J Lipid Atheroscler.
2020 Jan;9(1):205-229. 10.12997/jla.2020.9.1.205.
Associations of Dietary Intake with Cardiovascular Disease, Blood Pressure, and Lipid Profile in the Korean Population: a Systematic Review and Meta-Analysis
- Affiliations
-
- 1Department of Cancer Biomedical Science, National Cancer Center Graduate School of Cancer Science and Policy, Goyang, Korea. jskim@ncc.re.kr
- 2Department of Food and Nutrition, Daegu University, Gyeongsan, Korea.
- 3Food and Nutrition Major, Division of Food Science and Culinary Arts, Shinhan University, Uijeongbu, Korea.
- 4Department of Food and Nutrition, Keimyung University, Daegu, Korea.
- 5Department of Food and Nutrition, Kyungnam University, Changwon, Korea.
- 6Department of Food and Nutrition, Yonsei University, Seoul, Korea.
- 7Department of Food and Nutrition, Hannam University, Daejeon, Korea.
- 8Dietetics and Nutrition Services Team, Asan Medical Center, Seoul, Korea.
- 9Nutrition Support Team, Kyung Hee University Medical Center, Seoul, Korea.
- 10Clinical Nutrition Part, Samsung Medical Center, Seoul, Korea.
- KMID: 2470812
- DOI: http://doi.org/10.12997/jla.2020.9.1.205
Abstract
OBJECTIVE
Previous studies have separately reported the contributions of dietary factors to the risk of cardiovascular disease (CVD) and its markers, including blood pressure (BP) and lipid profile. This study systematically reviewed the current evidence on this issue in the Korean population.
METHODS
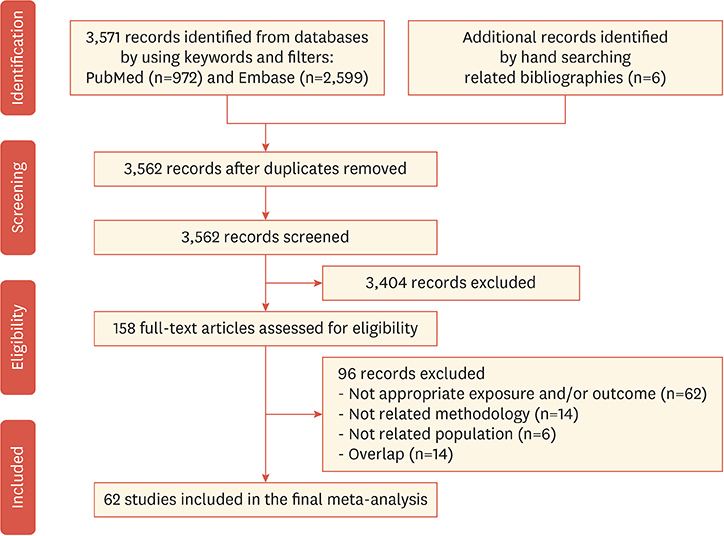
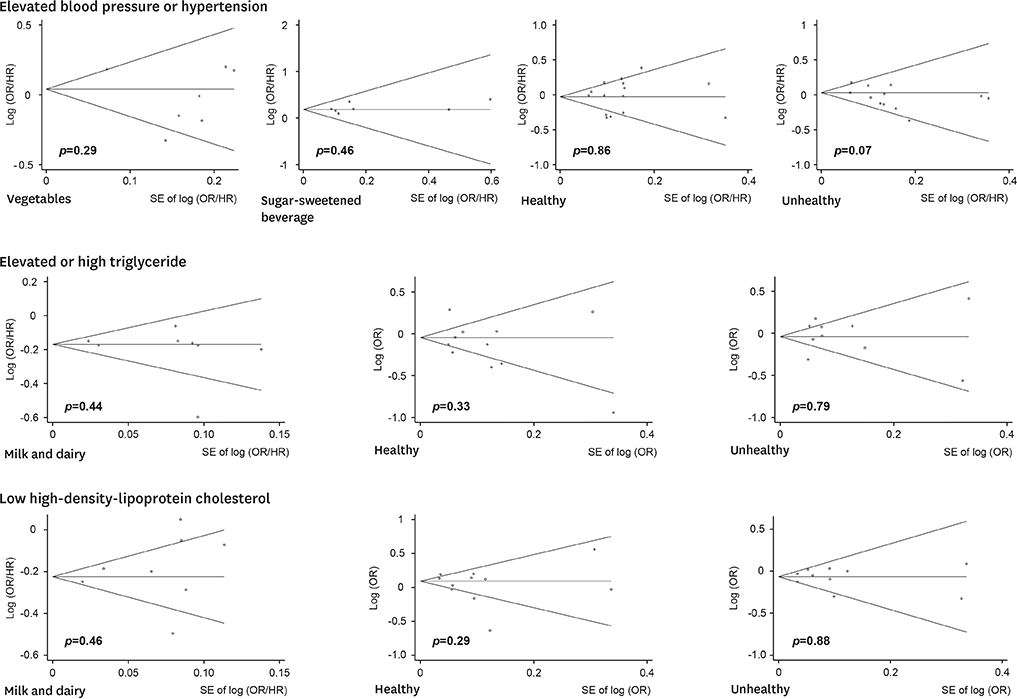
Sixty-two studies from PubMed and Embase were included in this meta-analysis. We performed a random-effects model to analyze pooled odds ratios (ORs) and hazard ratios (HRs) and their 95% confidence intervals (CIs) for the consumption of 14 food items, three macro- and eight micro-nutrients, two dietary patterns, and three dietary indices.
