Perinatology.
2018 Jun;29(2):72-77. 10.14734/PN.2018.29.2.72.
Trends in Treatment Outcome and Critical Predictors of Mortality for Congenital Diaphragmatic Hernia in a Single Center
- Affiliations
-
- 1Division of Neonatalogy, Department of Pediatrics, Asan Medical Center Children's Hospital, University of Ulsan College of Medicine, Seoul, Korea. arkim@amc.seoul.kr
- 2Department of Pediatrics, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea.
- 3Division of Pediatric Surgery, Department of Surgery, Asan Medical Center Children's Hospital, University of Ulsan College of Medicine, Seoul, Korea. kimdy@amc.seoul.kr
- 4Department of Obstetrics and Gynecology, Asan Medical Center Children's Hospital, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2468552
- DOI: http://doi.org/10.14734/PN.2018.29.2.72
Abstract
OBJECTIVE
To review trends in treatment outcomes, to determine risk factors for mortality, and to present a cut-off values of observed/expected lung to head ratio (O/E LHR) predicting mortality in infants with congenital diaphragmatic hernia (CDH).
METHODS
A retrospective study of infants with CDH treated in the neonatal intensive care unit at tertiary medical center over 27 years (1989 to 2016) was done. We analyzed the factors associated with mortality and based on significant factors in predicting the mortality, the best cut-off value of O/E LHR was sought.
RESULTS
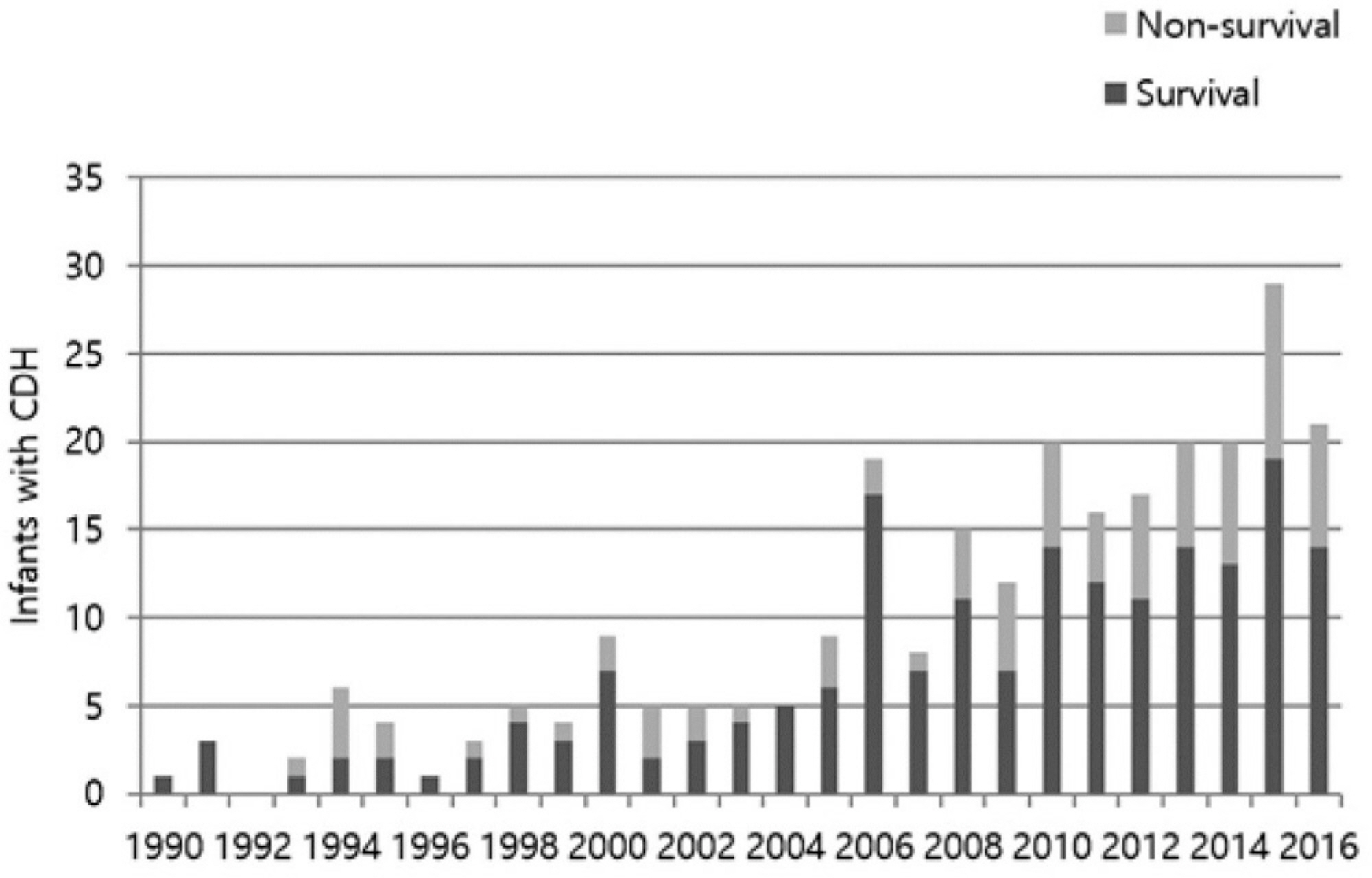
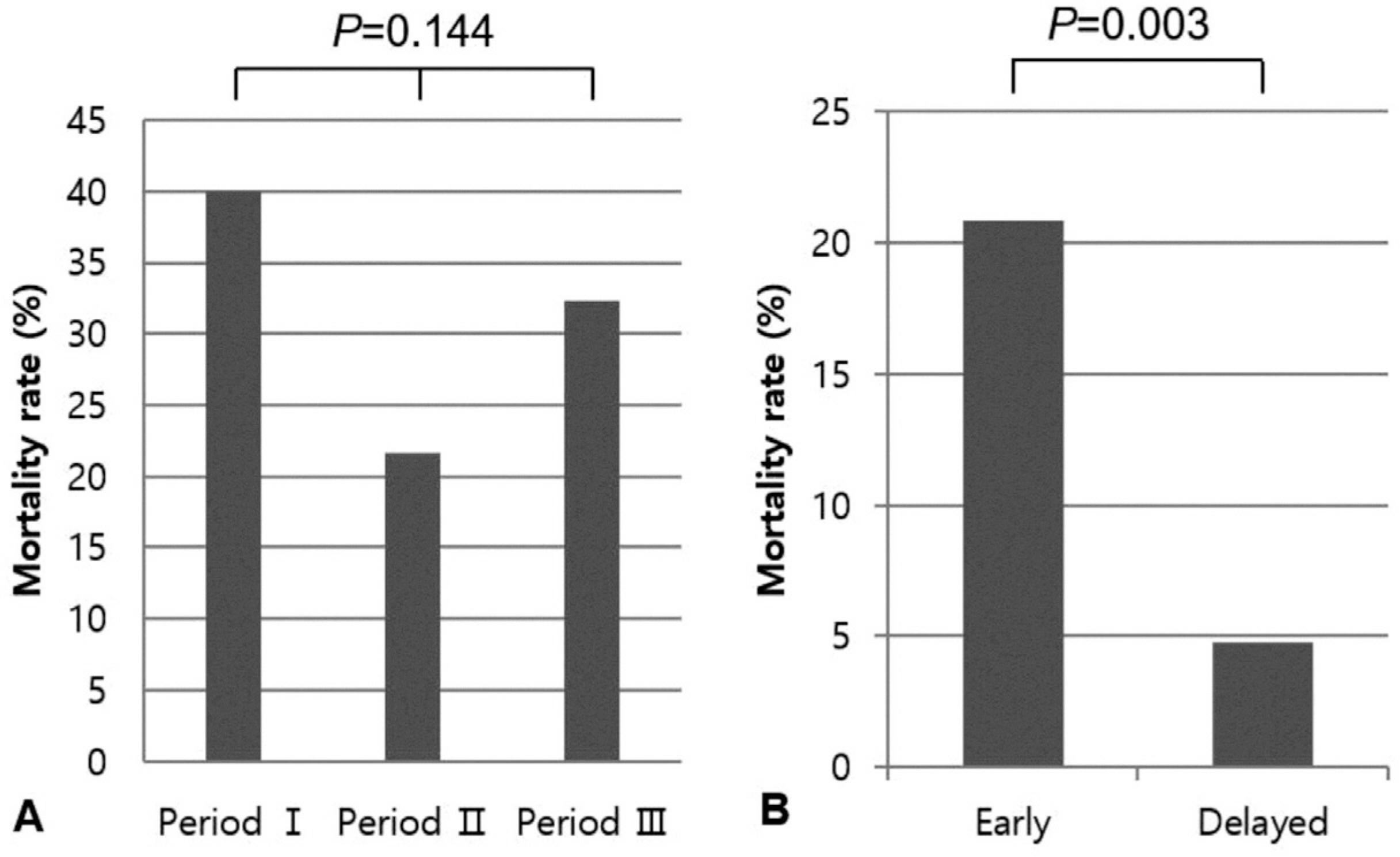
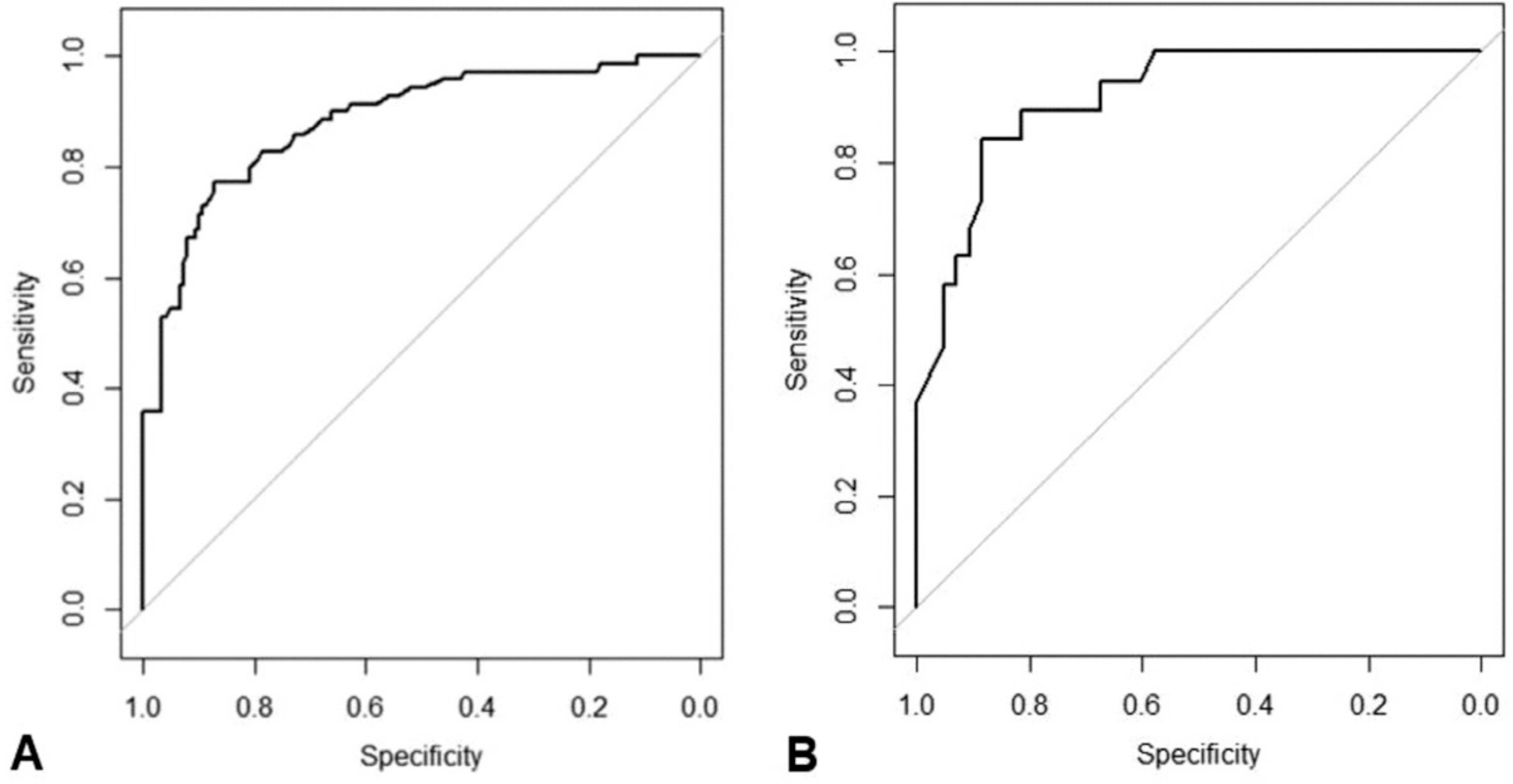
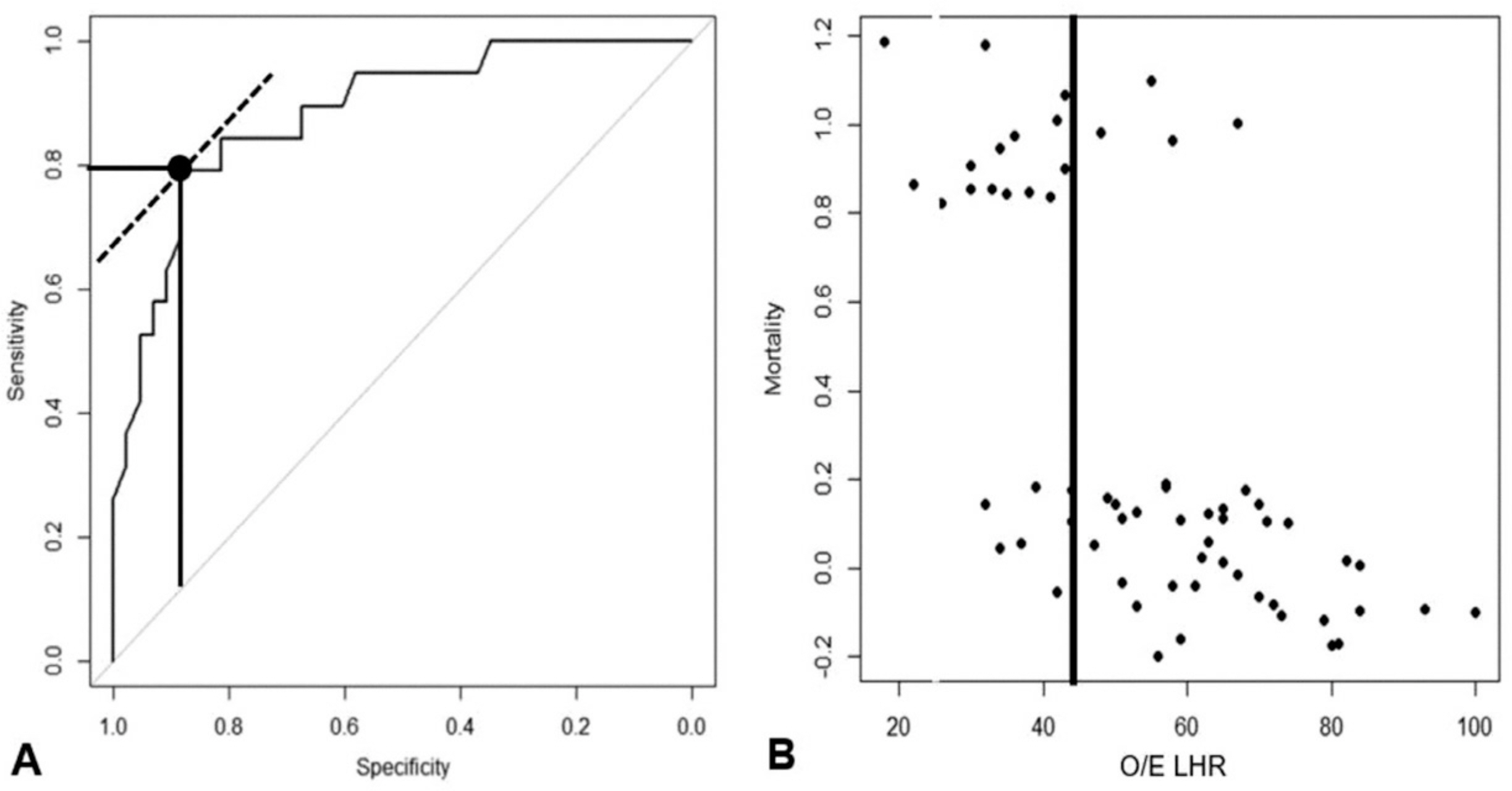
A total of 264 patients were included for the study. The mean gestational age and birth weight were 38.0±2.2 weeks and 2,934.2±578.2 g, respectively. Seventy nine patients (29.9%) died. The range of yearly mortality rate varied from 0 to 67%. Prenatal, neonatal, and surgical factors associated to mortality included time of prenatal diagnosis, polyhydramnios, O/E LHR, associated major congenital anomalies (cardiac, gastrointestinal or chromosomal anomalies), gestational age, birth weight, Apgar scores, initial pH and pCO2, and number of herniated organs. Among 62 fetuses whose O/E LHR were available, O/E LHR and major congenital anomalies were independent risk factors for mortality (area under curve=0.918), fetuses with O/E LHR < 44% without congenital anomalies showed predicted mortality of 72% and fetuses with O/E LHR ≥44% without congenital anomalies showed expected mortality of 7%.
