J Korean Fract Soc.
2019 Oct;32(4):204-210. 10.12671/jkfs.2019.32.4.204.
Use of Miniplate for Severe Comminuted Metadiaphyseal Fractures of the Distal Radius
- Affiliations
-
- 1Department of Orthopaedic Surgery, Gachon University College of Medicine, Incheon, Korea.
- 2Orthopedic Trauma Division, Trauma Center, Gachon University College of Medicine, Incheon, Korea. dryoonyc@gmail.com
- KMID: 2468683
- DOI: http://doi.org/10.12671/jkfs.2019.32.4.204
Abstract
- PURPOSE
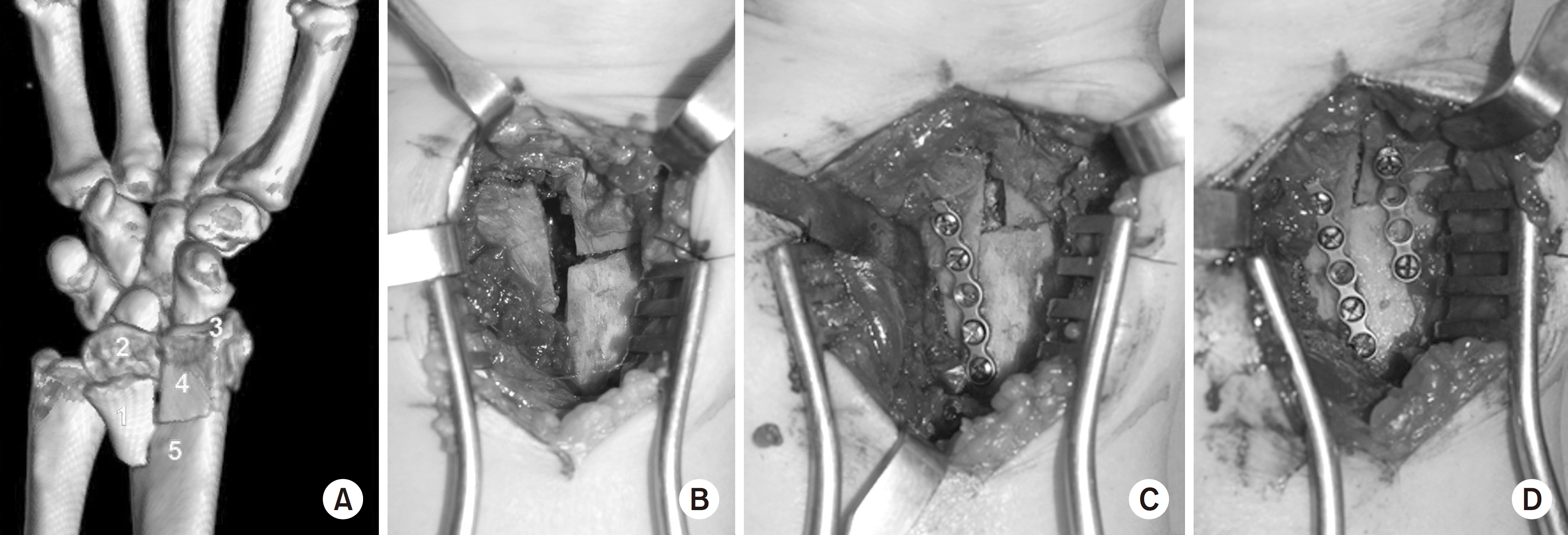
This study investigated the clinical and radiological outcomes of patients undergoing provisional fixation in conjunction with locking plate fixation. Miniplates were used as the reduction plates for the surgical treatment of severe comminuted metadiaphyseal fractures with an intra-articular fracture of the distal radius.