RESULTS
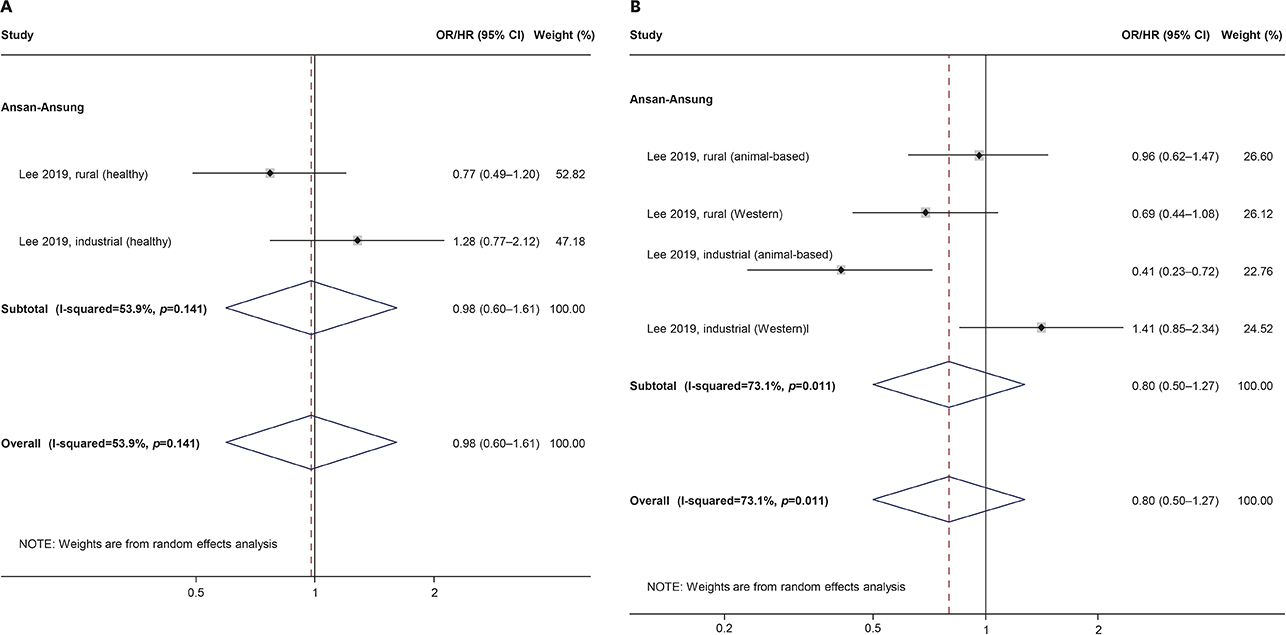
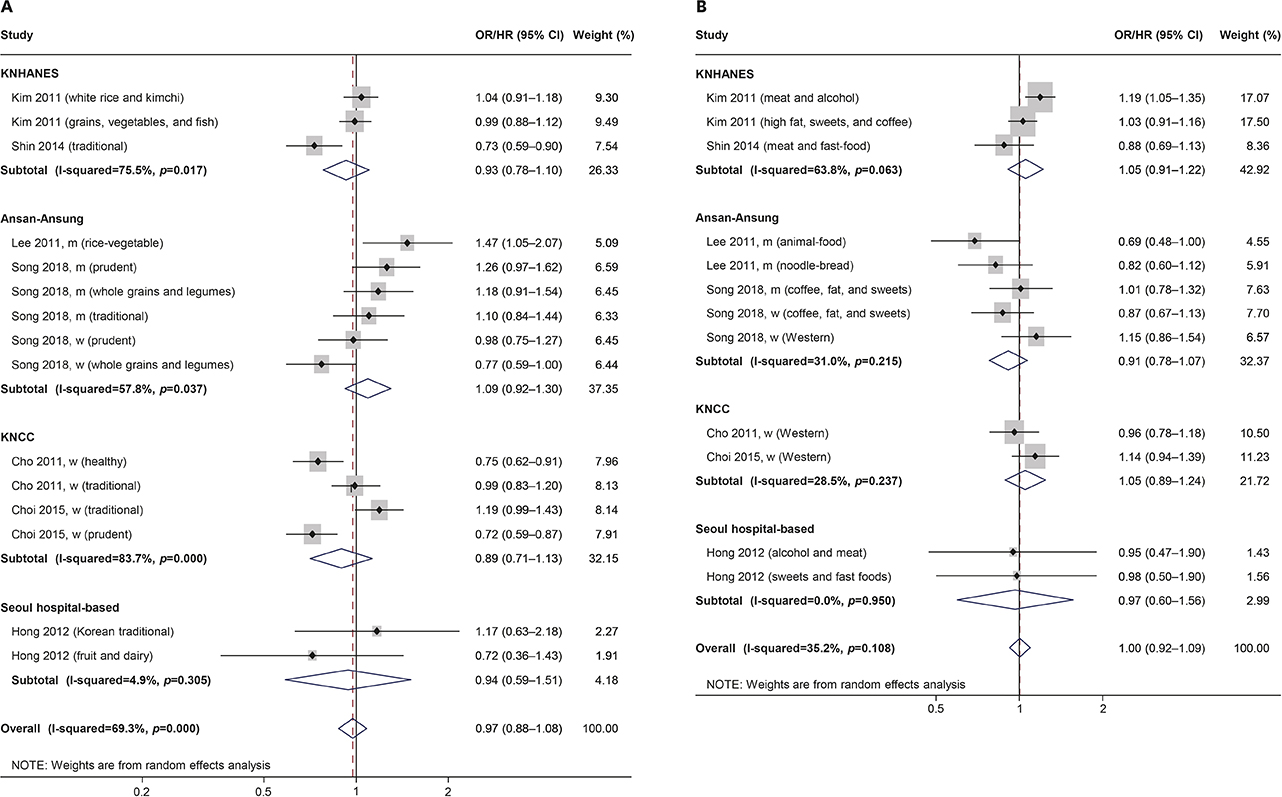
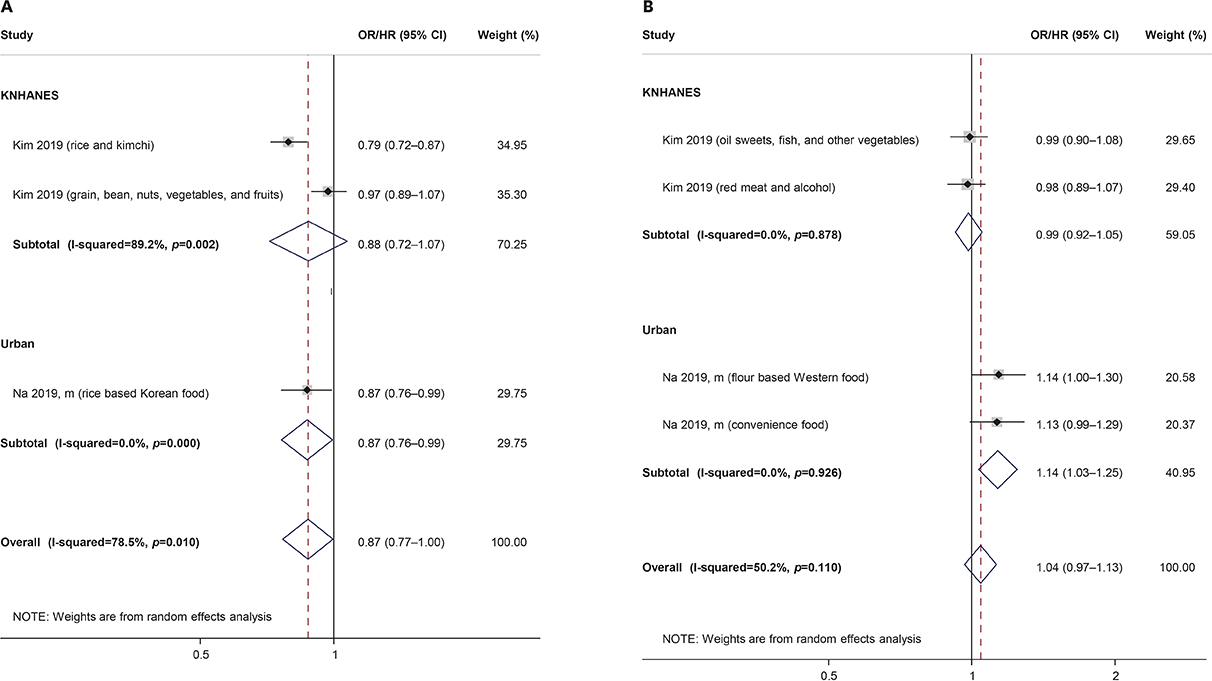
An analysis of pooled effect sizes from at least four individual study populations showed significant associations between coffee consumption and CVD (OR/HR, 0.71; 95% CI, 0.52-0.97) and elevated/high triglycerides (TG) (OR, 0.84; 95% CI, 0.78-0.90), sugar-sweetened beverage intake and elevated BP (OR/HR, 1.20; 95% CI, 1.09-1.33), and milk and dairy intake and elevated/high TG and low high-density lipoprotein cholesterol (HDL-C) (OR/HR, 0.82; 95% CI, 0.76-0.89 for both). Carbohydrate consumption and the low-carbohydrate-diet score were consistently related to an approximately 25% risk reduction for elevated TG and low HDL-C. A lower risk of elevated total cholesterol, but not low-density lipoprotein, was additionally observed for those with a higher low-carbohydrate-diet score. A healthy dietary pattern was only associated with a reduced risk of elevated TG in the Korea National Cancer Screenee Cohort (OR, 0.81; 95% CI, 0.67-0.98).