CONCLUSION
The mortality of Infants with CDH has not improved despite advance of neonatal care. The O/E LHR and the presence of major congenital anomalies could be used adjunctively when counseling parents about the prognosis.
MeSH Terms
Figure
Reference
-
1). Langham MR Jr., Kays DW., Ledbetter DJ., Frentzen B., Sanford LL., Richards DS. Congenital diaphragmatic hernia. Epidemiology and outcome. Clin Perinatol. 1996. 23:671–88.2). Javid PJ., Jaksic T., Skarsgard ED., Lee S. Canadian Neonatal Network. Survival rate in congenital diaphragmatic hernia: the experience of the Canadian Neonatal Network. J Pediatr Surg. 2004. 39:657–60.
Article3). Colvin J., Bower C., Dickinson JE., Sokol J. Outcomes of congenital diaphragmatic hernia: a population-based study in Western Australia. Pediatrics. 2005. 116:e356–63.
Article4). Harting MT., Lally KP. The Congenital Diaphragmatic Hernia Study Group registry update. Semin Fetal Neonatal Med. 2014. 19:370–5.
Article5). Garriboli M., Duess JW., Ruttenstock E., Bishay M., Eaton S., De Coppi P, et al. Trends in the treatment and outcome of congenital diaphragmatic hernia over the last decade. Pediatr Surg Int. 2012. 28:1177–81.
Article6). Skari H., Bjornland K., Frenckner B., Friberg LG., Heikkinen M., Hurme T, et al. Congenital diaphragmatic hernia in Scandinavia from 1995 to 1998: predictors of mortality. J Pediatr Surg. 2002. 37:1269–75.
Article7). Stege G., Fenton A., Jaffray B. Nihilism in the 1990s: the true mortality of congenital diaphragmatic hernia. Pediatrics. 2003. 112(3 Pt 1):532–5.
Article8). Nobuhara KK., Wilson JM. Pathophysiology of congenital diaphragmatic hernia. Semin Pediatr Surg. 1996. 5:234–42.9). Congenital Diaphragmatic Hernia Study Group. Lally KP., Lally PA., Lasky RE., Tibboel D., Jaksic T, et al. Defect size determines survival in infants with congenital diaphragmatic hernia. Pediatrics. 2007. 120:e651–7.10). Thébaud B., Azancot A., de Lagausie P., Vuillard E., Ferkadji L., Benali K, et al. Congenital diaphragmatic hernia: antenatal prognostic factors. Does cardiac ventricular disproportion in utero predict outcome and pulmonary hypoplasia? Intensive Care Med. 1997. 23:10062–9.
Article11). Congenital Diaphragmatic Hernia Study Group. Estimating disease severity of congenital diaphragmatic hernia in the first 5 minutes of life. J Pediatr Surg. 2001. 36:141–5.12). Numanoglu A., Morrison C., Rode H. Prediction of outcome in congenital diaphragmatic hernia. Pediatr Surg Int. 1998. 13:564–8.
Article13). Deprest J., Jani J., Van Schoubroeck D., Cannie M., Gallot D., Dymarkowski S, et al. Current consequences of prenatal diagnosis of congenital diaphragmatic hernia. J Pediatr Surg. 2006. 41:423–30.
Article14). Fumino S., Shimotake T., Kume Y., Tsuda T., Aoi S., Kimura O, et al. A clinical analysis of prognostic parameters of survival in children with congenital diaphragmatic hernia. Eur J Pediatr Surg. 2005. 15:399–403.
Article15). Park HW., Lee BS., Lim G., Choi YS., Kim EA., Kim KS. A simplified formula using early blood gas analysis can predict survival outcomes and the requirements for extracorporeal membrane oxygenation in congenital diaphragmatic hernia. J Korean Med Sci. 2013. 28:924–8.
Article16). Jani J., Peralta CF., Van Schoubroeck D., Deprest J., Nicolaides KH. Relationship between lung-to-head ratio and lung volume in normal fetuses and fetuses with diaphragmatic hernia. Ultrasound Obstet Gynecol. 2006. 27:545–50.
Article17). Jani J., Peralta CF., Benachi A., Deprest J., Nicolaides KH. Assessment of lung area in fetuses with congenital diaphragmatic hernia. Ultrasound Obstet Gynecol. 2007. 30:72–6.
