Korean J Radiol.
2017 Feb;18(1):18-27. 10.3348/kjr.2017.18.1.18.
Radiology Consultation in the Era of Precision Oncology: A Review of Consultation Models and Services in the Tertiary Setting
- Affiliations
-
- 1Department of Imaging, Dana Farber Cancer Institute, Harvard Medical School, Boston, MA 02215, USA. pdipiro@partners.org
- 2Department of Radiology, Brigham and Women's Hospital, Harvard Medical School, Boston, MA 02215, USA.
- KMID: 2468119
- DOI: http://doi.org/10.3348/kjr.2017.18.1.18
Abstract
- The purpose of the article is to describe the various radiology consultation models in the Era of Precision Medicine. Since the inception of our specialty, radiologists have served as consultants to physicians of various disciplines. A variety of radiology consultation services have been described in the literature, including clinical decision support, patient-centric, subspecialty interpretation, and/or some combination of these. In oncology care in particular, case complexity often merits open dialogue with clinical providers. To explore the utility and impact of radiology consultation services in the academic setting, this article will further describe existing consultation models and the circumstances that precipitated their development. The hybrid model successful at our tertiary cancer center is discussed. In addition, the contributions of a consultant radiologist in breast cancer care are reviewed as the archetype of radiology consultation services provided to oncology practitioners.
MeSH Terms
-
Breast Neoplasms/diagnostic imaging
Decision Support Techniques
Female
Humans
Interprofessional Relations
Oncology Service, Hospital/*organization & administration
Patient-Centered Care/organization & administration
Precision Medicine/*methods
Radiology/*organization & administration
Referral and Consultation/*organization & administration
Tertiary Healthcare/organization & administration
Tomography, X-Ray Computed
Figure
Cited by 1 articles
-
Identification of Preoperative Magnetic Resonance Imaging Features Associated with Positive Resection Margins in Breast Cancer: A Retrospective Study
Jung-Hyun Kang, Ji Hyun Youk, Jeong-Ah Kim, Hye Mi Gweon, Na Lae Eun, Kyung Hee Ko, Eun Ju Son
Korean J Radiol. 2018;19(5):897-904. doi: 10.3348/kjr.2018.19.5.897.
Reference
-
