J Clin Neurol.
2019 Apr;15(2):221-227. 10.3988/jcn.2019.15.2.221.
Acquired Ocular Motor Nerve Palsy in Neurology Clinics: A Prospective Multicenter Study
- Affiliations
-
- 1Department of Neurology, Pusan National University Hospital, Pusan National University School of Medicine and Biomedical Research Institute, Busan, Korea.
- 2Department of Neurology, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, Korea. jisookim@snu.ac.kr
- 3Department of Neurology, Pusan National University Yangsan Hospital, Pusan National University School of Medicine and Biomedical Research Institute, Yangsan, Korea.
- 4Department of Neurology, Chonbuk National University School of Medicine, Jeonju, Korea.
- 5Department of Neurology, Kyungpook National University School of Medicine, Daegu, Korea.
- 6Department of Neurology, Wonkwang University School of Medicine, Institute of Wonkwang Medical Science and Regional Cardiocerebrovascular Center, Iksan, Korea.
- 7Department of Neurology, Chonnam National University Medical School, Chonnam National University Hospital, Gwangju, Korea.
- 8Department of Neurology, Chungnam National University School of Medicine, Daejeon, Korea.
- 9Research Administration Team, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 2467736
- DOI: http://doi.org/10.3988/jcn.2019.15.2.221
Abstract
- BACKGROUND AND PURPOSE
This study aimed to determine the patterns and etiologies of acquired ocular motor nerve palsy (OMNP) diagnosed in neurology clinics. We also investigated the clinical features that may predict the causes other than microvascular ischemia in isolated OMNP.
METHODS
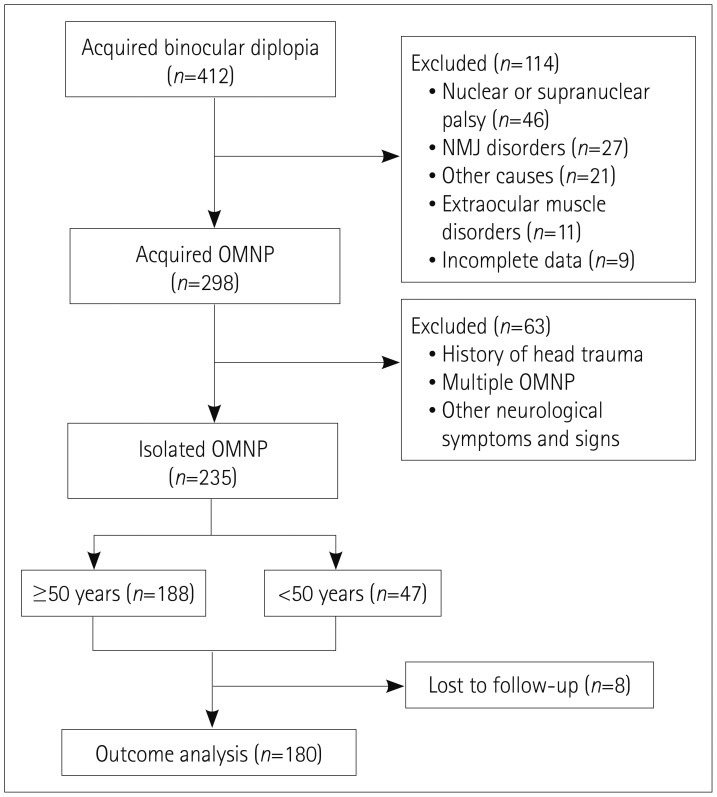
We performed a prospective multicenter study that had recruited 298 patients with acquired OMNP from the neurology clinics of referral-based 9 university hospitals in Korea. We finally selected 235 patients with isolated OMNP and divided them into older (age ≥50 years, n=188) and younger (age <50 years, n=47) groups. We investigated the underlying etiologies of acquired OMNP. We also estimated the frequency of microvascular ischemia and other causes in isolated OMNP, and sought to determine the clinical features that can predict the causes other than microvascular ischemia.
RESULTS
Abducens nerve palsy was the most common (40%) of the acquired OMNPs, followed by oculomotor nerve palsy (27%), trochlear nerve palsy (23%), and multiple OMNPs (10%). The etiologies included microvascular ischemia (47%), inflammatory (21%), stroke (5%), trauma (5%), neoplasm (3%), and others (2%), with the cause not being determined in 13% of the patients. Microvascular ischemia was the most common cause (83%) in patients aged ≥50 years with isolated OMNP, followed by inflammation (6%), stroke (6%), neoplasm (3%), and aneurysm (1%). Microvascular ischemia was more common in the older than the younger group (83% vs. 49%, p<0.001). The intensity of headache was the only risk factor for causes other than microvascular ischemia in isolated OMNP.
CONCLUSIONS
Vascular and inflammatory disorders are the most common causes of acquired OMNP diagnosed in neurology clinics. Microvascular ischemia was the predominant cause of isolated OMNP. Severe headache indicates causes other than microvascular ischemia in isolated OMNP.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Isolated abducens nerve palsy due to internal carotid artery aneurysm
Byung Joon Kim, Kang Min Park
Ann Clin Neurophysiol. 2020;22(1):46-47. doi: 10.14253/acn.2020.22.1.46.
