Kosin Med J.
2019 Dec;34(2):168-172. 10.7180/kmj.2019.34.2.168.
Aortoiliac Occlusive Disease as a Cause of Allograft Kidney Dysfunction and Refractory Hypertension
- Affiliations
-
- 1Department of surgery, Seoul Paik hospital, Inje University, Korea. Jin.theDoc@gmail.com
- KMID: 2467978
- DOI: http://doi.org/10.7180/kmj.2019.34.2.168
Abstract
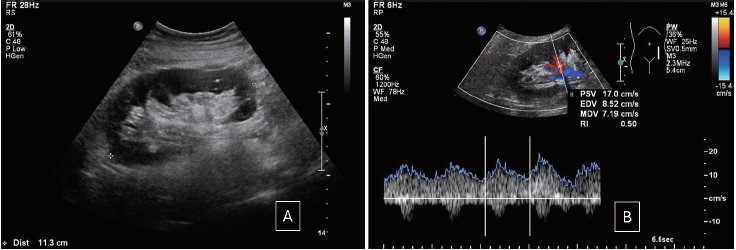
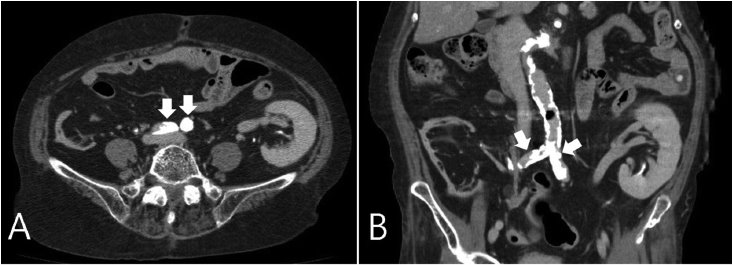
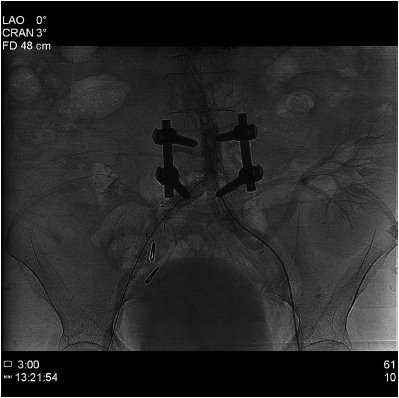
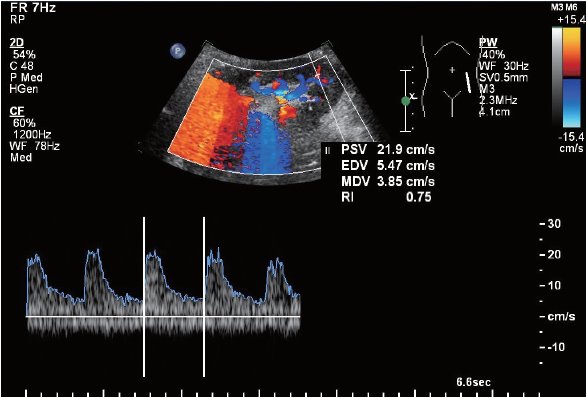
- Aortoiliac occlusive disease (AIOD), especially proximal to the transplant artery, in kidney transplant patient activates the renin-angiotensin-aldosterone system by limiting graft renal perfusion and causes symptoms that can occur with transplant renal artery stenosis (TRAS) such as refractory hypertension, water retention, and graft renal dysfunction. Immediate clinical suspicion is difficult due to the nature of the progressive disease unlike TRAS. Herein, we present an interesting case of bilateral common iliac artery occlusion (AIOD, TASC II, type C) that manifested as uncontrolled blood pressure and decreased allograft function in a patient who had kidney transplant 17 years ago. The patient was successfully diagnosed with duplex scan, ankle-brachial index (ABI) and computed tomography angiography and treated with percutaneous luminal angioplasty and stent graft insertion.
MeSH Terms
Figure
Reference
-
1. Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG, et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). Eur J Vasc Endovasc Surg. 2007; 33:Suppl 1. S5–75.
Article2. Bracale UM, Giribono AM, Spinelli D, Del Guercio L, Pipitò N, Ferrara D, et al. Long-term Results of Endovascular Treatment of TASC C and D Aortoiliac Occlusive Disease with Expanded Polytetrafluoroethylene Stent Graft. Ann Vasc Surg. 2019; 56:254–260.
Article3. Mwipatayi BP, Sharma S, Daneshmand A, Thomase SD, Vijayan V, Altaf N, et al. Durability of the balloon-expandable covered versus bare-metal stents in the Covered versus Balloon Expandable Stent Trial (COBEST) for the treatment of aortoiliac occlusive disease. J Vasc Surg. 2016; 64:83–94.e1.
Article4. Bruno S, Remuzzi G, Ruggenenti P. Transplant renal artery stenosis. J Am Soc Nephrol. 2004; 15:134–141.
Article5. Coemans M, Süsal C, Döhler B, Anglicheau D, Giral M, Bestard O, et al. Analyses of the short- and long-term graft survival after kidney transplantation in Europe between 1986 and 2015. Kidney Int. 2018; 94:964–973.
Article6. Becker BN, Odorico JS, Becker YT, Leverson G, McDermott JC, Grist T, et al. Peripheral vascular disease and renal transplant artery stenosis: a reappraisal of transplant renovascular disease. Clin Transplant. 1999; 13:349–355.
Article7. Voiculescu A, Hollenbeck M, Plum J, Hetzel GR, Mödder U, Pfeiffer T, et al. Iliac artery stenosis proximal to a kidney transplant: clinical findings, duplex-sonographic criteria, treatment, and outcome. Transplantation. 2003; 76:332–339.
Article8. Misra S, Shishehbor MH, Takahashi EA, Aronow HD, Brewster LP, Bunte MC, et al. Perfusion Assessment in Critical Limb Ischemia: Principles for Understanding and the Development of Evidence and Evaluation of Devices: A Scientific Statement From the American Heart Association. Circulation. 2019; 140:e657–e672.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The accidental renal artery embolism in patient with aortoiliac occlusive disease with unilateral renal atrophy during aortobifemoral bypass graft: A case report
- Asymptomatic Common Iliac Artery Stenosis as a Cause of Renal Allograft Dysfunction and Uncontrolled Hypertension
- Single Tract Aortic Revascularization Technique in the Treatment of Aortoiliac Occlusive Disease
- Internal Thoracic Artery Collateral to the External Iliac Artery in Chronic Aortoiliac Occlusive Disease
- Treatment of Aortoiliac Occlusions According to Multiple Competiting Therapeutic Options