J Surg Ultrasound.
2019 Nov;6(2):38-45. 10.0000/jsu.2019.6.2.38.
Clinical Predictors of Upstaging to Invasive Cancer Postoperatively in Patients Diagnosed with Ductal Carcinoma In Situ before Surgery
- Affiliations
-
- 1Department of Surgery, Eunpyeong St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea.
- 2Department of Surgery, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea. chanheun1@gmail.com
- KMID: 2469747
- DOI: http://doi.org/10.0000/jsu.2019.6.2.38
Abstract
- PURPOSE
Upstaging to invasive cancer (IC) is often found after surgery in those patients diagnosed with ductal carcinoma in situ (DCIS) and who underwent preoperative needle biopsy. This may change the post-surgical plans that include the re-operation, chemotherapy, and/or radiotherapy. Yet, there are no clinically available factors to predict IC in preoperatively diagnosed DCIS patients. This study evaluated the clinical and pathological predictive risk factors for upgrading DCIS to IC.
METHODS
This study retrospectively evaluated those patients who were diagnosed with DCIS preoperatively, and this diagnosis was followed by performing breast surgery between Jan 2005 and June 2018. Clinico-pathological factors were collected for the analysis between the pure DCIS group and the IC group.
RESULTS
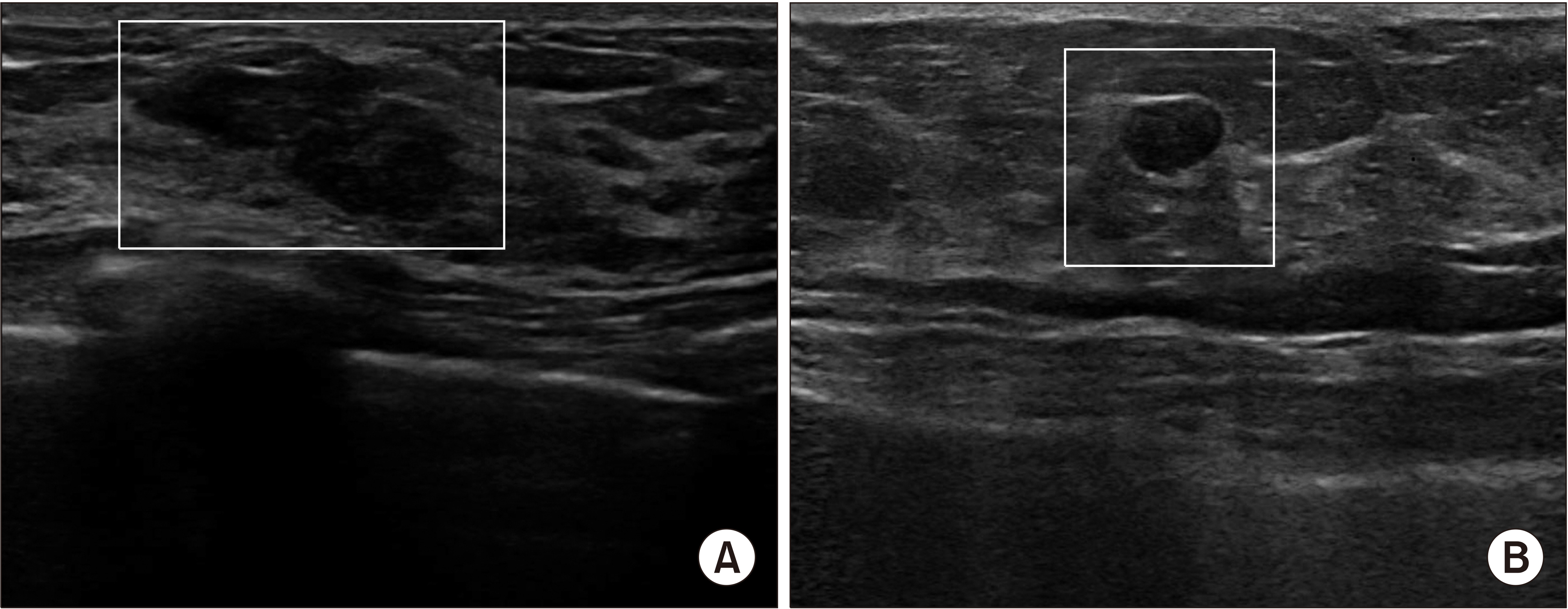
Of the 431 patients included in the study, 34 (7.9%) were upstaged to IC after surgery, and 397 (92.1%) were diagnosed as having pure DCIS. The nuclear grade was the sole predictor of upstaging to IC on the analysis of the clinico-pathological factors (odds ratio [OR] = 2.39, 95% confidence interval [95% CI] = 1.05-5.42, P = 0.038 on the univariate analysis; aOR = 2.86, 95% CI = 1.14-7.14, P = 0.025 on the multivariate analysis). The mass's size and characteristics, as determined by sonography, were not predictive of IC.
