J Korean Assoc Oral Maxillofac Surg.
2013 Aug;39(4):182-187.
Expansile keratocystic odontogenic tumor in the maxilla: immunohistochemical studies and review of literature
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Institute of Health Science, Gyeongsang National University School of Medicine, Jinju, Korea. parkbw@gnu.ac.kr
Abstract
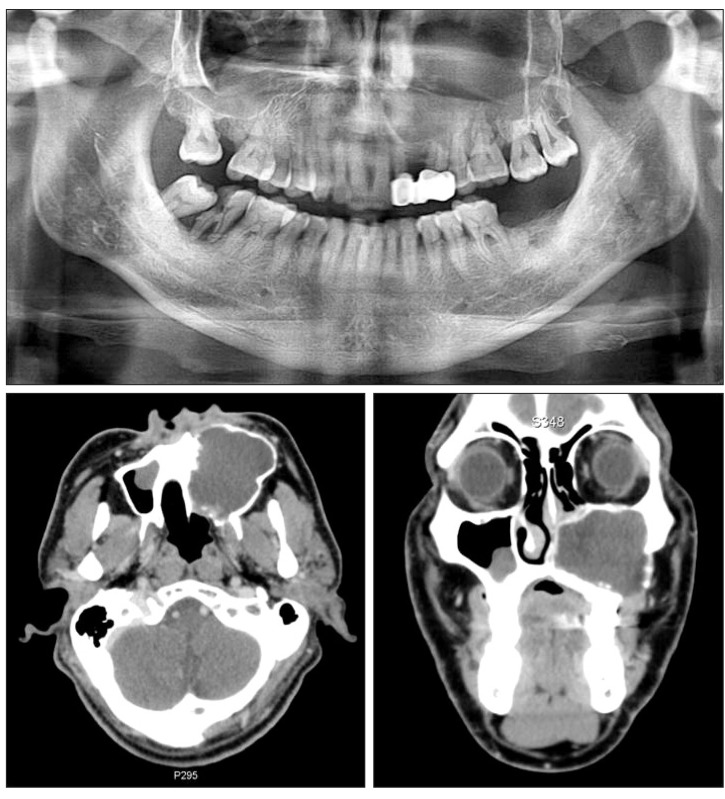
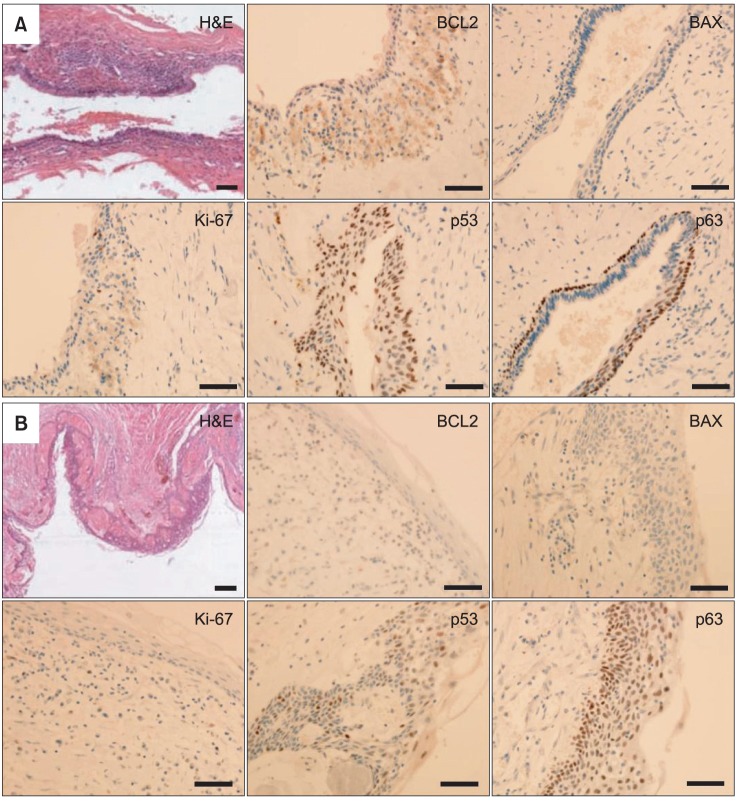
- Keratocystic odontogenic tumors (KCOT) - previously termed odontogenic keratocysts (OKC) - are characterized by aggressive behavior and a high rate of recurrence. Histopathologically, the basal layer of KCOT shows a higher cell proliferation rate and increased expression of anti-apoptosis genes. Clinically, KCOT is frequently involved in the mandibular posterior region but is not common in the posterior maxilla. However, it should be noted that due to its expansive characteristics, KCOT involved near the maxillary sinus could easily expand to an enormous size and occupy the entire maxilla. To achieve total excision of these expanded cystic tumors in the maxilla, a more aggressive approach would be needed. In this report, we describe two cases of expansile KCOT involving the entire unilateral maxilla and maxillary sinus; they were completely excised using the Weber-Ferguson approach, showing no evidence of recurrence during the follow-up period of more than two years. In immunohistochemical analyses of the tumor specimens, p53 and p63 showed strong expression, and B-cell lymphoma 2 (BCL2) and MKI67 (Ki-67) showed moderate or weak expression, however, detection of BCL2-associated X protein (BAX) was almost negative. These data indicate that expansile KCOT possesses increased anti-apoptotic activity and cell proliferation rate but decreased apoptosis. These properties of KCOT may contribute to tumor enlargement, aggressive behavior, and high recurrence rate.