1. Shaikh S, Bafana R, Halabi SS. Concierge and second-opinion radiology: review of current practices. Curr Probl Diagn Radiol. 2016; 45:111–114.2. Shuman WP, Heilman RS. The radiologist as a consultant. JAMA. 1979; 242:1519–1520.3. Baker SR. The operation of a radiology consultation service in an acute care hospital. JAMA. 1982; 248:2152–2154.4. Baker SR, Rosenberg ZS, Adel H. The operation of a ward-based radiology consultation service. Radiology. 1984; 152:331–333.5. Baker SR, Stein HD. Radiologic consultation: its application to an acute care surgical ward. AJR Am J Roentgenol. 1986; 147:637–640.6. Seltzer SE, Beard JO, Adams DF. Radiologist as consultant: direct contact between referring clinician and radiologist before CT examination. AJR Am J Roentgenol. 1985; 144:661–664.7. Khorasani R, Silverman SG, Meyer JE, Gibson M, Weissman BN, Seltzer SE. Design and implementation of a new radiology consultation service in a teaching hospital. AJR Am J Roentgenol. 1994; 163:457–459.8. Bree RL, Kazerooni EA, Katz SJ. Effect of mandatory radiology consultation on inpatient imaging use. A randomized controlled trial. JAMA. 1996; 276:1595–1598.9. Gottlieb RH, Hollenberg GM, Fultz PJ, Rubens DJ. Radiologic consultation: effect on inpatient diagnostic imaging evaluation in a teaching hospital. Acad Radiol. 1997; 4:217–221.10. Reiner B, Siegel E, Protopapas Z, Hooper F, Ghebrekidan H, Scanlon M. Impact of filmless radiology on frequency of clinician consultations with radiologists. AJR Am J Roentgenol. 1999; 173:1169–1172.11. Tillack AA, Borgstede JP. An evaluation of the impact of clinically embedded reading rooms on radiologist-referring clinician communication. J Am Coll Radiol. 2013; 10:368–372.12. American College of Radiology. Imaging 3.0™. Accessed January 17, 2016. http://www.acr.org/Advocacy/Economics-Health-Policy/Imaging-3.13. Sherman RS. Whom do we serve? Radiology. 1966; 87:147–148.14. Liston SE. A new type of cancer lawsuit is emerging. ACR Bulletin. 1990; 46:14.15. Berlin L. Communicating results of all radiologic examinations directly to patients: has the time come? AJR Am J Roentgenol. 2007; 189:1275–1282.16. Peteet JR, Stomper PC, Ross DM, Cotton V, Truesdell P, Moczynski W. Emotional support for patients with cancer who are undergoing CT: semistructured interviews of patients at a cancer institute. Radiology. 1992; 182:99–102.17. Schreiber MH, Leonard M Jr, Rieniets CY. Disclosure of imaging findings to patients directly by radiologists: survey of patients' preferences. AJR Am J Roentgenol. 1995; 165:467–469.18. Schreiber MH. Direct disclosure by radiologists of imaging findings to patients: a survey of radiologists and medical staff members. AJR Am J Roentgenol. 1996; 167:1091–1093.19. Basu PA, Ruiz-Wibbelsmann JA, Spielman SB, Van Dalsem VF 3rd, Rosenberg JK, Glazer GM. Creating a patient-centered imaging service: determining what patients want. AJR Am J Roentgenol. 