CONCLUSION
The sonographic findings were not significant factors for predicting IC in preoperative DCIS patients. A high nuclear grade was the only statistically significant factor associated with IC. Considering the variability of the gauge of biopsy needles or the method for needle biopsy, large-scale prospective studies that control these variables may well reveal available predictive factors of IC in patients with DCIS.
Keyword
MeSH Terms
Figure
Reference
-
World Cancer Research Fund, American Institute for Cancer Research. 2019. Breast cancer statistics: breast cancer is the most common cancer in women worldwide [Internet]. World Cancer Research Fund;London: Available at: https://www.wcrf.org/dietandcancer/cancer-trends/breast-cancer-statistics . cited 2019 Oct 30.Youn HJ., Ahn HR., Kang SY., Jung SH. 2019. Efficacy of ultrasonography in breast cancer screening. J Surg Ultrasound. 6:1–7. DOI: 10.46268/jsu.2019.6.1.1.
ArticleDillon MF., McDermott EW., Quinn CM., O'Doherty A., O'Higgins N., Hill AD. 2006. Predictors of invasive disease in breast cancer when core biopsy demonstrates DCIS only. J Surg Oncol. 93:559–63. DOI: 10.1002/jso.20445. PMID: 16705731.
ArticleMaffuz A., Barroso-Bravo S., Nájera I., Zarco G., Alvarado-Cabrero I., Rodríguez-Cuevas SA. 2006. Tumor size as predictor of microinvasion, invasion, and axillary metastasis in ductal carcinoma in situ. J Exp Clin Cancer Res. 25:223–7. PMID: 16918134.Meijnen P., Oldenburg HS., Loo CE., Nieweg OE., Peterse JL., Rutgers EJ. 2007. Risk of invasion and axillary lymph node metastasis in ductal carcinoma in situ diagnosed by core-needle biopsy. Br J Surg. 94:952–6. DOI: 10.1002/bjs.5735. PMID: 17440955.Guillot E., Vaysse C., Goetgeluck J., Falcou MC., Couturaud B., Fitoussi A, et al. 2014. Extensive pure ductal carcinoma in situ of the breast: identification of predictors of associated infiltrating carcinoma and lymph node metastasis before immediate reconstructive surgery. Breast. 23:97–103. DOI: 10.1016/j.breast.2013.12.002. PMID: 24388733.
ArticleGoto M., Yuen S., Akazawa K., Nishida K., Konishi E., Kajihara M, et al. 2012. The role of breast MR imaging in pre-operative determination of invasive disease for ductal carcinoma in situ diagnosed by needle biopsy. Eur Radiol. 22:1255–64. DOI: 10.1007/s00330-011-2357-2. PMID: 22205445.
ArticleMori N., Ota H., Mugikura S., Takasawa C., Tominaga J., Ishida T, et al. 2013. Detection of invasive components in cases of breast ductal carcinoma in situ on biopsy by using apparent diffusion coefficient MR parameters. Eur Radiol. 23:2705–12. DOI: 10.1007/s00330-013-2902-2. PMID: 23732688.
ArticleWisner DJ., Hwang ES., Chang CB., Tso HH., Joe BN., Lessing JN, et al. 2013. Features of occult invasion in biopsy-proven DCIS at breast MRI. Breast J. 19:650–8. DOI: 10.1111/tbj.12201. PMID: 24165314. PMCID: PMC4036640.
ArticlePark AY., Gweon HM., Son EJ., Yoo M., Kim JA., Youk JH. 2014. Ductal carcinoma in situ diagnosed at US-guided 14-gauge core-needle biopsy for breast mass: preoperative predictors of invasive breast cancer. Eur J Radiol. 83:654–9. DOI: 10.1016/j.ejrad.2014.01.010. PMID: 24534119.
ArticleNori J., Meattini I., Giannotti E., Abdulcadir D., Mariscotti G., Calabrese M, et al. 2014. Role of preoperative breast MRI in ductal carcinoma in situ for prediction of the presence and assessment of the extent of occult invasive component. Breast J. 20:243–8. DOI: 10.1111/tbj.12250. PMID: 24750509.
