Investig Clin Urol.
2020 Mar;61(2):224-230. 10.4111/icu.2020.61.2.224.
Scrotal septum detachment during penile plication to compensate for loss of penile length compared with conventional surgical technique
- Affiliations
-
- 1Department of Urology, Korea University Guro Hospital, Seoul, Korea. dgmoon@korea.ac.kr
- KMID: 2471079
- DOI: http://doi.org/10.4111/icu.2020.61.2.224
Abstract
- PURPOSE
To evaluate the efficacy and safety of penile elongation featuring simple scrotal septum detachment from the penile base to compensate for the loss of penile length during penile plication in patients with Peyronie's disease compared with conventional penile plication.
MATERIALS AND METHODS
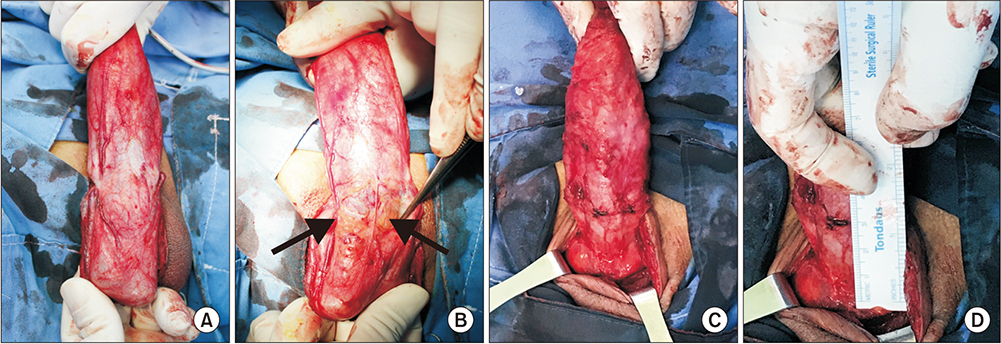
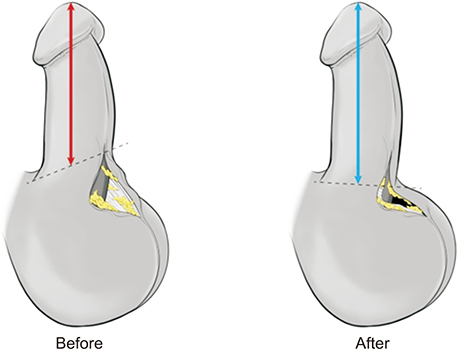
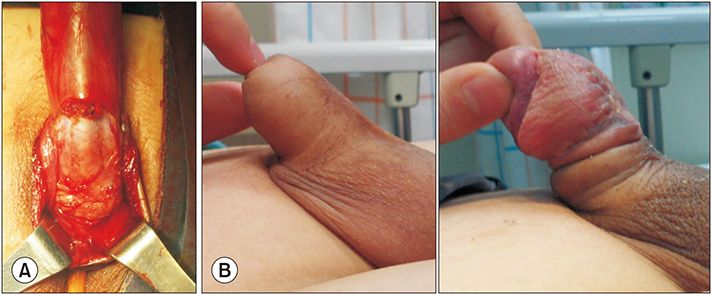
We conducted a retrospective analysis of 38 patients (24-75 years of age) with Peyronie's disease who underwent penile plication with or without our novel technique from January 2009 to May 2018. Penile elongation was achieved by release and detachment of the scrotal septum from the penile base to the level of the scrotal fat tissue. The objective outcome of change in stretched penile length (SPL) and the subjective outcome of patient perception of postoperative penile length were compared between groups. Any postoperative complications were recorded.
RESULTS
Of the 38 patients, 16 underwent penile plication with scrotal septum detachment (elongation group) and 22 underwent penile plication only (conventional group). The postoperative mean SPL was increased in the elongation group and decreased in the conventional group (1.2±1.3 cm vs. −0.5±0.3 cm, p<0.001). Fourteen of 16 patients (87.5%) in the elongation group reported perceived penile lengthening after surgery, whereas 17/22 patients (77.3%) in the conventional group complained of penile shortening. We encountered no procedure-related complications such as hematoma, infection, or necrosis in either group.
CONCLUSIONS
Simple detachment of the scrotal septum from the penile base afforded both objective and subjective penile elongation without any severe complications compared with conventional penile plication.
Keyword
MeSH Terms
Figure
Reference
-
1. Mulhall JP, Schiff J, Guhring P. An analysis of the natural history of Peyronie's disease. J Urol. 2006; 175:2115–2118. discussion 2118.
Article2. Nelson CJ, Diblasio C, Kendirci M, Hellstrom W, Guhring P, Mulhall JP. The chronology of depression and distress in men with Peyronie's disease. J Sex Med. 2008; 5:1985–1990.
Article3. Tan RB, Sangkum P, Mitchell GC, Hellstrom WJ. Update on medical management of Peyronie's disease. Curr Urol Rep. 2014; 15:415.