2011; 196:605–610.20. Pahade J, Couto C, Davis RB, Patel P, Siewert B, Rosen MP. Reviewing imaging examination results with a radiologist immediately after study completion: patient preferences and assessment of feasibility in an academic department. AJR Am J Roentgenol. 2012; 199:844–851.21. Mangano MD, Rahman A, Choy G, Sahani DV, Boland GW, Gunn AJ. Radiologists' role in the communication of imaging examination results to patients: perceptions and preferences of patients. AJR Am J Roentgenol. 2014; 203:1034–1039.22. Cabarrus M, Naeger DM, Rybkin A, Qayyum A. Patients prefer results from the ordering provider and access to their radiology reports. J Am Coll Radiol. 2015; 12:556–562.23. Mangano MD, Bennett SE, Gunn AJ, Sahani DV, Choy G. Creating a patient-centered radiology practice through the establishment of a diagnostic radiology consultation clinic. AJR Am J Roentgenol. 2015; 205:95–99.24. Neiman HL. Face of Radiology campaign. Acad Radiol. 2009; 16:517–520.25. Sullivan CL, Pandya A, Min RJ, Drotman M, Hentel K. The development and implementation of a patient-centered radiology consultation service: a focus on breast density and additional screening options. Clin Imaging. 2015; 39:731–734.26. Franken EA Jr, Berbaum KS, Brandser EA, D'Alessandro MP, Schweiger GD, Smith WL. Pediatric radiology at a rural hospital: value of teleradiology and subspecialty consultation. AJR Am J Roentgenol. 1997; 168:1349–1352.27. Mullerad M, Hricak H, Wang L, Chen HN, Kattan MW, Scardino PT. Prostate cancer: detection of extracapsular extension by genitourinary and general body radiologists at MR imaging. Radiology. 2004; 232:140–146.28. Brook OR, Hakmon T, Brook A, Dudnik E, Kuten A, Engel A. The effect of a Radiology Conference consultation on cancer patients management. Ann Oncol. 2011; 22:1204–1208.29. Loevner LA, Sonners AI, Schulman BJ, Slawek K, Weber RS, Rosenthal DI, et al. Reinterpretation of cross-sectional images in patients with head and neck cancer in the setting of a multidisciplinary cancer center. AJNR Am J Neuroradiol. 2002; 23:1622–1626.30. Lysack JT, Hoy M, Hudon ME, Nakoneshny SC, Chandarana SP, Matthews TW, et al. Impact of neuroradiologist second opinion on staging and management of head and neck cancer. J Otolaryngol Head Neck Surg. 2013; 42:39.31. Mallory MA, Losk K, Lin NU, Sagara Y, Birdwell RL, Cutone L, et al. The influence of radiology image consultation in the surgical management of breast cancer patients. Ann Surg Oncol. 2015; 22:3383–3388.32. Chalian M, Del Grande F, Thakkar RS, Jalali SF, Chhabra A, Carrino JA. Second-opinion subspecialty consultations in musculoskeletal radiology. AJR Am J Roentgenol. 