CONCLUSION
This study showed that milk and dairy and coffee had protective effects for CVD and its risk factors, such as BP and lipid profile, while sugar-sweetened beverages exerted harmful effects.
Keyword
MeSH Terms
Figure
Reference
-
1. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018; 392:1789–1858.2. GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017; 390:1151–1210.3. Roth GA, Huffman MD, Moran AE, Feigin V, Mensah GA, Naghavi M, et al. Global and regional patterns in cardiovascular mortality from 1990 to 2013. Circulation. 2015; 132:1667–1678.
Article4. Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. 2017; 70:1–25.5. Lee SW, Kim HC, Lee HS, Suh I. Thirty-year trends in mortality from cardiovascular diseases in Korea. Korean Circ J. 2015; 45:202–209.
Article6. Bhatnagar A. Environmental determinants of cardiovascular disease. Circ Res. 2017; 121:162–180.
Article7. Kim HC, Oh SM. Noncommunicable diseases: current status of major modifiable risk factors in Korea. J Prev Med Public Health. 2013; 46:165–172.
Article8. Bromfield S, Muntner P. High blood pressure: the leading global burden of disease risk factor and the need for worldwide prevention programs. Curr Hypertens Rep. 2013; 15:134–136.
Article9. Miller M. Dyslipidemia and cardiovascular risk: the importance of early prevention. QJM. 2009; 102:657–667.
Article10. Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004; 364:937–952.
Article11. Peters SAE, Wang X, Lam TH, Kim HC, Ho S, Ninomiya T, et al. Clustering of risk factors and the risk of incident cardiovascular disease in Asian and Caucasian populations: results from the Asia Pacific Cohort Studies Collaboration. BMJ Open. 2018; 8:e019335.
Article12. Jee SH, Jang Y, Oh DJ, Oh BH, Lee SH, Park SW, et al. A coronary heart disease prediction model: the Korean Heart Study. BMJ Open. 2014; 4:e005025.
Article13. Kim HJ, Kim Y, Cho Y, Jun B, Oh KW. Trends in the prevalence of major cardiovascular disease risk factors among Korean adults: results from the Korea National Health and Nutrition Examination Survey, 1998–2012. Int J Cardiol. 2014; 174:64–72.
Article14. Kokubo Y. Prevention of hypertension and cardiovascular diseases: a comparison of lifestyle factors in Westerners and East Asians. Hypertension. 2014; 63:655–660.
Article15. Siri-Tarino PW, Krauss RM. Diet, lipids, and cardiovascular disease. Curr Opin Lipidol. 2016; 27:323–328.
Article16. Anand SS, Hawkes C, de Souza RJ, Mente A, Dehghan M, Nugent R, et al. Food consumption and its impact on cardiovascular disease: importance of solutions focused on the globalized food system: a report from the workshop convened by the World Heart Federation. J Am Coll Cardiol. 2015; 66:1590–1614.
Article17. Lee HY, Shin J, Kim GH, Park S, Ihm SH, Kim HC, et al. 2018 Korean Society of Hypertension Guidelines for the management of hypertension: part II-diagnosis and treatment of hypertension. Clin Hypertens. 2019; 25:20.
Article18. Rhee EJ, Kim HC, Kim JH, Lee EY, Kim BJ, Kim EM, et al. 2018 Guidelines for the management of dyslipidemia in Korea. Korean J Intern Med. 2019; 34:1171.
