Electrolyte Blood Press.
2019 Dec;17(2):25-35. 10.5049/EBP.2019.17.2.25.
Effect of Renin-Angiotensin System Blockade on Mortality in Korean Hypertensive Patients with Proteinuria
- Affiliations
-
- 1Ewha Institute of Convergence Medicine, Ewha Womans University Mokdong Hospital, Seoul, Korea.
- 2Institute of Life and Death Studies, Hallym University, Chuncheon, Korea.
- 3School of Medicine, Ewha Womans University, Seoul, Korea. drryu@ewha.ac.kr
- 4Tissue Injury Defense Research Center, Ewha Womans University, Seoul, Korea.
- KMID: 2467958
- DOI: http://doi.org/10.5049/EBP.2019.17.2.25
Abstract
- BACKGROUND
Although renin-angiotensin system (RAS) blockade is recommended for hypertensive patients with proteinuria, the effect of RAS blockade on Korean hypertensive patients has not been investigated.
METHODS
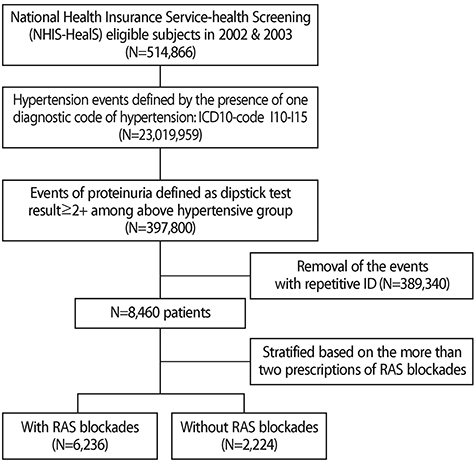
Among individuals who underwent a National Health Examination between 2002 and 2003 in Korea, hypertensive patients with proteinuria (defined as a dipstick test result ≥2+) were enrolled in this study. We investigated the outcomes of two groups stratified by RAS blockade prescription (with RAS blockade vs. without RAS blockade). Moreover, Cox proportional hazard regression and Kaplan-Meier analyses were performed to examine the effects of RAS blockade on mortality and end-stage renal disease (ESRD).
RESULTS
A total of 8,460 patients were enrolled in this study, of whom 6,236 (73.7%) were prescribed with RAS blockade. The mean follow-up period was 129 months. A total of 1,003 (11.9%) patients died, of whom 273 (3.2%) died of cardiovascular (CV) events. The Kaplan-Meier curves for all-cause or CV mortality showed that the survival probability was significantly higher in the RAS blockade group than in the non-RAS blockade group. Multivariate Cox analysis also revealed RAS blockade significantly reduced the all-cause and CV mortality rates by 39.1% and 33.7%, respectively, compared with non-RAS blockade, even after adjusting for age, sex, and comorbid diseases; however, ESRD was not affected.
CONCLUSION
In this study, we found that RAS blockade was significantly associated with a reduction in mortality but not in the incidence of ESRD. However, 26.3% of the enrolled patients did not use RAS blockade. Physicians need to consider the usefulness of RAS blockade in hypertensive patients with proteinuria.
Keyword
MeSH Terms
Figure
Reference
-
1. Dinneen SF, Gerstein HC. The association of microalbuminuria and mortality in non-insulin-dependent diabetes mellitus. A systematic overview of the literature. Archives of Internal Medicine. 1997; 157(13):1413–1418.
Article2. Hillege HL, Fidler V, Diercks GF, et al. Urinary albumin excretion predicts cardiovascular and noncardiovascular mortality in general population. Circulation. 2002; 106(14):1777–1782.
Article3. Jafar TH, Stark PC, Schmid CH, et al. Proteinuria as a modifiable risk factor for the progression of non-diabetic renal disease. Kidney International. 2001; 60(3):1131–1140.
Article4. Mann JF, Gerstein HC, Yi QL, et al. Development of renal disease in people at high cardiovascular risk: results of the HOPE randomized study. Journal of the American Society of Nephrology: JASN. 2003; 14(3):641–647.
Article5. Atkins RC, Briganti EM, Lewis JB, et al. Proteinuria reduction and progression to renal failure in patients with type 2 diabetes mellitus and overt nephropathy. American Journal of Kidney Diseases: the Official Journal of the National Kidney Foundation. 2005; 45(2):281–287.
Article6. Asselbergs FW, Diercks GF, Hillege HL, et al. : Effects of fosinopril and pravastatin on cardiovascular events in subjects with microalbuminuria. Circulation. 2004; 110(18):2809–2816.
Article7. White SL, Yu R, Craig JC, Polkinghorne KR, Atkins RC, Chadban SJ. Diagnostic accuracy of urine dipsticks for detection of albuminuria in the general community. American Journal of Kidney Diseases: the Official Journal of the National Kidney Foundation. 2011; 58(1):19–28.