2016; 206:1217–1221.33. Dickerson EC, Alam HB, Brown RK, Stojanovska J, Davenport MS. Michigan Radiology Quality Collaborative. In-person communication between radiologists and acute care surgeons leads to significant alterations in surgical decision making. J Am Coll Radiol. 2016; 13:943–949.34. Yousem DM. Establishing an outside film reading service/dealing with turf issues: unintended consequences. J Am Coll Radiol. 2010; 7:480–481.35. DiPiro PJ, vanSonnenberg E, Tumeh SS, Ros PR. Volume and impact of second-opinion consultations by radiologists at a tertiary care cancer center: data. Acad Radiol. 2002; 9:1430–1433.36. Fennell ML, Das IP, Clauser S, Petrelli N, Salner A. The organization of multidisciplinary care teams: modeling internal and external influences on cancer care quality. J Natl Cancer Inst Monogr. 2010; 2010:72–80.37. Van den Abbeele AD, Krajewski KM, Tirumani SH, Fennessy FM, DiPiro PJ, Nguyen QD, et al. Cancer imaging at the crossroads of precision medicine: perspective from an academic imaging department in a comprehensive cancer center. J Am Coll Radiol. 2016; 13:365–371.38. Jacene H, DiPiro P, Bellon J, Nakhlis F, Hirshfield-Bartek J, Yeh E, et al. Discrepancy between CT and FDG-PET/CT in the staging of patients with inflammatory breast cancer: implications for radiation therapy treatment planning. Cancer Res. 2012; 72:24 Suppl. Abstract nr P5-02-01.39. Hamaoka T, Madewell JE, Podoloff DA, Hortobagyi GN, Ueno NT. Bone imaging in metastatic breast cancer. J Clin Oncol. 2004; 22:2942–2953.40. Norbash A, Bluth E, Lee CI, Francavilla M, Donner M 3rd, Dutton SC, et al. Radiologist manpower considerations and Imaging 3.0: effort planning for value-based imaging. J Am Coll Radiol. 2014; 11:953–958.41. Duong PA, Bresnahan B, Pastel DA, Sadigh G, Ballard D, Sullivan JC, et al. Value of imaging part I: perspectives for the academic radiologist. Acad Radiol. 2016; 23:18–22.42. Duong PA, Pastel DA, Sadigh G, Ballard D, Sullivan JC, Bresnahan B, et al. The value of imaging part II: value beyond Image interpretation. Acad Radiol. 2016; 23:23–29.
- Full Text Links
- Actions
-
Cited
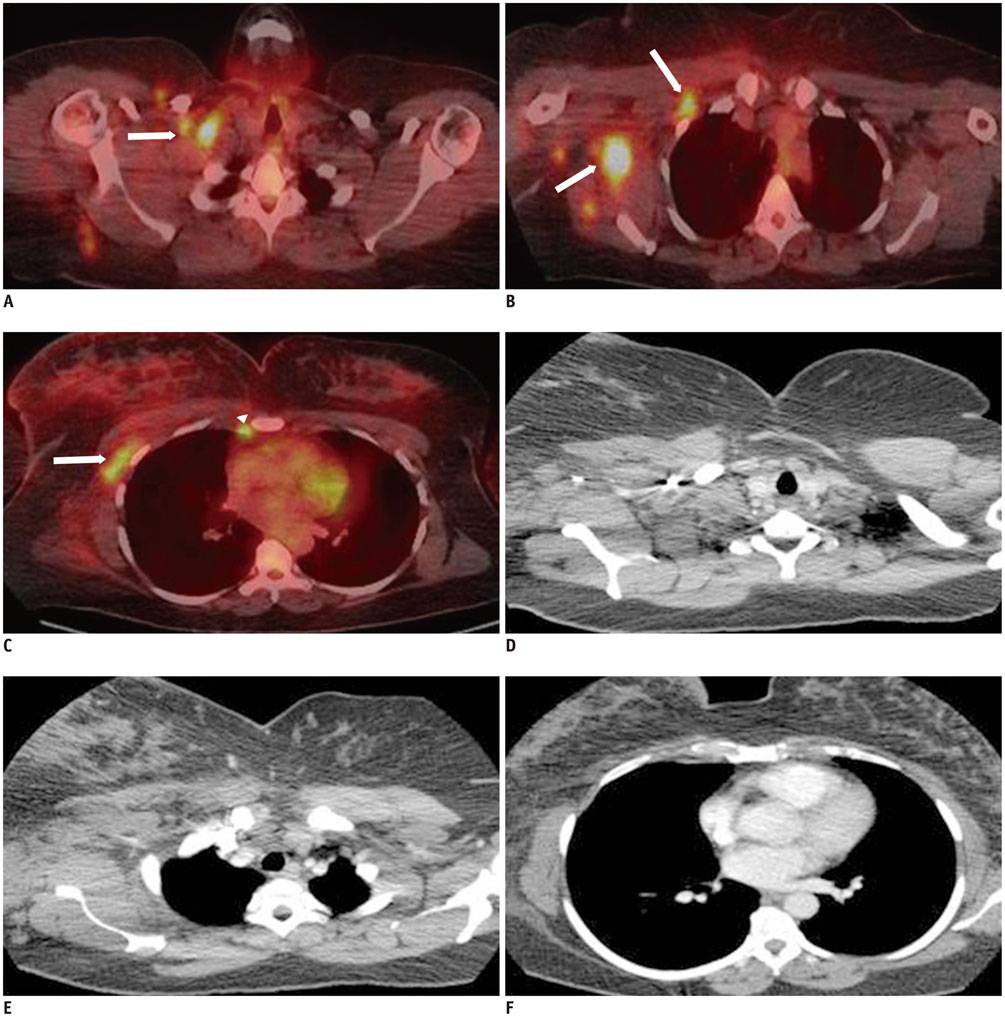
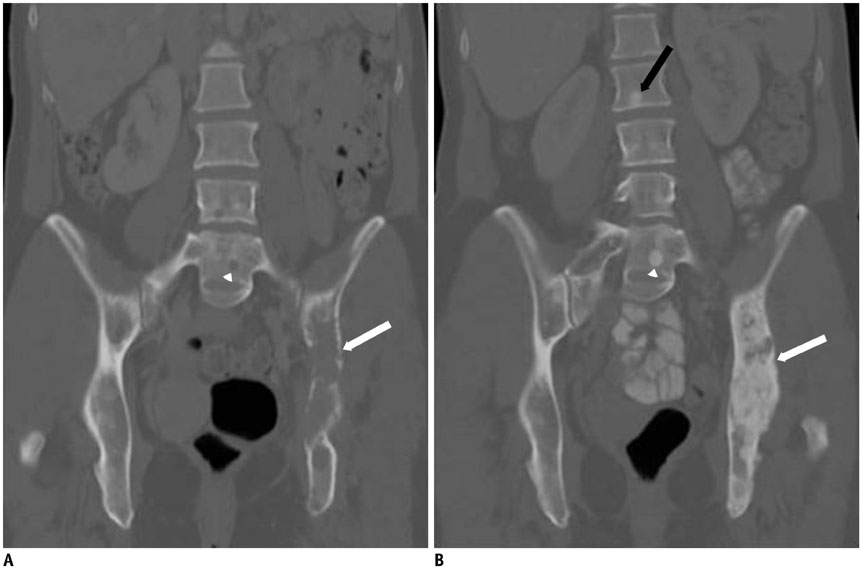
- CITED
-
- Close
- Share
- Similar articles
-
- A Study on the Characteristics and Consultation Request Type of Inpatients Referred for Depressive Symptoms
- A Study on the Characteristics and Consultation Type of Inpatients Referred for Delirium and Depressive Disorder
- An exploratory study of the patients for the consultation and use of preventive dental service
- Doctor Consultation through Mobile Applications in India: An Overview, Challenges and the Way Forward
- Other Physicians' Recognition and Satisfaction to the Psychiatric Consultation Service in a University Hospital