Article19. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009; 6:e1000100.
Article20. Eriksen MB, Frandsen TF. The impact of patient, intervention, comparison, outcome (PICO) as a search strategy tool on literature search quality: a systematic review. J Med Libr Assoc. 2018; 106:420–431.
Article21. Modesti PA, Reboldi G, Cappuccio FP, Agyemang C, Remuzzi G, Rapi S, et al. Panethnic differences in blood pressure in Europe: a systematic review and meta-analysis. PLoS One. 2016; 11:e0147601.
Article22. Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses [Internet]. Ottawa: Ottawa Hospital Research Institute;2000. cited 2019 Oct 8. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.23. Grosso G, Bella F, Godos J, Sciacca S, Del Rio D, Ray S, et al. Possible role of diet in cancer: systematic review and multiple meta-analyses of dietary patterns, lifestyle factors, and cancer risk. Nutr Rev. 2017; 75:405–419.
Article24. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327:557–560.
Article25. Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010; 1:97–111.
Article26. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997; 315:629–634.
Article27. Macaskill P, Walter SD, Irwig L. A comparison of methods to detect publication bias in meta-analysis. Stat Med. 2001; 20:641–654.
Article28. Baik I, Abbott RD, Curb JD, Shin C. Intake of fish and n-3 fatty acids and future risk of metabolic syndrome. J Am Diet Assoc. 2010; 110:1018–1026.
Article29. Cha D, Park Y. Association between dietary cholesterol and their food sources and risk for hypercholesterolemia: the 2012–2016 Korea national health and nutrition examination survey. Nutrients. 2019; 11:E846.
Article30. Chae MJ, Jang JY, Park K. Association between dietary calcium intake and the risk of cardiovascular disease among Korean adults. Eur J Clin Nutr. Forthcoming. 2019.
Article31. Cho YA, Kim J, Cho ER, Shin A. Dietary patterns and the prevalence of metabolic syndrome in Korean women. Nutr Metab Cardiovasc Dis. 2011; 21:893–900.
Article32. Choi JH, Woo HD, Lee JH, Kim J. Dietary patterns and risk for metabolic syndrome in Korean women. Medicine (Baltimore). 2015; 94:e1424.
Article33. Choi MK, Bae YJ. Association of magnesium intake with high blood pressure in Korean adults: Korea national health and nutrition examination survey 2007–2009. PLoS One. 2015; 10:e0130405.
Article34. Chung S, Chung MY, Choi HK, Park JH, Hwang JT. Consumption of black food decreases the risk of abdominal obesity in Korean women. Asia Pac J Clin Nutr. 2019; 28:266–275.35. Ha K, Joung H, Song Y. Low-carbohydrate diet and the risk of metabolic syndrome in Korean adults. Nutr Metab Cardiovasc Dis. 2018; 28:1122–1132.
Article36. Ha K, Kim K, Chun OK, Joung H, Song Y. Differential association of dietary carbohydrate intake with metabolic syndrome in the US and Korean adults: data from the 2007–2012 NHANES and KNHANES. Eur J Clin Nutr. 2018; 72:848–860.
Article37. Hong S, Song Y, Lee KH, Lee HS, Lee M, Jee SH, et al. A fruit and dairy dietary pattern is associated with a reduced risk of metabolic syndrome. Metabolism. 2012; 61:883–890.
Article38. Hong SA, Kim MK. Relationship between fruit and vegetable intake and the risk of metabolic syndrome and its disorders in Korean women according to menopausal status. Asia Pac J Clin Nutr. 2017; 26:514–523.39. Jang J, Shin MJ, Kim OY, Park K. Longitudinal association between egg consumption and the risk of cardiovascular disease: interaction with type 2 diabetes mellitus. Nutr Diabetes. 2018; 8:20.
Article40. Jeon J, Park K. Dietary vitamin B6 intake associated with a decreased risk of cardiovascular disease: a prospective cohort study. Nutrients. 2019; 11:E1484.
Article41. Joo NS, Yang SW, Park SJ, Choi SJ, Song BC, Yeum KJ. Milk consumption and Framingham Risk Score: Analysis of the Korea national health and nutrition examination survey data (2008–2011). Yonsei Med J. 2016; 57:197–202.
Article42. Kang Y, Kim J. Association between fried food consumption and hypertension in Korean adults. Br J Nutr. 2016; 115:87–94.
Article43. Kang Y, Kim J. Soft drink consumption is associated with increased incidence of the metabolic syndrome only in women. Br J Nutr. 2017; 117:315–324.
