Korean Circ J.
2020 Feb;50(2):148-159. 10.4070/kcj.2019.0219.
Clinical Implications of Preoperative Nonvalvular Atrial Fibrillation with Respect to Postoperative Cardiovascular Outcomes in Patients Undergoing Non-Cardiac Surgery
- Affiliations
-
- 1Department of Cardiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea. mdjunkim@gmail.com
- 2Division of Cardiology, Department of Internal Medicine, Keimyung University Dongsan Hospital, Daegu, Korea.
- 3Department of Clinical Epidemiology and Biostatistics, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- KMID: 2468041
- DOI: http://doi.org/10.4070/kcj.2019.0219
Abstract
- BACKGROUND AND OBJECTIVES
Atrial fibrillation (AF) is associated with a higher long-term risk of major cardiovascular events. However, its clinical implications with respect to peri-operative cardiovascular outcomes in patients undergoing non-cardiac surgery is unclear. We tried to examine the association between pre-operative AF and peri-operative cardiovascular outcomes.
METHODS
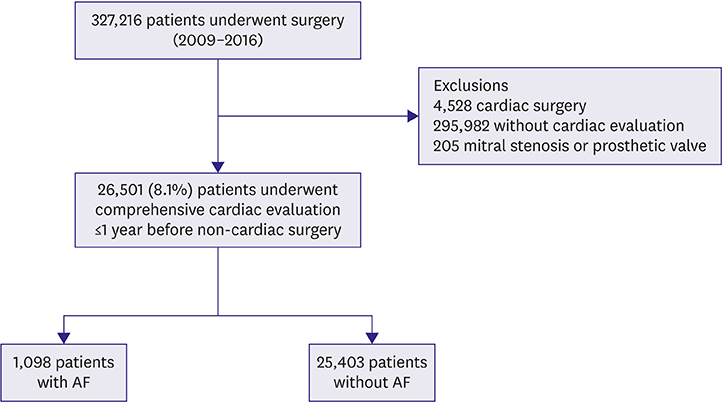
We retrospectively analyzed data from 26,501 consecutive patients who underwent comprehensive preoperative cardiac evaluations for risk stratification prior to receiving non-cardiac surgery at our center. Preoperative AF was diagnosed in 1,098 patients (4.1%), and their cardiovascular outcomes were compared with those of patients without AF. The primary outcome was the rate of major adverse cardiac and cerebrovascular events (MACCE) during immediate post-surgery period (<30 days).
RESULTS
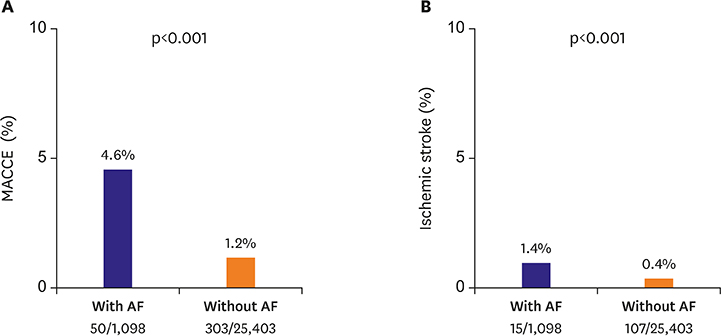
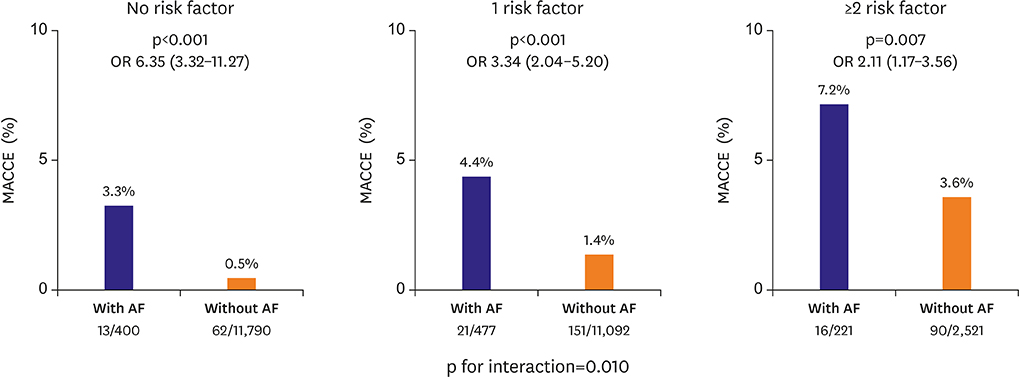
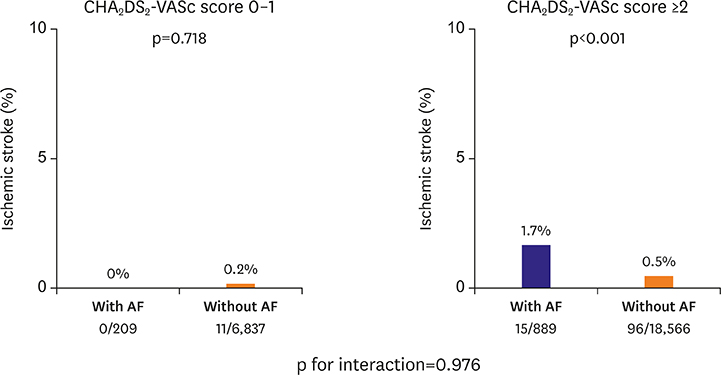
Patients with AF were older and had higher proportion of male sex, higher rate of extra-cardiac comorbidities, higher CHAâ‚‚DSâ‚‚-VASc score, and higher revised cardiac risk index (RCRI) compared with those without AF. The rate of MACCE was significantly higher in AF patients compared to non-AF patients (4.6% vs. 1.2%, p<0.001). Preoperative AF was associated with higher risk of MACCE, even after multivariable adjustment (odds ratio, 2.97; 95% confidence interval, 2.13-4.07, p<0.001). The relative contribution of AF to MACCE was larger in patients with lower RCRI (p for interaction=0.010). The discriminating performance of RCRI was significantly enhanced by addition of AF.