Reference
-
2. Danchaivijitr C, Kennard C. Diplopia and eye movement disorders. J Neurol Neurosurg Psychiatry. 2004; 75(Suppl 4):iv24–iv31. PMID: 15564429.
Article3. Buracchio T, Rucker JC. Pearls and oy-sters of localization in ophthalmoparesis. Neurology. 2007; 69:E35–E40. PMID: 18071135.
Article4. Prasad S, Volpe NJ. Paralytic strabismus: third, fourth, and sixth nerve palsy. Neurol Clin. 2010; 28:803–833. PMID: 20638001.
Article5. Keane JR. Fourth nerve palsy: historical review and study of 215 inpatients. Neurology. 1993; 43:2439–2443. PMID: 8255437.
Article6. Jacobson DM. Pupil involvement in patients with diabetes-associated oculomotor nerve palsy. Arch Ophthalmol. 1998; 116:723–727. PMID: 9639439.
Article7. Jacobson DM. Relative pupil-sparing third nerve palsy: etiology and clinical variables predictive of a mass. Neurology. 2001; 56:797–798. PMID: 11274322.
Article8. Lee SH, Lee SS, Park KY, Han SH. Isolated oculomotor nerve palsy: diagnostic approach using the degree of external and internal dysfunction. Clin Neurol Neurosurg. 2002; 104:136–141. PMID: 11932044.
Article9. Richards BW, Jones FR Jr, Younge BR. Causes and prognosis in 4,278 cases of paralysis of the oculomotor, trochlear, and abducens cranial nerves. Am J Ophthalmol. 1992; 113:489–496. PMID: 1575221.
Article10. Rucker CW. Paralysis of the third, fourth and sixth cranial nerves. Am J Ophthalmol. 1958; 46:787–794. PMID: 13606195.
Article11. Rucker CW. The causes of paralysis of the third, fourth and sixth cranial nerves. Am J Ophthalmol. 1966; 61:1293–1298. PMID: 5938012.
Article12. Rush JA, Younge BR. Paralysis of cranial nerves III, IV, and VI. Cause and prognosis in 1,000 cases. Arch Ophthalmol. 1981; 99:76–79. PMID: 7458744.13. Tiffin PA, MacEwen CJ, Craig EA, Clayton G. Acquired palsy of the oculomotor, trochlear and abducens nerves. Eye (Lond). 1996; 10:377–384. PMID: 8796166.
Article14. Berlit P. Isolated and combined pareses of cranial nerves III, IV and VI. A retrospective study of 412 patients. J Neurol Sci. 1991; 103:10–15. PMID: 1865222.
Article15. Peters GB 3rd, Bakri SJ, Krohel GB. Cause and prognosis of nontraumatic sixth nerve palsies in young adults. Ophthalmology. 2002; 109:1925–1928. PMID: 12359616.
Article16. Moster ML, Savino PJ, Sergott RC, Bosley TM, Schatz NJ. Isolated sixth-nerve palsies in younger adults. Arch Ophthalmol. 1984; 102:1328–1330. PMID: 6477251.
Article17. Park UC, Kim SJ, Hwang JM, Yu YS. Clinical features and natural history of acquired third, fourth, and sixth cranial nerve palsy. Eye (Lond). 2008; 22:691–696. PMID: 17293794.
Article18. Bendszus M, Beck A, Koltzenburg M, Vince GH, Brechtelsbauer D, Littan T, et al. MRI in isolated sixth nerve palsies. Neuroradiology. 2001; 43:742–745. PMID: 11594423.
Article19. Chou KL, Galetta SL, Liu GT, Volpe NJ, Bennett JL, Asbury AK, et al. Acute ocular motor mononeuropathies: prospective study of the roles of neuroimaging and clinical assessment. J Neurol Sci. 2004; 219:35–39. PMID: 15050435.
Article20. Murchison AP, Gilbert ME, Savino PJ. Neuroimaging and acute ocular motor mononeuropathies: a prospective study. Arch Ophthalmol. 2011; 129:301–305. PMID: 21402985.21. Tamhankar MA, Biousse V, Ying GS, Prasad S, Subramanian PS, Lee MS, et al. Isolated third, fourth, and sixth cranial nerve palsies from presumed microvascular versus other causes: a prospective study. Ophthalmology. 2013; 120:2264–2269. PMID: 23747163.22. Mollan SP, Edwards JH, Price A, Abbott J, Burdon MA. Aetiology and outcomes of adult superior oblique palsies: a modern series. Eye (Lond). 2009; 23:640–644. PMID: 18327160.
Article23. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018; 38:1–211.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Clinical Study of Diplopia Due to Neurologic Disorder
- Ocular Abduction Palsy in a Patient with Herpes ZosterOphthalmicus and This was Improved by Short-term Use of Steroid
- Eight-And-a-Half Syndrome in Pontine Infarction
- Clinical Features and Natural History of the Acquired Third, Fourth, and Sixth Cranial Nerve Palsy
- Clinical Study of Motor Paresis in In-patients with Herpes Zoster