Article8. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. American Journal of Kidney Diseases: the Official Journal of the National Kidney Foundation. 2002; 39(2 Suppl 1):S1–S266.9. Lamb EJ, MacKenzie F, Stevens PE. How should proteinuria be detected and measured? Annals of Clinical Biochemistry. 2009; 46(Pt 3):205–217.
Article10. Pesola GR, Argos M, Chen Y, et al. Dipstick proteinuria as a predictor of all-cause and cardiovascular disease mortality in Bangladesh: a prospective cohort study. Preventive Medicine. 2015; 78:72–77.
Article11. Rao MV, Qiu Y, Wang C, Bakris G. Hypertension and CKD: Kidney Early Evaluation Program(KEEP) and National Health and Nutrition Examination Survey (NHANES), 1999-2004. American Journal of Kidney Diseases: the Official Journal of the National Kidney Foundation. 2008; 51(4 Suppl 2):S30–S37.12. Coresh J, Wei GL, McQuillan G, et al. Prevalence of high blood pressure and elevated serum creatinine level in the United States: findings from the third National Health and Nutrition Examination Survey (1988-1994). Archives of Internal Medicine. 2001; 161(9):1207–1216.
Article13. Breyer JA, Bain RP, Evans JK, et al. Predictors of the progression of renal insufficiency in patients with insulin-dependent diabetes and overt diabetic nephropathy. The Collaborative Study Group. Kidney International. 1996; 50(5):1651–1658.
Article14. Peterson JC, Adler S, Burkart JM, et al. Blood pressure control, proteinuria, and the progression of renal disease. The Modification of Diet in Renal Disease Study. Annals of Internal Medicine. 1995; 123(10):754–762.
Article15. Randomised placebo-controlled trial of effect of ramipril on decline in glomerular filtration rate and risk of terminal renal failure in proteinuric, non-diabetic nephropathy. The GISEN Group (Gruppo Italiano di Studi Epidemiologici in Nefrologia). Lancet. 1997; 349(9069):1857–1863.16. Botdorf J, Chaudhary K, Whaley-Connell A. Hypertension in cardiovascular and kidney disease. Cardiorenal Medicine. 2011; 1(3):183–119.
Article17. Segura J, Ruilope LM. Hypertension in moderate-tosevere nondiabetic CKD patients. Advances in Chronic Kidney Disease. 2011; 18(1):23–22.
Article18. de Zeeuw D, Remuzzi G, Parving HH, et al. : Proteinuria, a target for renoprotection in patients with type 2 diabetic nephropathy: lessons from RENAAL. Kidney International. 2004; 65(6):2309–2320.
Article19. Irie F, Iso H, Sairenchi T, et al. : The relationships of proteinuria, serum creatinine, glomerular filtration rate with cardiovascular disease mortality in Japanese general population. Kidney International. 2006; 69(7):1264–1271.
Article20. Lewis EJ, Hunsicker LG, Clarke WR, et al. : Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. The New England Journal of Medicine. 2001; 345(12):851–860.
Article21. Chobanian AV, Bakris GL, Black HR, et al. : The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 Report. JAMA. 2003; 289(19):2560–2572.
Article22. Introduction: the American Diabetes Association's (ADA) evidence-based practice guidelines, standards, and related recommendations and documents for diabetes care. Diabetes Care. 2012; 35 Suppl 1:S1–S2.23. Sarafidis PA, Khosla N, Bakris GL. Antihypertensive therapy in the presence of proteinuria. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2007; 49(1):12–26.
Article24. Yoshioka T, Rennke HG, Salant DJ, Deen WM, Ichikawa I. Role of abnormally high transmural pressure in the permselectivity defect of glomerular capillary wall: a study in early passive Heymann nephritis. Circulation Research. 1987; 61(4):531–553.
Article25. Kunz R, Friedrich C, Wolbers M, Mann JF. Meta-analysis: effect of monotherapy and combination therapy with inhibitors of the renin angiotensin system on proteinuria in renal disease. Annals of Internal Medicine. 2008; 148(1):30–34.
Article26. Gansevoort RT, Sluiter WJ, Hemmelder MH, de Zeeuw D, de Jong PE. Antiproteinuric effect of blood-pressure-lowering agents: a meta-analysis of comparative trials. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association. 1995; 10(11):1963–1974.27. Li PK, Leung CB, Chow KM, et al. Hong Kong study using valsartan in IgA nephropathy (HKVIN): a doubleblind, randomized, placebo-controlled study. American Journal of Kidney Diseases: the Official Journal of the National Kidney Foundation. 2006; 47(5):751–760.
Article28. Nickenig G, Harrison DG. The AT(1)-type angiotensin receptor in oxidative stress and atherogenesis: part I: oxidative stress and atherogenesis. Circulation. 2002; 105(3):393–339.
Article29. Perticone F, Ceravolo R, Pujia A, et al. : Prognostic significance of endothelial dysfunction in hypertensive patients. Circulation. 2001; 104(2):191–196.
Article30. Quyyumi AA. Endothelial function in health and disease: new insights into the genesis of cardiovascular disease. The American Journal of Medicine. 1998; 105(1a):32s–39s.
