J Korean Soc Spine Surg.
2019 Dec;26(4):172-177. 10.4184/jkss.2019.26.4.172.
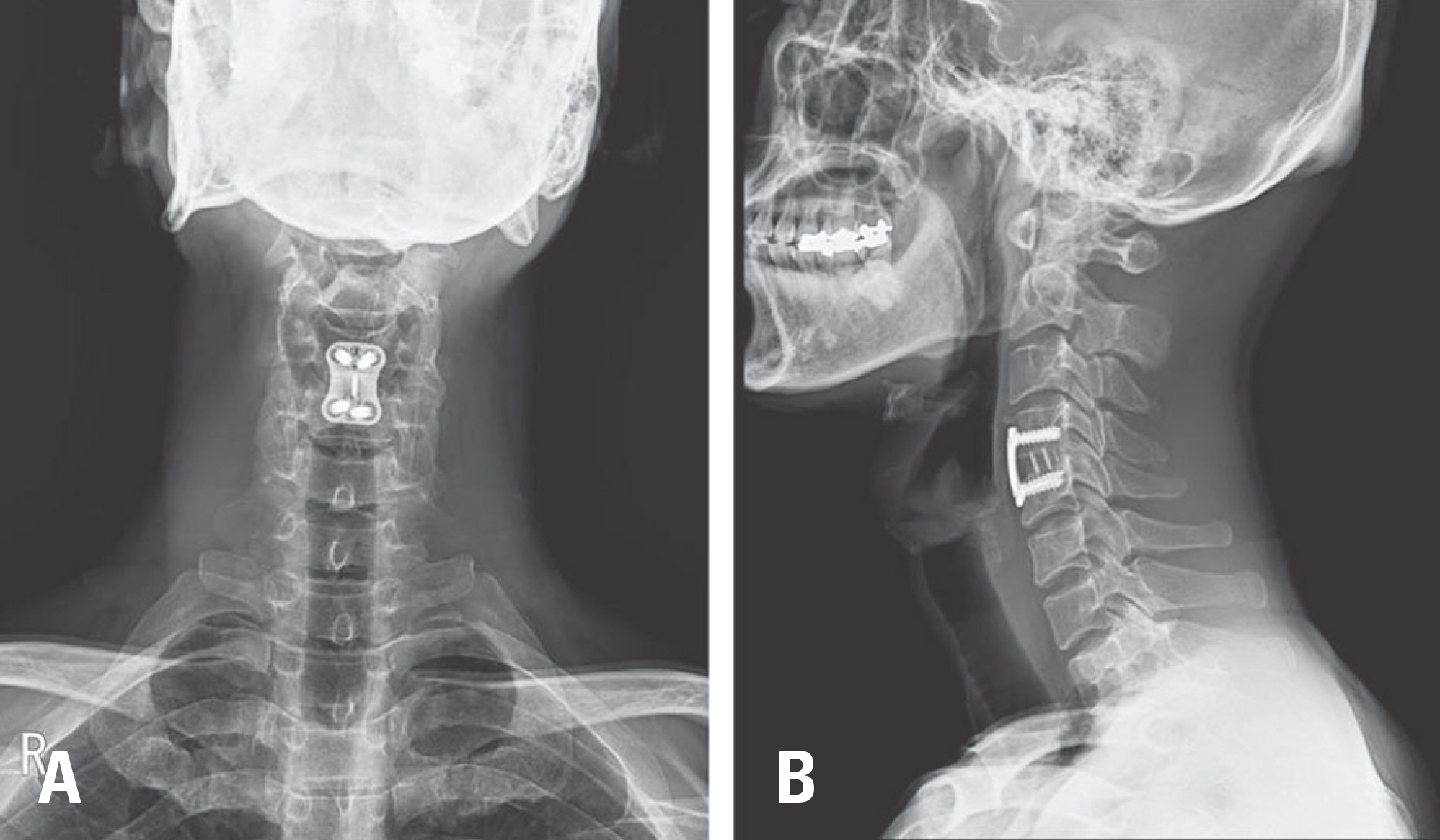
Clinical Efficacy of Cages in Anterior Cervical Fusion for Degenerative Cervical Disease
- Affiliations
-
- 1Department of Orthopedic Surgery, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea. amhangpark@gmail.com
- 2Department of Orthopedic Surgery, College of Medicine, Kyungpook National University, Kyungpook, Korea.
- 3Department of Orthopedic Surgery, Catholic University Hospital, Daegu, Korea.
- 4Department of Orthopedic Surgery, Catholic University College of Medicine, Seoul, Korea.
- 5Department of Orthopaedic Surgery, Inje University College of Medicine, Buson, Korea.
- 6Department of Orthopaedic Surgery, Chonbuk National University, Chonbuk, Korea.
- KMID: 2467947
- DOI: http://doi.org/10.4184/jkss.2019.26.4.172
Abstract
- STUDY DESIGN: Review of the literature.