MATERIALS AND METHODS
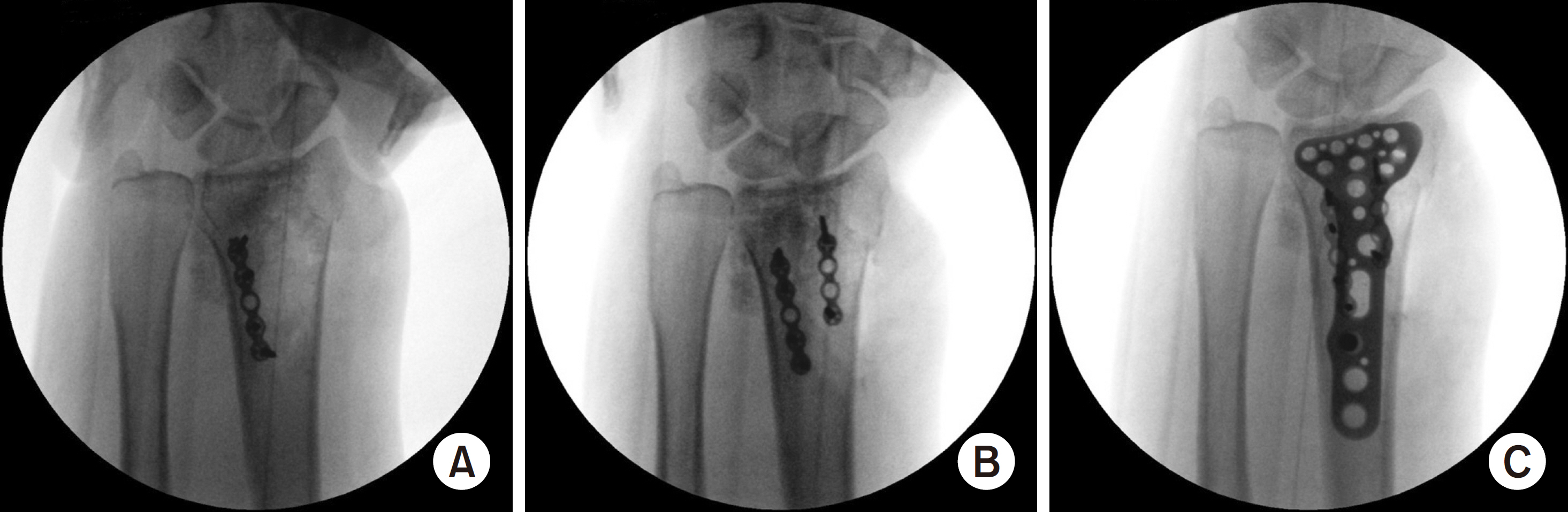
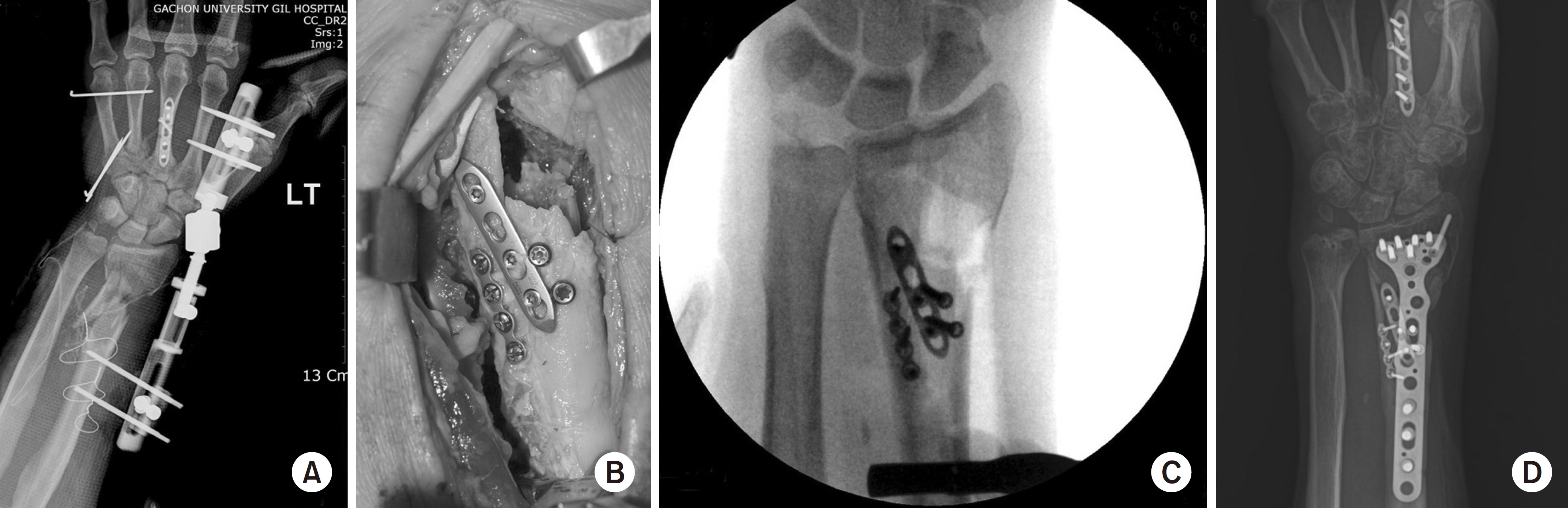
The radial length, radial inclination, volar tilt, and radial intra-articular step-off were measured preoperatively, postoperatively, and at one year after surgery in 12 patients (eight males, four females, mean age 55.4 years old). The patients underwent volar locking plate fixation with miniplate as a reduction plate for severe comminuted metadiaphyseal fractures with an intra-articular fracture of the distal radius. Clinical evaluations were conducted using the modified Mayo wrist score (MMWS).