Article44. Kim D, Kim J. Dairy consumption is associated with a lower incidence of the metabolic syndrome in middle-aged and older Korean adults: the Korean Genome and Epidemiology Study (KoGES). Br J Nutr. 2017; 117:148–160.
Article45. Kim J. Dairy food consumption is inversely associated with the risk of the metabolic syndrome in Korean adults. J Hum Nutr Diet. 2013; 26 Suppl 1:171–179.
Article46. Kim J, Jo I. Grains, vegetables, and fish dietary pattern is inversely associated with the risk of metabolic syndrome in South Korean adults. J Am Diet Assoc. 2011; 111:1141–1149.
Article47. Kim J, Kim J. Association between fruit and vegetable consumption and risk of hypertension in middle-aged and older Korean adults. J Acad Nutr Diet. 2018; 118:1438–1449.e5.
Article48. Kim K, Kim K, Park SM. Association between the prevalence of metabolic syndrome and the level of coffee consumption among Korean women. PLoS One. 2016; 11:e0167007.
Article49. Kim SA, Joung H, Shin S. Dietary pattern, dietary total antioxidant capacity, and dyslipidemia in Korean adults. Nutr J. 2019; 18:37.
Article50. Kim SA, Lee JK, Kang D, Shin S. Oily fish consumption and the risk of dyslipidemia in Korean adults: a prospective cohort study based on the Health Examinees Gem (HEXA-G) study. Nutrients. 2019; 11:E2506.
Article51. Kim Y, Je Y. Moderate coffee consumption is inversely associated with the metabolic syndrome in the Korean adult population. Br J Nutr. 2018; 120:1279–1287.
Article52. Kim Y, Je Y. A modified Mediterranean diet score is inversely associated with metabolic syndrome in Korean adults. Eur J Clin Nutr. 2018; 72:1682–1689.
Article53. Kwak JH, Jo G, Chung HK, Shin MJ. Association between sugar-sweetened beverage consumption and incident hypertension in Korean adults: a prospective study. Eur J Nutr. 2019; 58:1009–1017.
Article54. Kwon HT, Lee CM, Park JH, Ko JA, Seong EJ, Park MS, et al. Milk intake and its association with metabolic syndrome in Korean: analysis of the third Korea National Health and Nutrition Examination Survey (KNHANES III). J Korean Med Sci. 2010; 25:1473–1479.
Article55. Lee H, Lee J, Hwang SS, Kim S, Chin HJ, Han JS, et al. Potassium intake and the prevalence of metabolic syndrome: the Korean National Health and Nutrition Examination Survey 2008–2010. PLoS One. 2013; 8:e55106.
Article56. Lee HA, An H, Park H. Identification of dietary patterns related to metabolic diseases and their association with cardiovascular disease: from the Korean Genome and Epidemiology Study. Nutrients. 2019; 11:E2434.
Article57. Lee HA, Park H. Diet-related risk factors for incident hypertension during an 11-year follow-up: the Korean Genome Epidemiology Study. Nutrients. 2018; 10:E1077.
Article58. Lee J, Lee JE, Kim Y. Relationship between coffee consumption and stroke risk in Korean population: the Health Examinees (HEXA) Study. Nutr J. 2017; 16:7.
Article59. Lee JE, Kim JH, Son SJ, Ahn Y, Lee J, Park C, et al. Dietary pattern classifications with nutrient intake and health-risk factors in Korean men. Nutrition. 2011; 27:26–33.
Article60. Lee KW, Cho MS. The traditional Korean dietary pattern is associated with decreased risk of metabolic syndrome: findings from the Korean National Health and Nutrition Examination Survey, 1998–2009. J Med Food. 2014; 17:43–56.
Article61. Lee KW, Cho W. The consumption of dairy products is associated with reduced risks of obesity and metabolic syndrome in Korean women but not in men. Nutrients. 2017; 9:E630.
Article62. Lee SM, Choi NK, Yoon BW, Park JM, Han MK, Park BJ. The impact of green tea consumption on the prevention of hemorrhagic stroke. Neuroepidemiology. 2015; 44:215–220.
Article63. Lee YJ, Song S, Song Y. High-carbohydrate diets and food patterns and their associations with metabolic disease in the Korean population. Yonsei Med J. 2018; 59:834–842.
Article64. Na W, Chung B, Sohn C. A relationship between dietary patterns and dyslipidemia in urban-dwelling middle-aged Korean men: using Korean Genome and Epidemiology Study (KoGES). Clin Nutr Res. 2019; 8:219–228.
Article65. Nam CM, Oh KW, Lee KH, Jee SH, Cho SY, Shim WH, et al. Vitamin C intake and risk of ischemic heart disease in a population with a high prevalence of smoking. J Am Coll Nutr. 2003; 22:372–378.
