J Korean Assoc Oral Maxillofac Surg.
2018 Dec;44(6):275-281. 10.5125/jkaoms.2018.44.6.275.
A working paradigm for managing mandibular fractures under regional anesthesia
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Government Dental College and Hospital, Mumbai, India. natarajan.balaji.c@gmail.com
- 2Private Practitioner, Bengaluru, India.
- KMID: 2467174
- DOI: http://doi.org/10.5125/jkaoms.2018.44.6.275
Abstract
OBJECTIVES
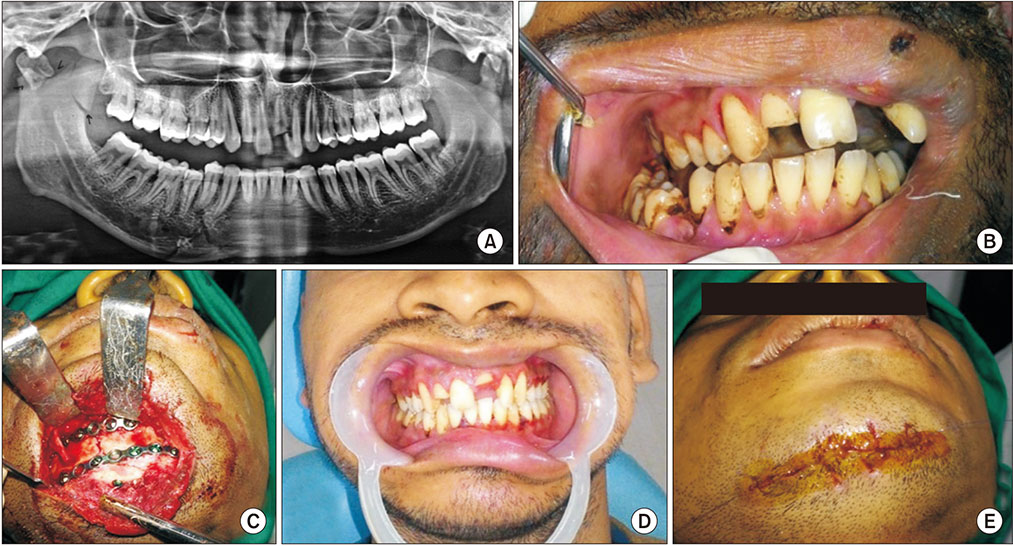
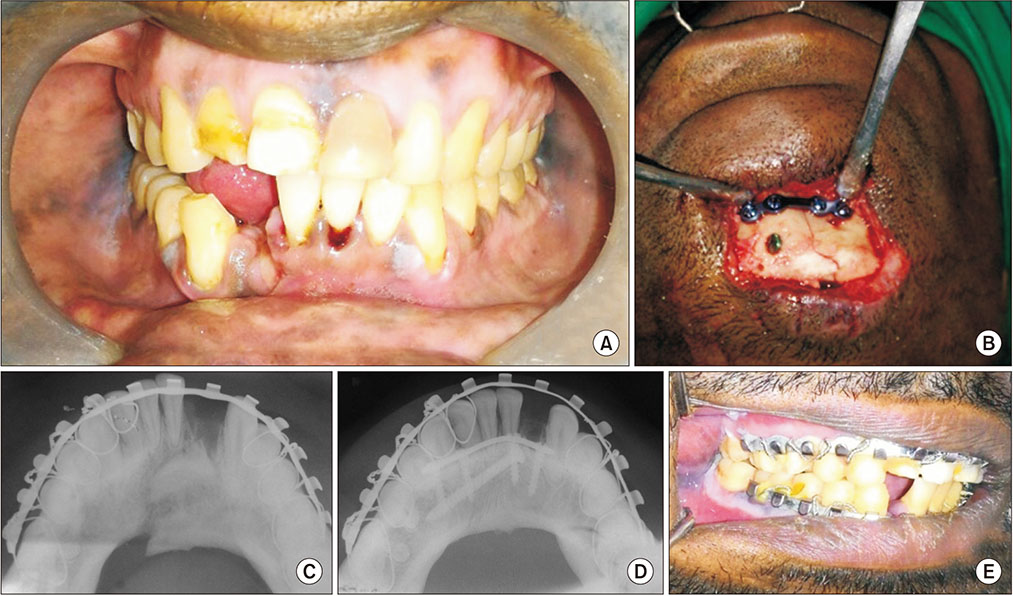
Isolated mandibular fractures contribute to approximately 45% of maxillofacial traumas. Improper management of mandibular fractures can cause myriad potential complications and can lead to serious functional and aesthetic sequelae. The objective of the study is to design a stepwise approach for managing isolated mandibular fractures using open reduction and internal fixation (ORIF) with regional anesthesia on outpatient basis.