RESULTS
Bone union was achieved in all cases. The mean MMWS was 81.8 points, including two excellent, three good, and seven fair cases. Radiological improvements were observed in the average radial length (preoperative, 6.4 mm; postoperative, 11.8 mm), average radial inclination (10.2° to 22.4°), average volar tilt (−4.5° to 10.6°), and average radial intra-articular step-off (4.8-0.8 mm) (all, p<0.05). Radiographic measurements obtained immediately after surgery and at the final follow-up revealed insignificant decreases in radial length (0.6 mm), radial inclination (0.4°), and volar tilt (0.9°) (all, p>0.05).
CONCLUSION
Miniplate fixation can be an effective treatment option as a reduction plate for the treatment of distal radial fractures, which is challenging to reduce and maintain due to severely comminuted metadiaphysis fractures with the intra-articular fracture.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Kapoor H, Agarwal A, Dhaon BK. Displaced intraarticular fractures of distal radius: a comparative evaluation of results following closed reduction, external fixation and open reduction with internal fixation. Injury. 31:75–79. 2000.
Article2. Harley BJ, Scharfenberger A, Beaupre LA, Jomha N, Weber DW. Augmented external fixation versus percutaneous pinning and casting for unstable fractures of the distal radius–a prospective randomized trial. J Hand Surg Am. 29:815–824. 2004.
Article3. Gruber G, Bernhardt GA, Köhler G, Gruber K. Surgical treatment of distal radius fractures with an angle fixed bar palmar plating system: a single center study of 102 patients over a 2-year period. Arch Orthop Trauma Surg. 126:680–685. 2006.
Article4. Figl M, Weninger P, Liska M, Hofbauer M, Leixnering M. Volar fixed-angle plate osteosynthesis of unstable distal radius fractures: 12 months results. Arch Orthop Trauma Surg. 129:661–669. 2009.5. Chung KC, Watt AJ, Kotsis SV, Margaliot Z, Haase SC, Kim HM. Treatment of unstable distal radial fractures with the volar locking plating system. J Bone Joint Surg Am. 88:2687–2694. 2006.
Article6. Downing ND, Karantana A. A revolution in the management of fractures of the distal radius? J Bone Joint Surg Br. 90:1271–1275. 2008.
Article7. Cho SH, Park HG, Jun DS, et al. Outcomes of severe comminuted distal radius fractures with pronator preserving approach. J Korean Fract Soc. 28:178–185. 2015.
Article8. Mast J, Jakob R, Ganz R. Planning and reduction technique in fracture surgery. Berlin, Heidelberg: Springer;p. 54–75. 1989.9. Benirschke SK, Henley MB, Ott JW. Proximal one-third tibial fracture solution. Orthop Trans. 18:1055–1056. 1995.10. Lang GJ, Cohen BE, Bosse MJ, Kellam JF. Proximal third tibial shaft fractures. Should they be nailed? Clin Orthop Relat Res. 315:64–74. 1995.
Article11. Archdeacon MT, Wyrick JD. Reduction plating for provisional fracture fixation. J Orthop Trauma. 20:206–211. 2006.
Article12. Yun HH, Lee YI, Kim KH, Yun SH. Use of auxiliary locking plates for the treatment of unstable pertrochanteric femur fractures. Orthopedics. 15:305–309. 2015.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Comminuted Distal Radius Fracutures with External Skeletal Fixation
- Operative Treatment of Unstable Fracture of Distal Radius
- Percutaneous pinning of intraarticular comminuted fracture of the distal radius
- Failure of Distal Locking Screws in an Intraarticular Distal Radius Fracture Treated with Volar Locking Plate Fixation
- Treatment of Comminuted - Intraarticular Fracture of Distal Radius using External Fixator: Comparative Study of Treatment by External Fixation with or Without bone Graft