Article66. Noh HM, Park YS, Kim JH. Coffee consumption and coronary heart disease risk using the Framingham risk score. Asia Pac J Clin Nutr. 2017; 26:931–938.67. Oh C, No JK. Appropriate protein intake is one strategy in the management of metabolic syndrome in Korean elderly to mitigate changes in body composition. Nutr Res. 2018; 51:21–28.
Article68. Oh JS, Kim H, Vijayakumar A, Kwon O, Kim Y, Chang N. Association of dietary flavonoid intake with prevalence of type 2 diabetes mellitus and cardiovascular disease risk factors in Korean women aged ≥30 years. J Nutr Sci Vitaminol (Tokyo). 2017; 63:51–58.
Article69. Park K, Son J, Jang J, Kang R, Chung HK, Lee KW, et al. Unprocessed meat consumption and incident cardiovascular diseases in Korean adults: the Korean Genome and Epidemiology Study (KoGES). Nutrients. 2017; 9:E498.
Article70. Park S, Ahn J, Lee BK. Very-low-fat diets may be associated with increased risk of metabolic syndrome in the adult population. Clin Nutr. 2016; 35:1159–1167.
Article71. Park S, Ham JO, Lee BK. Effects of total vitamin A, vitamin C, and fruit intake on risk for metabolic syndrome in Korean women and men. Nutrition. 2015; 31:111–118.
Article72. Park SH, Lee KS, Park HY. Dietary carbohydrate intake is associated with cardiovascular disease risk in Korean: analysis of the third Korea National Health and Nutrition Examination Survey (KNHANES III). Int J Cardiol. 2010; 139:234–240.
Article73. Seo EH, Kim H, Kwon O. Association between total sugar intake and metabolic syndrome in middle-aged Korean men and women. Nutrients. 2019; 11:E2042.
Article74. Shin H, Yoon YS, Lee Y, Kim CI, Oh SW. Dairy product intake is inversely associated with metabolic syndrome in Korean adults: Anseong and Ansan cohort of the Korean Genome and Epidemiology Study. J Korean Med Sci. 2013; 28:1482–1488.
Article75. Shin HJ, Cho E, Lee HJ, Fung TT, Rimm E, Rosner B, et al. Instant noodle intake and dietary patterns are associated with distinct cardiometabolic risk factors in Korea. J Nutr. 2014; 144:1247–1255.
Article76. Shin J, Ham D, Shin S, Choi SK, Paik HY, Joung H. Effects of lifestyle-related factors on ischemic heart disease according to body mass index and fasting blood glucose levels in Korean adults. PLoS One. 2019; 14:e0216534.
Article77. Shin S, Kim SA, Ha J, Lim K. Sugar-sweetened beverage consumption in relation to obesity and metabolic syndrome among Korean adults: a cross-sectional study from the 2012–2016 Korean national health and nutrition examination survey (KNHANES). Nutrients. 2018; 10:E1467.
Article78. Shin S, Lee HW, Kim CE, Lim J, Lee JK, Kang D. Association between milk consumption and metabolic syndrome among Korean adults: results from the health examinees study. Nutrients. 2017; 9:E1102.
Article79. Shin S, Lee HW, Kim CE, Lim J, Lee JK, Lee SA, et al. Egg consumption and risk of metabolic syndrome in Korean adults: results from the health examinees study. Nutrients. 2017; 9:E687.
Article80. Shin S, Lim J, Lee HW, Kim CE, Kim SA, Lee JK, et al. Association between the prevalence of metabolic syndrome and coffee consumption among Korean adults: results from the Health Examinees study. Appl Physiol Nutr Metab. 2019; 44:1371–1378.
Article81. Shin WY, Kim JH. Low riboflavin intake is associated with cardiometabolic risks in Korean women. Asia Pac J Clin Nutr. 2019; 28:285–299.82. Shin Y, Lee S, Kim Y. Sweet preference associated with the risk of hypercholesterolemia among middle-aged women in Korea. J Atheroscler Thromb. 2018; 25:1215–1221.
Article83. Son J, Lee Y, Park K. Effects of processed red meat consumption on the risk of type 2 diabetes and cardiovascular diseases among Korean adults: the Korean Genome and Epidemiology Study. Eur J Nutr. 2019; 58:2477–2484.
Article84. Song HJ, Paek YJ, Choi MK, Yoo KB, Kang JH, Lee HJ. Gender Differences in the relationship between carbonated sugar-sweetened beverage intake and the likelihood of hypertension according to obesity. Int J Public Health. 2017; 62:573–581.