OBJECTIVES
To present up-to-date information on the use of cages in anterior cervical fusion for degenerative cervical disease. SUMMARY OF LITERATURE REVIEW: The use of cages in anterior cervical fusion for degenerative cervical disease remains controversial.
MATERIALS AND METHODS
Review of the relevant literature.
RESULTS
The use of cages in anterior cervical fusion of one and multiple disc levels was effective in terms of biomechanical stability and clinical outcomes without complications at the donor site compared with use of an autograft. However, the use of only a cage had many drawbacks, so the combined use of a cage and a cervical plate is recommended.
CONCLUSIONS
The use of cages in anterior cervical fusion was effective in terms of clinical outcomes, and the combined use of a cage and a cervical plate is recommended.
Keyword
Figure
Reference
-
1. Sasso RC, LeHuec JC, Shaffrey C, Spine Interbody Research G. Iliac crest bone graft donor site pain after anterior lumbar interbody fusion: a prospective patient satisfaction outcome assessment. J Spinal Disord Tech. 2005; 18(Suppl):S77–81.2. Silber JS, Anderson DG, Daffner SD, et al. Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976). 2003; 28-2:134–9. DOI: 10.1097/01.BRS.0000041587.55176.67.
Article3. Song KJ, Lee KB. A preliminary study of the use of cage and plating for single-segment fusion in degenerative cervical spine disease. J Clin Neurosci. 2006; 13-2:181–7. DOI: S0967-5868(05)00412-1[pii],10.1016/j.jocn.2005.02.018.
Article4. Kurz LT, Garfin SR, Booth RE Jr. Iliac bone grafting: techniques and complications of harvesting. Garfin SR, editor. ed.Complications of spine surgery. Baltimore: Williams and Wilkins;1989. p. 323–41.5. Kim SH, Lee JK, Jang JW, et al. Polyetheretherketone Cage with Demineralized Bone Matrix Can Replace Iliac Crest Autografts for Anterior Cervical Discectomy and Fusion in Subaxial Cervical Spine Injuries. J Korean Neurosurg Soc. 2017; 60(2):211–9. DOI: 10.3340/jkns.2015.0203.014.
Article6. Vanek P, Bradac O, DeLacy P, et al. Comparison of 3 fusion techniques in the treatment of the degenerative cervical spine disease. Is standalone autograft really the “gold stan-dard?”: prospective study with 2-year follow-up. Spine (Phila Pa 1976). 2012; 37(19):1645–51. DOI: 10.1097/BRS.0b013e31825413fe.7. Celik SE, Kara A, Celik S. A comparison of changes over time in cervical foraminal height after tricortical iliac graft or polyetheretherketone cage placement following anterior discectomy. J Neurosurg Spine. 2007; 6-1:10–6. DOI: 10.3171/spi.2007.6.1.3.8. Bartels RH, Donk R, van Azn RD. Height of cervical foramina after anterior discectomy and implantation of a car-bon fiber cage. J Neurosurg. 2001; 95-1(Suppl):40–2.
Article9. Sekerci Z, Ugur A, Ergun R, et al. Early changes in the cervical foraminal area after anterior interbody fusion with polyetheretherketone (PEEK) cage containing synthetic bone particulate: a prospective study of 20 cases. Neurol Res. 2006; 28(5):568–71. DOI: 10.1179/016164106X110382.10. Dufour T, Huppert J, Louis C, et al. Radiological analysis of 37 segments in cervical spine implanted with a peek standalone device, with at least one year follow-up. Br J Neurosurg. 2010; 24(6):633–40. DOI: 10.3109/02688691003793029.
Article11. Lind BI, Zoega B, Rosen H. Autograft versus interbody fusion cage without plate fixation in the cervical spine: a randomized clinical study using radiostereometry. Eur Spine J. 2007; 16(8):1251–6. DOI: 10.1007/s00586-007-0337-7.
Article12. Feng SW, Chang MC, Chou PH, et al. Implantation of an empty polyetheretherketone cage in anterior cervical discectomy and fusion: a prospective randomised controlled study with 2 years follow-up. Eur Spine J. 2018; 27(6):1358–64. DOI: 10.1007/s00586-017-5450-7.13. Lee CH, Hyun SJ, Kim MJ, et al. Comparative analysis of 3 different construct systems for single-level anterior cervical discectomy and fusion: standalone cage, iliac graft plus plate augmentation, and cage plus plating. J Spinal Disord Tech. 2013; 26(2):112–8. DOI: 10.1097/BSD.0b013e318274148e.14. Fujibayashi S, Neo M, Nakamura T. Stand-alone interbody cage versus anterior cervical plate for treatment of cervical disc herniation: sequential changes in cage subsidence. J Clin Neurosci. 2008; 15-9:1017–22. DOI: 10.1016/j.jocn.2007.05.011.