Article18). Logan JW., Rice HE., Goldberg RN., Cotten CM. Congenital diaphragmatic hernia: a systematic review and summary of best-evidence practice strategies. J Perinatol. 2007. 27:535–49.
Article19). Tracy ET., Mears SE., Smith PB., Danko ME., Diesen DL., Fisher KA, et al. Protocolized approach to the management of congenital diaphragmatic hernia: benefits of reducing variability in care. J Pediatr Surg. 2010. 45:1343–8.
Article20). Frenckner B., Ehren H., Granholm T., Linden V., Palmer K. Improved results in patients who have congenital diaphragmatic hernia using preoperative stabilization, extracorporeal membrane oxygenation, and delayed surgery. J Pediatr Surg. 1997. 32:1185–9.
Article21). Sakai H., Tamura M., Hosokawa Y., Bryan AC., Barker GA., Bohn DJ. Effect of surgical repair on respiratory mechanics in congenital diaphragmatic hernia. J Pediatr. 1987. 111:432–8.
Article22). Burgos CM., Frenckner B. Addressing the hidden mortality in CDH: a population-based study. J Pediatr Surg. 2017. 52:522–5.
Article23). Skari H., Bjornland K., Haugen G., Egeland T., Emblem R. Congenital diaphragmatic hernia: a meta-analysis of mortality factors. J Pediatr Surg. 2000. 35:1187–97.
Article24). Kim BE., Ha EJ., Kim YA., Kim S., Par JJ., Yun TJ, et al. Four cases of extracorporeal membrane oxygenation for congenital diaphragmatic hernia. J Korean Soc Neonatol. 2009. 16:64–70.25). Boloker J., Bateman DA., Wung JT., Stolar CJ. Congenital diaphragmatic hernia in 120 infants treated consecutively with permissive hyper-capnea/spontaneous respiration/elective repair. J Pediatr Surg. 2002. 37:357–66.
Article26). Nakayama DK., Motoyama EK., Tagge EM. Effect of preoperative stabilization on respiratory system compliance and outcome in newborn infants with congenital diaphragmatic hernia. J Pediatr. 1991. 118:793–9.
Article27). Moyer V., Moya F., Tibboel R., Losty P., Nagaya M., Lally KP. Late versus early surgical correction for congenital diaphragmatic hernia in newborn infants. Cochrane Database Syst Rev. 2002. 3:CD001695.
Article28). Seo JY., Nam SH., Kim DY., Kim SC., Kim AR., Kim KS, et al. Prognosis of bochdalek hernia in neonate after change in management principle. J Korean Assoc Pediatr Surg. 2006. 12:192–201.
Article29). Metkus AP., Filly RA., Stringer MD., Harrison MR., Adzick NS. Sonographic predictors of survival in fetal diaphragmatic hernia. J Pediatr Surg. 1996. 31:148–51. discussion 151-2.
Article30). Jani J., Nicolaides KH., Keller RL., Benachi A., Peralta CF., Favre R, et al. Observed to expected lung area to head circumference ratio in the prediction of survival in fetuses with isolated diaphragmatic hernia. Ultrasound Obstet Gynecol. 2007. 30:67–71.
Article31). Deprest JA., Flemmer AW., Gratacos E., Nicolaides K. Antenatal prediction of lung volume and in-utero treatment by fetal endoscopic tracheal occlusion in severe isolated congenital diaphragmatic hernia. Semin Fetal Neonatal Med. 2009. 14:8–13.
Article32). Zaiss I., Kehl S., Link K., Neff W., Schaible T., Sütterlin M, et al. Associated malformations in congenital diaphragmatic hernia. Am J Perinatol. 2011. 28:211–8.
Article33). Jani JC., Peralta CF., Nicolaides KH. Lung-to-head ratio: a need to unify the technique. Ultrasound Obstet Gynecol. 2012. 39:2–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unilateral Congenital Diaphragmatic Eventration Mimicking Congenital Diaphragmatic Hernia
- A Case of Sliding Hiatal Hernia associated with Bochdalek Hernia Repair
- A Case of Congenital Right Diaphragmatic Eventration
- Cardiac Arrest Due to Unrecognized Congenital Diaphragmatic Hernia
- Anesthetic Consideration Concerning a Congenital Diaphragmatic Hernia in a Patient with a Single Ventricle: A case report