MATERIALS AND METHODS
Patients with isolated mandibular fractures presenting to the department of maxillofacial surgery were selected for ORIF under regional anesthesia based on occlusion, age, socioeconomic status, general condition, habits, and allied medical ailments. Standard preoperative, intraoperative, and postoperative protocols were followed. All patients were followed up for a minimum of 4 weeks up to a maximum of 1 year.
RESULTS
Of 23 patients who received regional anesthesia, all but one had good postoperative functional occlusion. One patient was hypersensitive and had difficulty tolerating the procedure. Two patients developed an extraoral draining sinus, one of whom was managed with local curettage, while the other required hardware removal. One patient, who was a chronic alcoholic, returned 1 week after treatment with deranged fracture segments after he fell while intoxicated.
CONCLUSION
With proper case selection following a stepwise protocol, the majority of mandibular fractures requiring ORIF can be managed with regional anesthesia and yield minimal to no complications.
Keyword
MeSH Terms
Figure
Reference
-
1. Gajiwala KJ. Surgery of temporomandibular joint under local anaesthesia. Indian J Plast Surg. 2008; 41:175–182.
Article2. Manodh P, Prabhu Shankar D, Pradeep D, Santhosh R, Murugan A. Incidence and patterns of maxillofacial trauma-a retrospective analysis of 3611 patients-an update. Oral Maxillofac Surg. 2016; 20:377–383.
Article3. Ellis E 3rd, Moos KF, El-Attar A. Ten years of mandibular fractures: an analysis of 2,137 cases. Oral Surg Oral Med Oral Pathol. 1985; 59:120–129.
Article4. Zweig BE. Complications of mandibular fractures. Atlas Oral Maxillofac Surg Clin North Am. 2009; 17:93–101.
Article5. Champy M, Loddé JP, Schmitt R, Jaeger JH, Muster D. Mandibular osteosynthesis by miniature screwed plates via a buccal approach. J Maxillofac Surg. 1978; 6:14–21.
Article6. Ellis E 3rd, Walker LR. Treatment of mandibular angle fractures using one noncompression miniplate. J Oral Maxillofac Surg. 1996; 54:864–871. discussion 871-2.
Article7. Kumaran PS, Thambiah L. Versatility of a single upper border miniplate to treat mandibular angle fractures: a clinical study. Ann Maxillofac Surg. 2011; 1:160–165.
Article8. Ellis E 3rd. Open reduction and internal fixation of combined angle and body/symphysis fractures of the mandible: how much fixation is enough? J Oral Maxillofac Surg. 2013; 71:726–733.
Article9. Khalil H. A basic review on the inferior alveolar nerve block techniques. Anesth Essays Res. 2014; 8:3–8.
Article10. Heard AM, Green RJ, Lacquiere DA, Sillifant P. The use of mandibular nerve block to predict safe anaesthetic induction in patients with acute trismus. Anaesthesia. 2009; 64:1196–1198.
Article11. Woodall NM, Harwood RJ, Barker GL. Complications of awake fibreoptic intubation without sedation in 200 healthy anaesthetists attending a training course. Br J Anaesth. 2008; 100:850–855.
Article12. Singh B, Bhardwaj V. Continuous mandibular nerve block for pain relief. A report of two cases. Can J Anaesth. 2002; 49:951–953.
Article13. El-Anwar MW, Hegab A. Internal fixation of single mandibular fracture under mandibular nerve block. Oral Maxillofac Surg. 2016; 20:57–61.
Article14. Politi M, Toro C, Costa F, Polini F, Robiony M. Intraoperative awakening of the patient during orthognathic surgery: a method to prevent the condylar sag. J Oral Maxillofac Surg. 2007; 65:109–114.
Article15. Ellis E 3rd. Treatment methods for fractures of the mandibular angle. Int J Oral Maxillofac Surg. 1999; 28:243–252.
Article16. Elledge RO, Elledge R, Aquilina P, Hodson J, Dover S. The role of alcohol in maxillofacial trauma: a comparative retrospective audit between the two centers. Alcohol. 2011; 45:239–243.
Article17. Falender LG, Leban SG, Williams FA. Postoperative nutritional support in oral and maxillofacial surgery. J Oral Maxillofac Surg. 1987; 45:324–330.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Airway management in a displaced comminuted fracture of the mandible and atlas with a vertebral artery injury: A case report
- The role of mandibular third molar in the mandibular angle fractures
- The influence of mandibular third molar on mandibular angle fracture
- Treatment of Mandibular Angle Fractures
- Open Reduction and Rigid Internal Fixation of Mandibular Fractures