Article15. Oliver JD, Goncalves S, Kerezoudis P, et al. Comparison of Outcomes for Anterior Cervical Discectomy and Fusion with and without Anterior Plate Fixation: A Systematic Review and Meta-Analysis. Spine (Phila Pa 1976). 2018; 43(7):E413–E22. DOI: 10.1097/BRS.0000000000002441.16. 이동호, 염진섭, 장한. 경추 추간판 질환. 석세일. ed.척추외과학. 4th ed.서울: 최신의학사;2017. p. 258–9.17. Topuz K, Colak A, Kaya S, Simsek H, Kutlay M, Demircan MN, Velioglu M. Two-level contiguous cervical disc disease treated with peek cages packed with demineralized bone matrix: results of 3-year follow-up. Eur Spine J. 2009; 18(2):238–43. DOI: 10.1007/s00586-008-0869-5.
Article18. Lied B, Roenning PA, Sundseth J, et al. Anterior cervical discectomy with fusion in patients with cervical disc degeneration: a prospective outcome study of 258 patients (181 fused with autologous bone graft and 77 fused with a PEEK cage). BMC Surg. 2010; 10:10. DOI: 10.1186/1471-2482-10-10.
Article19. Jacobs W, Willems PC, Kruyt M, et al. Systematic review of anterior interbody fusion techniques for single- and double-level cervical degenerative disc disease. Spine (Phila Pa 1976). 2011; 36(14):E950–60. DOI: 10.1097/BRS.0b013e31821cbba5.
Article20. Burkhardt JK, Mannion AF, Marbacher S, et al. The influence of cervical plate fixation with either autologous bone or cage insertion on radiographic and patient-rated outcomes after two-level anterior cervical discectomy and fusion. Eur Spine J. 2015; 24-1:113–9. DOI: 10.1007/s00586-014-3456-y.
Article21. Song KJ, Yoon SJ, Lee KB. Three- and four-level anterior cervical discectomy and fusion with a PEEK cage and plate construct. Eur Spine J. 2012; 21(12):2492–7. DOI: 10.1007/s00586-012-2447-0.
Article22. Yang JJ, Yu CH, Chang BS, et al. Subsidence and non-union after anterior cervical interbody fusion using a standalone polyetheretherketone (PEEK) cage. Clin Orthop Surg. 2011; 3(1):16–23. DOI: 10.4055/cios.2011.3.1.16.
Article23. Ji GY, Oh CH, Shin DA, et al. Stand-alone Cervical Cages Versus Anterior Cervical Plates in 2-Level Cervical Anterior Interbody Fusion Patients: Analysis of Adjacent Segment Degeneration. J Spinal Disord Tech. 2015; 28(7):E433–8. DOI: 10.1097/BSD.0b013e3182a355ad.24. Oh JK, Kim TY, Lee HS, et al. Stand-alone cervical cages versus anterior cervical plate in 2-level cervical anterior interbody fusion patients: clinical outcomes and radiologic changes. J Spinal Disord Tech. 2013; 26(8):415–20. DOI: 10.1097/BSD.0b013e31824c7d22.25. Perrini P, Cagnazzo F, Benedetto N, et al. Cage with anterior plating is advantageous over the standalone cage for segmental lordosis in the treatment of two-level cervical degenerative spondylopathy: A retrospective study. Clin Neurol Neurosurg. 2017; 163:27–32. DOI: 10.1016/j.clineuro.2017.10.014.
Article26. Scholz M, Schleicher P, Pabst S, et al. A zero-profile an-chored spacer in multilevel cervical anterior interbody fusion: biomechanical comparison to established fixation techniques. Spine (Phila Pa 1976). 2015; 40(7):E375–80. DOI: 10.1097/BRS.0000000000000768.27. Chang WC, Tsou HK, Kao TH, et al. Successful treatment of extended epidural abscess and long segment os-teomyelitis: a case report and review of the literature. Surg Neurol. 2008; 69(2):117–20. discussion 20. DOI: 10.1016/j.surneu.2006.12.047.
Article28. Patel AR, Alton TB, Bransford RJ, et al. Spinal epidural abscesses: risk factors, medical versus surgical management, a retrospective review of 128 cases. Spine J. 2014; 14(2):32630. DOI: 10.1016/j.spinee.2013.10.046.
Article29. Song KJ, Choi BW, Kim GH, et al. Usefulness of polyetheretherketone (PEEK) cage with plate augmentation for anterior arthrodesis in traumatic cervical spine injury. Spine J. 2010; 10(1):50–7. DOI: S1529-9430 (09)00846-8 [pii], 10.1016/j.spinee.2009.08.458.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analysis of Noninstrumented Anterior Cervical Discectomy and Interbody Fusion in Degenerative Cervical Disease
- The Efficacy of the Unicortical Screw in the Anterior Cervical Fusion of the Degenerative Cervical Spine Disease
- Clinical Experience with Double Cylindrical Cages for Anterior Cervical Interbody Fusion
- Anterior Cervical Interbody Fusion with the Carbon Composite Osta-Pek Frame Cage in Degenerative Cervical Diseases
- Results of Four-Level Anterior Cervical Discectomy and Fusion Using Stand-Alone Interbody Titanium Cages