CONCLUSIONS
In patients undergoing non-cardiac surgery, preoperative AF was associated with a higher risk of peri-operative cardiovascular outcomes.
Keyword
Figure
Cited by 1 articles
-
Atrial Fibrillation as a Risk Factor for Major Adverse Cardiac and Cerebrovascular Events after Non-cardiac Surgery
Dong Geum Shin, Hong Euy Lim
Korean Circ J. 2020;50(2):160-162. doi: 10.4070/kcj.2019.0386.
Reference
-
1. Stewart S, Hart CL, Hole DJ, McMurray JJ. A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Am J Med. 2002; 113:359–364.
Article2. Priebe HJ. Triggers of perioperative myocardial ischaemia and infarction. Br J Anaesth. 2004; 93:9–20.
Article3. Grau AJ, Eicke M, Burmeister C, Hardt R, Schmitt E, Dienlin S. Risk of ischemic stroke and transient ischemic attack is increased up to 90 days after non-carotid and non-cardiac surgery. Cerebrovasc Dis. 2017; 43:242–249.
Article4. Smilowitz NR, Gupta N, Ramakrishna H, Guo Y, Berger JS, Bangalore S. Perioperative major adverse cardiovascular and cerebrovascular events associated with noncardiac surgery. JAMA Cardiol. 2017; 2:181–187.
Article5. Longstreth WT Jr, Bernick C, Fitzpatrick A, et al. Frequency and predictors of stroke death in 5,888 participants in the Cardiovascular Health Study. Neurology. 2001; 56:368–375.
Article6. Kaatz S, Douketis JD, Zhou H, Gage BF, White RH. Risk of stroke after surgery in patients with and without chronic atrial fibrillation. J Thromb Haemost. 2010; 8:884–890.
Article7. Urbanek C, Palm F, Buggle F, et al. Recent surgery or invasive procedures and the risk of stroke. Cerebrovasc Dis. 2014; 38:370–376.
Article8. Gupta PK, Gupta H, Sundaram A, et al. Development and validation of a risk calculator for prediction of cardiac risk after surgery. Circulation. 2011; 124:381–387.
Article9. Kristensen SD, Knuuti J, Saraste A, et al. 2014 ESC/ESA Guidelines on non-cardiac surgery: cardiovascular assessment and management: The Joint Task Force on non-cardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA). Eur Heart J. 2014; 35:2383–2431.10. McAlister FA, Jacka M, Graham M, et al. The prediction of postoperative stroke or death in patients with preoperative atrial fibrillation undergoing non-cardiac surgery: a VISION sub-study. J Thromb Haemost. 2015; 13:1768–1775.
Article11. Hollenberg M, Mangano DT, Browner WS, et al. Predictors of postoperative myocardial ischemia in patients undergoing noncardiac surgery. JAMA. 1992; 268:205–209.
Article12. Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999; 100:1043–1049.
Article13. January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014; 64:e1–76.14. Baumgartner H, Hung J, Bermejo J, et al. Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice. Eur J Echocardiogr. 2009; 10:1–25.
Article15. Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2012; 60:e44–164.16. Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010; 137:263–272.17. Hicks KA, Tcheng JE, Bozkurt B, et al. 2014 ACC/AHA key data elements and definitions for cardiovascular endpoint events in clinical trials: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Data Standards (Writing Committee to Develop Cardiovascular Endpoints Data Standards). J Am Coll Cardiol. 2015; 66:403–469.18. Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Eur Heart J. 2012; 33:2551–2567.19. Goldman L, Caldera DL, Nussbaum SR, et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med. 1977; 297:845–850.
Article20. van Diepen S, Bakal JA, McAlister FA, Ezekowitz JA. Mortality and readmission of patients with heart failure, atrial fibrillation, or coronary artery disease undergoing noncardiac surgery: an analysis of 38 047 patients. Circulation. 2011; 124:289–296.21. Botto F, Alonso-Coello P, Chan MT, et al. Myocardial injury after noncardiac surgery: a large, international, prospective cohort study establishing diagnostic criteria, characteristics, predictors, and 30-day outcomes. Anesthesiology. 2014; 120:564–578.22. Raymond RJ, Lee AJ, Messineo FC, Manning WJ, Silverman DI. Cardiac performance early after cardioversion from atrial fibrillation. Am Heart J. 1998; 136:435–442.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long-Term Outcomes of Preoperative Atrial Fibrillation in Cardiac Surgery
- Risk Factors of Atrial Fibrillation after Coronary Artery Bypass Grafting
- A Comparative Study on Cerebral Infarction in Patient with Nonvalvular and Valvular Atrial Fibrillation
- Surgical Management for Chronic Atrial Fibrillation
- Application of New Oral Anticoagulants: Prevention of Stroke in Patients with Nonvalvular Atrial Fibrillation