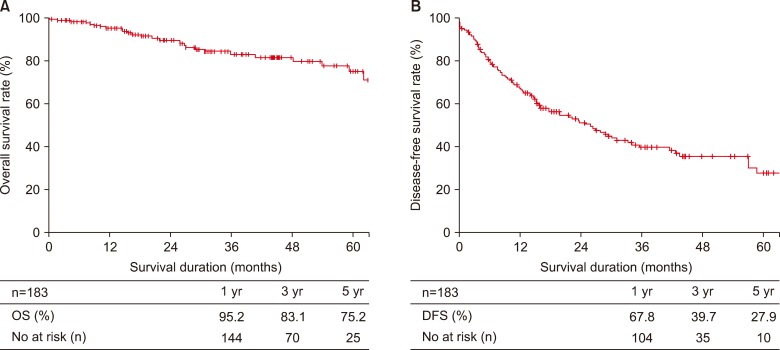
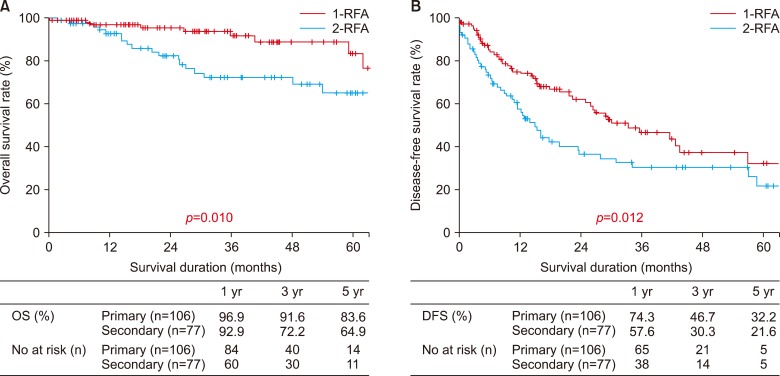
There were no significant differences in type of surgical approaches between the two groups (p=0.079). The number of tumors and largest tumor size were not significantly different between the two groups. Overall recurrence rate was 53%, and the 2-RFA group showed a higher recurrence rate (46.2% in 1-RFA group versus 62.3% in 2-RFA group; p=0.031). The 5-year overall survival (OS) and disease-free survival (DFS) rates of all the patients were 75.2% and 27.9%, respectively. The OS and DFS rates were significantly higher in the 1-RFA group. The 5-year OS rates were 83.6% and 64.9% in the 1-RFA and 2-RFA groups, respectively (p=0.010), whereas the 5-year DFS rates were 32.2% and 21.6%, respectively (p=0.012). On multivariate analysis, HBV-LC, 2-RFA, recurrence, and postoperative complications were independent predictive factors for survival.
CONCLUSIONS
Therapeutic outcomes of IO-RFA were comparable to those of surgical resection. Additionally, 1-RFA might be an alternative treatment for naïve HCC in patients with uncompensated liver function and severe comorbidities.
MeSH Terms
Figure
Reference
-
1. European Association for Study of Liver. European Organisation for Research and Treatment of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. Eur J Cancer. 2012; 48:599–641. PMID: 22424278.2. Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011; 61:69–90. PMID: 21296855.
Article3. Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014; 64:9–29. PMID: 24399786.
Article4. Sung PS, Yang H, Na GH, Hwang S, Kang D, Jang JW, et al. Long-term outcome of liver resection versus transplantation for hepatocellular carcinoma in a region where living donation is a main source. Ann Transplant. 2017; 22:276–284. PMID: 28473688.
Article5. Lencioni R, Cioni D, Crocetti L, Franchini C, Pina CD, Lera J, et al. Early-stage hepatocellular carcinoma in patients with cirrhosis: long-term results of percutaneous image-guided radiofrequency ablation. Radiology. 2005; 234:961–967. PMID: 15665226.
Article6. Georgiades CS, Hong K, Geschwind JF. Radiofrequency ablation and chemoembolization for hepatocellular carcinoma. Cancer J. 2008; 14:117–122. PMID: 18391617.
Article7. Xu Q, Kobayashi S, Ye X, Meng X. Comparison of hepatic resection and radiofrequency ablation for small hepatocellular carcinoma: a meta-analysis of 16,103 patients. Sci Rep. 2014; 4:7252. PMID: 25429732.
Article8. N'Kontchou G, Mahamoudi A, Aout M, Ganne-Carrié N, Grando V, Coderc E, et al. Radiofrequency ablation of hepatocellular carcinoma: long-term results and prognostic factors in 235 Western patients with cirrhosis. Hepatology. 2009; 50:1475–1483. PMID: 19731239.9. Lee DH, Lee JM, Lee JY, Kim SH, Yoon JH, Kim YJ, et al. Radiofrequency ablation of hepatocellular carcinoma as first-line treatment: long-term results and prognostic factors in 162 patients with cirrhosis. Radiology. 2014; 270:900–909. PMID: 24475823.