Article31. Schmieder RE. Endothelial dysfunction: how can one intervene at the beginning of the cardiovascular continuum? Journal of hypertension. Supplement : official journal of the International Society of Hypertension. 2006; 24(2):S31–S35.
Article32. Wassmann S, Nickenig G. Pathophysiological regulation of the AT1-receptor and implications for vascular disease. Journal of hypertension. Supplement : official journal of the International Society of Hypertension. 2006; 24(1):S15–S21.
Article33. Weber M. The telmisartan programme of research tO show Telmisartan End-organ proteCTION (PROTECTION) programme. Journal of hypertension. Supplement : official journal of the International Society of Hypertension. 2003; 21(6):S37–S46.
Article34. Brenner BM, Cooper ME, de Zeeuw D, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. The New England Journal of Medicine. 2001; 345(12):861–869.
Article35. Hou FF, Zhang X, Zhang GH, et al. Efficacy and safety of benazepril for advanced chronic renal insufficiency. The New England Journal of Medicine. 2006; 354(2):131–140.
Article36. Maschio G, Alberti D, Janin G, et al. Effect of the angiotensin-converting-enzyme inhibitor benazepril on the progression of chronic renal insufficiency. The Angioten sin-Converting-Enzyme Inhibition in Progressive Renal Insufficiency Study Group. The New England Journal of Medicine. 1996; 334(15):939–945.
Article37. Lee JH, Kwon YE, Park JT, et al. The effect of reninangiotensin system blockade on renal protection in chronic kidney disease patients with hyperkalemia. Journal of the Renin-angiotensin-aldosterone System: JRAAS. 2014; 15(4):491–497.
Article38. Rahman M, Pressel S, Davis BR, et al. Renal outcomes in high-risk hypertensive patients treated with an angiotensin-converting enzyme inhibitor or a calcium channel blocker vs a diuretic: a report from the antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT). Archives of Internal Medicine. 2005; 165(8):936–946.
Article39. Lewis EJ, Hunsicker LG, Bain RP, Rohde RD. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The Collaborative Study Group. The New England Journal of Medicine. 1993; 329(20):1456–1462.
Article40. Jafar TH, Schmid CH, Landa M, et al. Angiotensin-converting enzyme inhibitors and progression of nondiabetic renal disease. A meta-analysis of patient-level data. Annals of Internal Medicine. 2001; 135(2):73–87.
Article41. Ruggenenti P, Perna A, Gherardi G, et al. Renoprotective properties of ACE-inhibition in non-diabetic nephropathies with non-nephrotic proteinuria. Lancet. 1999; 354(9176):359–364. DOI: 10.1016/S0140-6736(98)10363-X. Epub 1999/08/07. PMID: 10437863.
Article42. Giatras I, Lau J, Levey AS. Effect of angiotensin-converting enzyme inhibitors on the progression of nondiabetic renal disease: a meta-analysis of randomized trials. Angiotensin-Converting-Enzyme Inhibition and Progressive Renal Disease Study Group. Annals of Internal Medicine. 1997; 127(5):337–345. Epub 1997/09/01. PMID: 9273824.
Article43. UK Prospective Diabetes Study Group. Efficacy of atenolol and captopril in reducing risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 39. UK Prospective Diabetes Study Group. BMJ. 1998; 317(7160):713–720. Epub 1998/09/11. PubMed Central PMCID: PMC28660. PMID:9732338.44. Suissa S, Hutchinson T, Brophy JM, et al. ACE-inhibitor use and the long-term risk of renal failure in diabetes. Kidney International. 2006; 69(5):913–919. DOI: 10.1038/sj.ki.5000159. Epub 2006/03/07. PMID:16518351.
Article45. Mann JF, Schmieder RE, McQueen M, et al. Renal outcomes with telmisartan, ramipril, or both, in people at high vascular risk (the ONTARGET study): a multicentre, randomised, double-blind, controlled trial. Lancet. 2008; 372(9638):547–553. DOI: 10.1016/S0140-6736(08)61236-2. Epub 2008/08/19. PMID: 18707986.
Article46. Oh YJ, Kim SM, Shin BC, et al. The impact of renin-angiotensin system blockade on renal outcomes and mortality in pre-dialysis patients with advanced chronic kidney disease. PLoS One. 2017; 12(1):e0170874. DOI: 10.1371/journal.pone.0170874.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Does Dual Renin-Angiotensin System Blockade Therapy Have Still Value in the Management of Chronic Kidney Disease with Proteinuria after ONTARGET Study?
- Renin Angiotensin System in Rabbit Corpus Cavernosum: Functional Characterization of Angiotensin II Receptors
- Renin-Angiotensin-Aldosterone System Blockade and Renal Protection in Diabetic Nephropathy
- Renal Interstitial Fibrosis and Renin Angiotensin System Inhibition
- Effect of Pinealectomy on the Renin-Angiotensin System in Sprague-Dawley Rats