ArticleLee CW., Wu HK., Lai HW., Wu WP., Chen ST., Chen DR, et al. 2016. Preoperative clinicopathologic factors and breast magnetic resonance imaging features can predict ductal carcinoma in situ with invasive components. Eur J Radiol. 85:780–9. DOI: 10.1016/j.ejrad.2015.12.027. PMID: 26971424.
ArticleR Core Team. 2016. R: a language and environment for statistical computing [Internet]. R Foundation for Statistical Computing;Vienna: Available at: https://www.R-project.org/ . cited 2019 Feb 20.Therneau TM. 2015. A package for survival analysis in S. version 2.38. [Internet]. R Foundation for Statistical Computing;Vienna: Available at: https://CRAN.R-project.org/package=survival . cited 2019 Feb 20.Yen TW., Hunt KK., Ross MI., Mirza NQ., Babiera GV., Meric-Bernstam F, et al. 2005. Predictors of invasive breast cancer in patients with an initial diagnosis of ductal carcinoma in situ: a guide to selective use of sentinel lymph nodebiopsy in management of ductal carcinoma in situ. J Am Coll Surg. 200:516–26. DOI: 10.1016/j.jamcollsurg.2004.11.012. PMID: 15804465.Rutstein LA., Johnson RR., Poller WR., Dabbs D., Groblewski J., Rakitt T, et al. 2007. Predictors of residual invasive disease after core needle biopsy diagnosis of ductal carcinoma in situ. Breast J. 13:251–7. DOI: 10.1111/j.1524-4741.2007.00418.x. PMID: 17461899.
ArticleGo EM., Chan SK., Vong JS., Lui PC., Chan AW., Ma TK, et al. 2010. Predictors of invasion in needle core biopsies of the breast with ductal carcinoma in situ. Mod Pathol. 23:737–42. DOI: 10.1038/modpathol.2009.187. PMID: 20081814.
ArticleChan MY., Lim S. 2010. Predictors of invasive breast cancer in ductal carcinoma in situ initially diagnosed by core biopsy. Asian J Surg. 33:76–82. DOI: 10.1016/S1015-9584(10)60013-9. PMID: 21029943.
ArticleHuang YT., Cheung YC., Lo YF., Ueng SH., Kuo WL., Chen SC. 2011. MRI findings of cancers preoperatively diagnosed as pure DCIS at core needle biopsy. Acta Radiol. 52:1064–8. DOI: 10.1258/ar.2011.110213. PMID: 21969708.
ArticleHan JS., Molberg KH., Sarode V. 2011. Predictors of invasion and axillary lymph node metastasis in patients with a core biopsy diagnosis of ductal carcinoma in situ: an analysis of 255 cases. Breast J. 17:223–9. DOI: 10.1111/j.1524-4741.2011.01069.x. PMID: 21545433.
ArticleBrennan ME., Turner RM., Ciatto S., Marinovich ML., French JR., Macaskill P, et al. 2011. Ductal carcinoma in situ at core-needle biopsy: meta-analysis of underestimation and predictors of invasive breast cancer. Radiology. 260:119–28. DOI: 10.1148/radiol.11102368. PMID: 21493791.
ArticleKim J., Han W., Lee JW., You JM., Shin HC., Ahn SK, et al. 2012. Factors associated with upstaging from ductal carcinoma in situ following core needle biopsy to invasive cancer in subsequent surgical excision. Breast. 21:641–5. DOI: 10.1016/j.breast.2012.06.012. PMID: 22749854.
ArticleHollingsworth AB., Stough RG. 2012. Multicentric and contralateral invasive tumors identified with pre-op MRI in patients newly diagnosed with ductal carcinoma in situ of the breast. Breast J. 18:420–7. DOI: 10.1111/j.1524-4741.2012.01273.x. PMID: 22804792.
ArticleTrentin C., Dominelli V., Maisonneuve P., Menna S., Bazolli B., Luini A, et al. 2012. Predictors of invasive breast cancer and lymph node involvement in ductal carcinoma in situ initially diagnosed by vacuum-assisted breast biopsy: experience of 733 cases. Breast. 21:635–40. DOI: 10.1016/j.breast.2012.06.009. PMID: 22795363.
ArticleNadrljanski M., Maksimović R., Plešnac-Karapandžć V., Nikitović M., Marković-Vasiljković B., Milošvić Z. 2014. Positive enhancement integral values in dynamic contrast enhanced magnetic resonance imaging of breast carcinoma: ductal carcinoma in situ vs. invasive ductal carcinoma. Eur J Radiol. 83:1363–7. DOI: 10.1016/j.ejrad.2014.05.006. PMID: 24894697.