Article10. Kocabayoglu P, Piras-Straub K, Gerken G, Paul A, Herzer K. Expression of fibrogenic markers in tumor and tumor-surrounding tissue at time of transplantation correlates with recurrence of hepatocellular carcinoma in patients undergoing liver transplantation. Ann Transplant. 2017; 22:446–454. PMID: 28729525.
Article11. Cho JY, Choi MS, Lee GS, Sohn W, Ahn J, Sinn DH, et al. Clinical significance and predictive factors of early massive recurrence after radiofrequency ablation in patients with a single small hepatocellular carcinoma. Clin Mol Hepatol. 2016; 22:477–486. PMID: 28081587.
Article12. Meniconi RL, Komatsu S, Perdigao F, Boëlle PY, Soubrane O, Scatton O. Recurrent hepatocellular carcinoma: a Western strategy that emphasizes the impact of pathologic profile of the first resection. Surgery. 2015; 157:454–462. PMID: 25633732.13. Yim SY, Seo YS, Jung CH, Kim TH, Lee JM, Kim ES, et al. The management and prognosis of patients with hepatocellular carcinoma: what has changed in 20 years? Liver Int. 2016; 36:445–453. PMID: 26352789.
Article14. Hong SN, Lee SY, Choi MS, Lee JH, Koh KC, Paik SW, et al. Comparing the outcomes of radiofrequency ablation and surgery in patients with a single small hepatocellular carcinoma and well-preserved hepatic function. J Clin Gastroenterol. 2005; 39:247–252. PMID: 15718869.
Article15. Livraghi T, Meloni F, Di Stasi M, Rolle E, Solbiati L, Tinelli C, et al. Sustained complete response and complications rates after radiofrequency ablation of very early hepatocellular carcinoma in cirrhosis: is resection still the treatment of choice? Hepatology. 2008; 47:82–89. PMID: 18008357.
Article16. Hung HH, Chiou YY, Hsia CY, Su CW, Chou YH, Chiang JH, et al. Survival rates are comparable after radiofrequency ablation or surgery in patients with small hepatocellular carcinomas. Clin Gastroenterol Hepatol. 2011; 9:79–86. PMID: 20831902.
Article17. Pompili M, Saviano A, de Matthaeis N, Cucchetti A, Ardito F, Federico B, et al. Long-term effectiveness of resection and radiofrequency ablation for single hepatocellular carcinoma ≤3 cm. Results of a multicenter Italian survey. J Hepatol. 2013; 59:89–97. PMID: 23523578.18. Imai K, Beppu T, Chikamoto A, Doi K, Okabe H, Hayashi H, et al. Comparison between hepatic resection and radiofrequency ablation as first-line treatment for solitary small-sized hepatocellular carcinoma of 3 cm or less. Hepatol Res. 2013; 43:853–864. PMID: 23281579.19. Zhou Z, Lei J, Li B, Yan L, Wang W, Wei Y, et al. Liver resection and radiofrequency ablation of very early hepatocellular carcinoma cases (single nodule <2 cm): a single-center study. Eur J Gastroenterol Hepatol. 2014; 26:339–344. PMID: 24150522.20. Ng KKC, Chok KSH, Chan ACY, Cheung TT, Wong TCL, Fung JYY, et al. Randomized clinical trial of hepatic resection versus radiofrequency ablation for early-stage hepatocellular carcinoma. Br J Surg. 2017; 104:1775–1784. PMID: 29091283.
Article21. Peng ZW, Lin XJ, Zhang YJ, Liang HH, Guo RP, Shi M, et al. Radiofrequency ablation versus hepatic resection for the treatment of hepatocellular carcinomas 2 cm or smaller: a retrospective comparative study. Radiology. 2012; 262:1022–1033. PMID: 22357902.
Article22. Wang JH, Wang CC, Hung CH, Chen CL, Lu SN. Survival comparison between surgical resection and radiofrequency ablation for patients in BCLC very early/early stage hepatocellular carcinoma. J Hepatol. 2012; 56:412–428. PMID: 21756858.
Article23. Liu PH, Hsu CY, Hsia CY, Lee YH, Huang YH, Chiou YY, et al. Surgical resection versus radiofrequency ablation for single hepatocellular carcinoma ≤ 2 cm in a propensity score model: erratum. Ann Surg. 2016; 263:e77. Erratum for: Ann Surg 2016;263:538–545. PMID: 27058857.24. Clinical practice guidelines for hepatocellular carcinoma differ between Japan, United States, and Europe. Liver Cancer. 2015; 4:85–95. PMID: 26020031.25. Cucchetti A, Cescon M, Bigonzi E, Piscaglia F, Golfieri R, Ercolani G, et al. Priority of candidates with hepatocellular carcinoma awaiting liver transplantation can be reduced after successful bridge therapy. Liver Transpl. 2011; 17:1344–1354. PMID: 21837731.