Article4. Ralph D, Gonzalez-Cadavid N, Mirone V, Perovic S, Sohn M, Usta M, et al. The management of Peyronie's disease: evidencebased 2010 guidelines. J Sex Med. 2010; 7:2359–2374.
Article5. Gholami SS, Lue TF. Correction of penile curvature using the 16-dot plication technique: a review of 132 patients. J Urol. 2002; 167:2066–2069.
Article6. Shin SH, Jeong HG, Park JJ, Chae JY, Kim JW, Oh MM, et al. The outcome of multiple slit on plaque with plication technique for the treatment of Peyronie's disease. World J Mens Health. 2016; 34:20–27.
Article7. Mobley EM, Fuchs ME, Myers JB, Brant WO. Update on plication procedures for Peyronie's disease and other penile deformities. Ther Adv Urol. 2012; 4:335–346.
Article8. Chung E. Penile reconstructive surgery in peyronie disease: challenges in restoring normal penis size, shape, and function. World J Mens Health. 2020; 38:1–8.
Article9. Dugi DD 3rd, Morey AF. Penoscrotal plication as a uniform approach to reconstruction of penile curvature. BJU Int. 2010; 105:1440–1444.
Article10. Chung PH, Tausch TJ, Simhan J, Scott JF, Morey AF. Dorsal plication without degloving is safe and effective for correcting ventral penile deformities. Urology. 2014; 84:1228–1233.
Article11. Adibi M, Hudak SJ, Morey AF. Penile plication without degloving enables effective correction of complex Peyronie's deformities. Urology. 2012; 79:831–835.
Article12. Dwyer ME, Salgado CJ, Lightner DJ. Normal penile, scrotal, and perineal anatomy with reconstructive considerations. Semin Plast Surg. 2011; 25:179–188.
Article13. Hoznek A, Rahmouni A, Abbou C, Delmas V, Colombel M. The suspensory ligament of the penis: an anatomic and radiologic description. Surg Radiol Anat. 1998; 20:413–417.
Article14. Cimador M, Catalano P, Ortolano R, Giuffrè M. The inconspicuous penis in children. Nat Rev Urol. 2015; 12:205–215.
Article15. Campbell J, Gillis J. A review of penile elongation surgery. Transl Androl Urol. 2017; 6:69–78.
Article16. Li CY, Kayes O, Kell PD, Christopher N, Minhas S, Ralph DJ. Penile suspensory ligament division for penile augmentation: indications and results. Eur Urol. 2006; 49:729–733.
Article17. Wessells H, Lue TF, McAninch JW. Complications of penile lengthening and augmentation seen at 1 referral center. J Urol. 1996; 155:1617–1620.
Article18. Alter GJ, Jordan GH. Penile elongation and girth enhancement. AUA Update Series. 2007; 26:229–237.19. Vardi Y, Har-Shai Y, Gil T, Gruenwald I. A critical analysis of penile enhancement procedures for patients with normal penile size: surgical techniques, success, and complications. Eur Urol. 2008; 54:1042–1050.
Article20. Schneider T, Sperling H, Schenck M, Schneider U, Rübben H. Treatment of penile curvature--how to combine the advantages of simple plication and the Nesbit-procedure by superficial excision of the tunica albuginea. World J Urol. 2003; 20:350–355.
Article21. Van Der Horst C, Martínez Portillo FJ, Seif C, Alken P, Juenemann KP. Treatment of penile curvature with Essed-Schröder tunical plication: aspects of quality of life from the patients' perspective. BJU Int. 2004; 93:105–108.22. Syed AH, Abbasi Z, Hargreave TB. Nesbit procedure for disabling Peyronie's curvature: a median follow-up of 84 months. Urology. 2003; 61:999–1003.
Article23. Sokolakis I, Schönbauer P, Mykoniatis I, Kübler H, Gschwend J, Lahme S, et al. Long-term results after surgical treatment of congenital penile curvature using a modified nesbit technique. World J Mens Health. 2019; 09. 04. DOI: 10.5534/wjmh.190092. [Epub].
Article24. Hudak SJ, Morey AF, Adibi M, Bagrodia A. Favorable patient reported outcomes after penile plication for wide array of peyronie disease abnormalities. J Urol. 2013; 189:1019–1024.
Article25. Taylor FL, Levine LA. Surgical correction of Peyronie's disease via tunica albuginea plication or partial plaque excision with pericardial graft: long-term follow up. J Sex Med. 2008; 5:2221–2228.
Article26. Tal R, Nabulsi O, Nelson CJ, Mulhall JP. The psychosocial impact of penile reconstructive surgery for congenital penile deviation. J Sex Med. 2010; 7(1 Pt 1):121–128.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Penile Resurfacing after Removal of Penile Foreign Body Granuloma
- The Outcome of Multiple Slit on Plaque with Plication Technique for the Treatment of Peyronie's Disease
- Penile Reconstructive Surgery in Peyronie Disease: Challenges in Restoring Normal Penis Size, Shape, and Function
- Penile paraffinoma: 39 cases
- A Case Report of Total Penile Skin Graft