ArticleDeurloo EE., Sriram JD., Teertstra HJ., Loo CE., Wesseling J., Rutgers EJ, et al. 2012. MRI of the breast in patients with DCIS to exclude the presence of invasive disease. Eur Radiol. 22:1504–11. DOI: 10.1007/s00330-012-2394-5. PMID: 22367470.
ArticleWilkie C., White L., Dupont E., Cantor A., Cox CE. 2005. An update of sentinel lymph node mapping in patients with ductal carcinoma in situ. Am J Surg. 190:563–6. DOI: 10.1016/j.amjsurg.2005.06.011. PMID: 16164920.
ArticleGoyal A., Douglas-Jones A., Monypenny I., Sweetland H., Stevens G., Mansel RE. 2006. Is there a role of sentinel lymph node biopsy in ductal carcinoma in situ?: analysis of 587 cases. Breast Cancer Res Treat. 98:311–4. DOI: 10.1007/s10549-006-9167-2. PMID: 16552627.
ArticleLee JM., Kaplan JB., Murray MP., Mazur-Grbec M., Tadic T., Stimac D, et al. 2007. Underestimation of DCIS at MRI-guided vacuum-assisted breast biopsy. AJR Am J Roentgenol. 189:468–74. DOI: 10.2214/AJR.07.2172. PMID: 17646475.
ArticleSantamaría G., Velasco M., Farrús B., Zanón G., Fernández PL. 2008. Preoperative MRI of pure intraductal breast carcinoma--a valuable adjunct to mammography in assessing cancer extent. Breast. 17:186–94. DOI: 10.1016/j.breast.2007.09.005. PMID: 17964786.
ArticleLee JW., Han W., Ko E., Cho J., Kim EK., Jung SY, et al. 2008. Sonographic lesion size of ductal carcinoma in situ as a preoperative predictor for the presence of an invasive focus. J Surg Oncol. 98:15–20. DOI: 10.1002/jso.21077. PMID: 18459155.
ArticleKim S., Kim J., Park HS., Kim HY., Lee K., Lee J, et al. 2019. An updated nomogram for predicting invasiveness in preoperative ductal carcinoma in situ of the breast. Yonsei Med J. 60:1028–35. DOI: 10.3349/ymj.2019.60.11.1028. PMID: 31637884. PMCID: PMC6813145.
ArticleSi J., Yang B., Guo R., Huang N., Quan C., Ma L, et al. 2019. Factors associated with upstaging in patients preoperatively diagnosed with ductal carcinoma in situ by core needle biopsy. Cancer Biol Med. 16:312–8. DOI: 10.20892/j.issn.2095-3941.2018.0159. PMID: 31516751. PMCID: PMC6713631.Kim YS., Park WS., Min SY. 2017. Diagnostic usefulness of shear-wave elastography for an evaluation of BI-RADS category 4a breast lesions detected by US. J Surg Ultrasound. 4:48–54.Youn HJ., Kang SY., Jung SH. 2018. Clinical application of shear wave elastography in patients with breast cancer. J Surg Ultrasound. 5:33–8. DOI: 10.46268/jsu.2018.5.2.33.
ArticleVinnicombe SJ., Whelehan P., Thomson K., McLean D., Purdie CA., Jordan LB, et al. 2014. What are the characteristics of breast cancers misclassified as benign by quantitative ultrasound shear wave elastography? Eur Radiol. 24:921–6. DOI: 10.1007/s00330-013-3079-4. PMID: 24326756.
ArticleEvans A., Purdie CA., Jordan L., Macaskill EJ., Flynn J., Vinnicombe S, et al. 2016. Stiffness at shear-wave elastography and patient presentation predicts upgrade at surgery following an ultrasound-guided core biopsy diagnosis of ductal carcinoma in situ. Clin Radiol. 71:1156–9. DOI: 10.1016/j.crad.2016.07.004. PMID: 27499466.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Predictors for the Transition from Ductal Carcinoma In Situ to Invasive Breast Cancer in Korean Patients
- Predictive Factors of Residual Invasive Breast Cancer after Core Biopsy for Ductal Carcinoma in Situ
- Invasive Lobular Carcinoma of the Breast Associated with Mixed Lobular and Ductal Carcinoma In Situ: A Case Report
- An Unusual Presentation of Extensive Ductal Carcinoma in Situ Accompanying Invasive Ductal Carcinoma on MRI: A Case Report
- Risk Factor of Invasive Breast Cancer in Patients with Preoperative Diagnosis of Ductal Carcinoma in Situ