MeSH Terms
Figure
Reference
-
1. Bhargava D, Deshpande A, Pogrel MA. Keratocystic odontogenic tumour (KCOT)--a cyst to a tumour. Oral Maxillofac Surg. 2012; 16:163–170. PMID: 22072419.
Article2. Barnes L, Eveson JW, Reichart P, Sidransky D. World Health Organization classification of tumors: pathology and genetics of head and neck tumours. Lyon: IARC Publishing Group;2005. p. 306–307.3. Habibi A, Saghravanian N, Habibi M, Mellati E, Habibi M. Keratocystic odontogenic tumor: a 10-year retrospective study of 83 cases in an Iranian population. J Oral Sci. 2007; 49:229–235. PMID: 17928730.
Article4. Stoelinga PJ. Etiology and pathogenesis of keratocysts. Oral Maxillofac Surg Clin North Am. 2003; 15:317–324. PMID: 18088685.
Article5. Shear M. The aggressive nature of the odontogenic keratocyst: is it a benign cystic neoplasm? Part 2. Proliferation and genetic studies. Oral Oncol. 2002; 38:323–331. PMID: 12076694.6. Eryilmaz T, Ozmen S, Findikcioglu K, Kandal S, Aral M. Odontogenic keratocyst: an unusual location and review of the literature. Ann Plast Surg. 2009; 62:210–212. PMID: 19158536.7. Neville BW, Damn DD, Allen CM, Bouquout JE. Oral and maxillofacial pathology. 3rd ed. Philadelphia: Saunders;2009.8. Lo Muzio L, Santarelli A, Caltabiano R, Rubini C, Pieramici T, Fior A, et al. p63 expression in odontogenic cysts. Int J Oral Maxillofac Surg. 2005; 34:668–673. PMID: 16053892.
Article9. Gurgel CA, Ramos EA, Azevedo RA, Sarmento VA, da Silva Carvalho AM, dos Santos JN. Expression of Ki-67, p53 and p63 proteins in keratocyst odontogenic tumours: an immunohistochemical study. J Mol Histol. 2008; 39:311–316. PMID: 18256893.
Article10. Mendes RA, Carvalho JF, van der Waal I. A comparative immunohistochemical analysis of COX-2, p53, and Ki-67 expression in keratocystic odontogenic tumors. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011; 111:333–339. PMID: 21215666.
Article11. Gonçalves CK, Fregnani ER, Leon JE, Silva-Sousa YT, Perez DE. Immunohistochemical expression of p63, epidermal growth factor receptor (EGFR) and notch-1 in radicular cysts, dentigerous cysts and keratocystic odontogenic tumors. Braz Dent J. 2012; 23:337–343. PMID: 23207846.
Article12. Gadbail AR, Patil R, Chaudhary M. Co-expression of Ki-67 and p53 protein in ameloblastoma and keratocystic odontogenic tumor. Acta Odontol Scand. 2012; 70:529–535. PMID: 21780975.
Article13. Soluk Tekkeşın M, Mutlu S, Olgaç V. Expressions of bax, bcl-2 and Ki-67 in odontogenic keratocysts (keratocystic odontogenic tumor) in comparison with ameloblastomas and radicular cysts. Turk Patoloji Derg. 2012; 28:49–55. PMID: 22207432.14. de Oliveira MG, Lauxen Ida S, Chaves AC, Rados PV, Sant'Ana Filho M. Immunohistochemical analysis of the patterns of p53 and PCNA expression in odontogenic cystic lesions. Med Oral Patol Oral Cir Bucal. 2008; 13:E275–E280. PMID: 18449109.15. Sikes JW Jr, Ghali GE, Troulis MJ. Expansile intraosseous lesion of the maxilla. J Oral Maxillofac Surg. 2000; 58:1395–1400. PMID: 11117688.
Article16. Cho JY, Nam KY. Expansile dentigerous cyst invading the entire maxillary sinus: a case report. J Korean Assoc Oral Maxillofac Surg. 2012; 38:245–248.
Article17. Kim SG, Park CY, Kang TH, Jang HS. Clinicopathologic study on cysts and postoperative cyst in maxillary sinus. J Korean Assoc Maxillofac Plast Reconstr Surg. 2000; 22:568–576.18. Albright CR, Hennig GH. Large dentigerous cyst of the maxilla near the maxillary sinus: report of case. J Am Dent Assoc. 1971; 83:1112–1115. PMID: 5286148.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Odontogenic fibromyxoma: A Case Report
- Analysis of Keratocystic Odontogenic Tumor
- Enucleation of large keratocystic odontogenic tumor at mandible via unilateral sagittal split osteotomy: a report of three cases
- A Case of Squamous Cell Carcinoma arising from an Odontogenic Keratocyst
- Central Odontogenic Fibroma in Anterior Maxilla: A Case Report