Article26. Cucchetti A, Mazzaferro V, Pinna AD, Sposito C, Golfieri R, Serra C, et al. Average treatment effect of hepatic resection versus locoregional therapies for hepatocellular carcinoma. Br J Surg. 2017; 104:1704–1712. PMID: 28745399.
Article27. Fontana RJ, Hamidullah H, Nghiem H, Greenson JK, Hussain H, Marrero J, et al. Percutaneous radiofrequency thermal ablation of hepatocellular carcinoma: a safe and effective bridge to liver transplantation. Liver Transpl. 2002; 8:1165–1174. PMID: 12474157.
Article28. Pompili M, Mirante VG, Rondinara G, Fassati LR, Piscaglia F, Agnes S, et al. Percutaneous ablation procedures in cirrhotic patients with hepatocellular carcinoma submitted to liver transplantation: assessment of efficacy at explant analysis and of safety for tumor recurrence. Liver Transpl. 2005; 11:1117–1126. PMID: 16123960.
Article29. Mazzaferro V, Battiston C, Perrone S, Pulvirenti A, Regalia E, Romito R, et al. Radiofrequency ablation of small hepatocellular carcinoma in cirrhotic patients awaiting liver transplantation: a prospective study. Ann Surg. 2004; 240:900–909. PMID: 15492574.30. Lam A, Yoshida EJ, Bui K, Katrivesis J, Fernando D, Nelson K, et al. Demographic and facility volume related outcomes in radiofrequency ablation for early-stage hepatocellular carcinoma. HPB (Oxford). 2019; 21:849–856. PMID: 30518497.
Article31. Lee HJ, Kim JW, Hur YH, Cho SB, Lee BC, Lee BK, et al. Conventional chemoembolization plus radiofrequency ablation versus surgical resection for single, medium-sized hepatocellular carcinoma: propensity-score matching analysis. J Vasc Interv Radiol. 2019; 30:284–292.e1. PMID: 30819467.
Article32. Chen L, Zhang Q, Chang W, Du Y, Zhang H, Cao G. Viral and host inflammation-related factors that can predict the prognosis of hepatocellular carcinoma. Eur J Cancer. 2012; 48:1977–1987. PMID: 22325840.
Article33. Yin J, Li N, Han Y, Xue J, Deng Y, Shi J, et al. Effect of antiviral treatment with nucleotide/nucleoside analogs on postoperative prognosis of hepatitis B virus-related hepatocellular carcinoma: a two-stage longitudinal clinical study. J Clin Oncol. 2013; 31:3647–3655. PMID: 24002499.
Article34. Wong JS, Wong GL, Tsoi KK, Wong VW, Cheung SY, Chong CN, et al. Meta-analysis: the efficacy of anti-viral therapy in prevention of recurrence after curative treatment of chronic hepatitis B-related hepatocellular carcinoma. Aliment Pharmacol Ther. 2011; 33:1104–1112. PMID: 21488914.
Article35. Miao RY, Zhao HT, Yang HY, Mao YL, Lu X, Zhao Y, et al. Postoperative adjuvant antiviral therapy for hepatitis B/C virus-related hepatocellular carcinoma: a meta-analysis. World J Gastroenterol. 2010; 16:2931–2942. PMID: 20556841.
Article36. Shiina S, Tateishi R, Arano T, Uchino K, Enooku K, Nakagawa H, et al. Radiofrequency ablation for hepatocellular carcinoma: 10-year outcome and prognostic factors. Am J Gastroenterol. 2012; 107:569–577. PMID: 22158026.
Article37. El-Fattah MA, Aboelmagd M, Elhamouly M. Prognostic factors of hepatocellular carcinoma survival after radiofrequency ablation: a US population-based study. United European Gastroenterol J. 2017; 5:227–235.38. Sparchez Z, Mocan T, Radu P, Mocan LP, Sparchez M, Leucuta DC, et al. Prognostic factors after percutaneous radiofrequency ablation in the treatment of hepatocellular carcinoma. Impact of incomplete ablation on recurrence and overall survival rates. J Gastrointestin Liver Dis. 2018; 27:399–407. PMID: 30574622.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current status and future of radiofrequency ablation for hepatocellular carcinoma
- The Role of Combination of Transarterial Chemoebolization and Radiofrequency Ablation for Hepatocellular Carcinoma Treatment
- Chemoembolization combined with radiofrequency ablation is the best option for the local treatment of early hepatocellular carcinoma?
- Microwave thermosphere versus radiofrequency ablation for hepatocellular carcinoma: Are we approaching the time to end the debate?
- Recent advance of local ablation for hepatocellular carcinoma