Article85. Song HJ, Park SJ, Jang DJ, Kwon DY, Lee HJ. High consumption of salt-fermented vegetables and hypertension risk in adults: a 12-year follow-up study. Asia Pac J Clin Nutr. 2017; 26:698–707.86. Song S, Kim J, Kim J. Gender differences in the association between dietary pattern and the incidence of hypertension in middle-aged and older adults. Nutrients. 2018; 10:E252.
Article87. Song S, Song WO, Song Y. Dietary carbohydrate and fat intakes are differentially associated with lipid abnormalities in Korean adults. J Clin Lipidol. 2017; 11:338–347.e3.
Article88. Suh I, Oh KW, Lee KH, Psaty BM, Nam CM, Kim SI, et al. Moderate dietary fat consumption as a risk factor for ischemic heart disease in a population with a low fat intake: a case-control study in Korean men. Am J Clin Nutr. 2001; 73:722–727.
Article89. Yang KY, Yong CS, Choi HD, Kim JO. Diet and lipid-lowering drug use among people with dyslipidemia in Korea. Asia Pac J Clin Nutr. 2019; 28:476–485.90. Aune D, Giovannucci E, Boffetta P, Fadnes LT, Keum N, Norat T, et al. Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality-a systematic review and dose-response meta-analysis of prospective studies. Int J Epidemiol. 2017; 46:1029–1056.
Article91. Wu L, Sun D, He Y. Fruit and vegetables consumption and incident hypertension: dose-response meta-analysis of prospective cohort studies. J Hum Hypertens. 2016; 30:573–580.
Article92. Kodama S, Horikawa C, Fujihara K, Ishii D, Hatta M, Takeda Y, et al. Relationship between intake of fruit separately from vegetables and triglycerides - A meta-analysis. Clin Nutr ESPEN. 2018; 27:53–58.
Article93. Li B, Li F, Wang L, Zhang D. Fruit and vegetables consumption and risk of hypertension: a meta-analysis. J Clin Hypertens (Greenwich). 2016; 18:468–476.
Article94. Michaëlsson K, Wolk A, Langenskiöld S, Basu S, Warensjö Lemming E, Melhus H, et al. Milk intake and risk of mortality and fractures in women and men: cohort studies. BMJ. 2014; 349:g6015.
Article95. Drouin-Chartier JP, Côté JA, Labonté ME, Brassard D, Tessier-Grenier M, Desroches S, et al. Comprehensive review of the impact of dairy foods and dairy fat on cardiometabolic risk. Adv Nutr. 2016; 7:1041–1051.
Article96. Ding M, Bhupathiraju SN, Satija A, van Dam RM, Hu FB. Long-term coffee consumption and risk of cardiovascular disease: a systematic review and a dose-response meta-analysis of prospective cohort studies. Circulation. 2014; 129:643–659.
Article97. de Koning Gans JM, Uiterwaal CS, van der Schouw YT, Boer JM, Grobbee DE, Verschuren WM, et al. Tea and coffee consumption and cardiovascular morbidity and mortality. Arterioscler Thromb Vasc Biol. 2010; 30:1665–1671.
Article98. Higashi Y. Coffee and endothelial function: a coffee paradox? Nutrients. 2019; 11:E2104.
Article99. Xi B, Huang Y, Reilly KH, Li S, Zheng R, Barrio-Lopez MT, et al. Sugar-sweetened beverages and risk of hypertension and CVD: a dose-response meta-analysis. Br J Nutr. 2015; 113:709–717.
Article100. Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol. 2014; 43:69–77.
Article101. Kim Y, Han BG; KoGES group. Cohort profile: the Korean Genome and Epidemiology Study (KoGES) Consortium. Int J Epidemiol. 2017; 46:e20.
Article102. Lim H, Kim J, Kim DY. Nutritional therapy for Asian patients at risk for atherosclerotic cardiovascular disease. J Lipid Atheroscler. 2019; 8:192–203.
Article103. Koo BK, Oh S, Kim YJ, Moon MK. Prediction of coronary heart disease risk in Korean patients with diabetes mellitus. J Lipid Atheroscler. 2018; 7:110–121.
Article104. Choi S. The potential role of biomarkers associated with ASCVD risk: risk-enhancing biomarkers. J Lipid Atheroscler. 2019; 8:173–182.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum: Associations of Dietary Intake with Cardiovascular Disease, Blood Pressure, and Lipid Profile in the Korean Population: a Systematic Review and Meta-Analysis
- Dietary intake and cancer incidence in Korean adults: a systematic review and meta-analysis of observational studies
- High Sodium Intake: Review of Recent Issues on Its Association with Cardiovascular Events and Measurement Methods
- Dietary Cholesterol Intake and Serum Cholesterol Concentration: Can We Eat Eggs without Limitation?
- Dietary Salt Intake and Hypertension