Korean J Radiol.
2020 Jan;21(1):25-32. 10.3348/kjr.2019.0275.
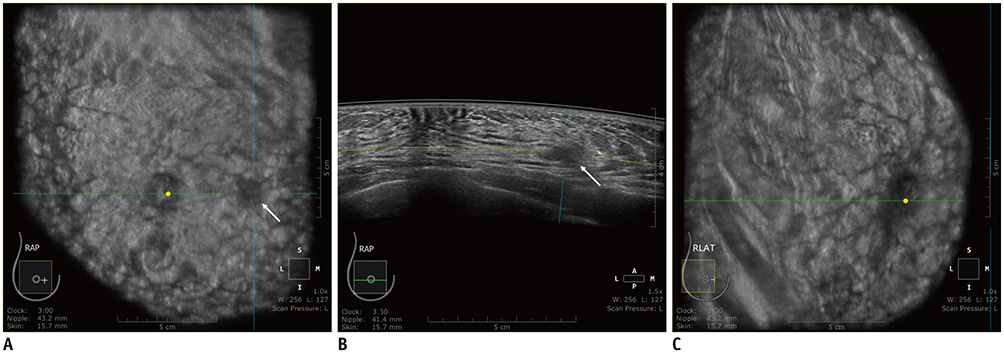
Automated Breast Ultrasound System for Breast Cancer Evaluation: Diagnostic Performance of the Two-View Scan Technique in Women with Small Breasts
- Affiliations
-
- 1Department of Radiology, Seoul National University College of Medicine, Seoul National University Hospital, Seoul, Korea. imchangjm@gmail.com
- 2Department of Radiology, Seoul National University Hospital Healthcare System Gangnam Center, Seoul, Korea.
- KMID: 2467039
- DOI: http://doi.org/10.3348/kjr.2019.0275
Abstract
OBJECTIVE
To comparatively evaluate the scan coverage and diagnostic performance of the two-view scan technique (2-VST) of the automated breast ultrasound system (ABUS) versus the conventional three-view scan technique (3-VST) in women with small breasts.
MATERIALS AND METHODS
Between March 2016 and May 2017, 136 asymptomatic women with small breasts (bra cup size A) suitable for 2-VST were enrolled. Subsequently, 272 breasts were subjected to bilateral whole-breast ultrasound examinations using ABUS and the hand-held ultrasound system (HHUS). During ABUS image acquisition, one breast was scanned with 2-VST, while the other breast was scanned with 3-VST. In each breast, the breast coverage and visibility of the HHUS detected lesions on ABUS were assessed. The sensitivity and specificity of ABUS were compared between 2-VST and 3-VST.
RESULTS
Among 136 breasts, eight cases of breast cancer were detected by 2-VST, and 10 cases of breast cancer were detected by 3-VST. The breast coverage was satisfactory in 94.1% and 91.9% of cases under 2-VST and 3-VST, respectively (p = 0.318). All HHUS-detected lesions were visible on the ABUS images regardless of the scan technique. The sensitivities and specificities were similar between 2-VST and 3-VST (100% [8/8] vs. 100% [10/10], and 97.7% [125/128] vs. 95.2% [120/126], respectively), with no significant difference (p > 0.05).
CONCLUSION
2-VST of ABUS achieved comparable scan coverage and diagnostic performance to that of conventional 3-VST in women with small breasts.
Keyword
Figure
Reference
-
1. Berg WA, Blume JD, Cormack JB, Mendelson EB, Lehrer D, Böhm-Vélez M, et al. ACRIN 6666 Investigators. Combined screening with ultrasound and mammography vs mammography alone in women at elevated risk of breast cancer. JAMA. 2008; 299:2151–2163.
Article2. Ohuchi N, Suzuki A, Sobue T, Kawai M, Yamamoto S, Zheng YF, et al. J-START investigator groups. Sensitivity and specificity of mammography and adjunctive ultrasonography to screen for breast cancer in the Japan Strategic Anti-cancer Randomized Trial (J-START): a randomised controlled trial. Lancet. 2016; 387:341–348.
Article3. Shen S, Zhou Y, Xu Y, Zhang B, Duan X, Huang R, et al. A multi-centre randomised trial comparing ultrasound vs mammography for screening breast cancer in high-risk Chinese women. Br J Cancer. 2015; 112:998–1004.
Article4. Berg WA, Blume JD, Cormack JB, Mendelson EB. Operator dependence of physician-performed whole-breast US: lesion detection and characterization. Radiology. 2006; 241:355–365.
Article5. van Zelst JCM, Mann RM. Automated three-dimensional breast US for screening: technique, artifacts, and lesion characterization. Radiographics. 2018; 38:663–683.
Article6. Brem RF, Tabár L, Duffy SW, Inciardi MF, Guingrich JA, Hashimoto BE, et al. Assessing improvement in detection of breast cancer with three-dimensional automated breast US in women with dense breast tissue: the SomoInsight Study. Radiology. 2015; 274:663–673.
Article7. Choi WJ, Cha JH, Kim HH, Shin HJ, Kim H, Chae EY, et al. Comparison of automated breast volume scanning and hand-held ultrasound in the detection of breast cancer: an analysis of 5,566 patient evaluations. Asian Pac J Cancer Prev. 2014; 15:9101–9105.
Article8. Giuliano V, Giuliano C. Improved breast cancer detection in asymptomatic women using 3D-automated breast ultrasound in mammographically dense breasts. Clin Imaging. 2013; 37:480–486.
Article9. Vourtsis A, Kachulis A. The performance of 3D ABUS versus HHUS in the visualisation and BI-RADS characterisation of breast lesions in a large cohort of 1,886 women. Eur Radiol. 2018; 28:592–601.
Article10. Wilczek B, Wilczek HE, Rasouliyan L, Leifland K. Adding 3D automated breast ultrasound to mammography screening in women with heterogeneously and extremely dense breasts: report from a hospital-based, high-volume, single-center breast cancer screening program. Eur J Radiol. 2016; 85:1554–1563.
Article11. Tozaki M, Isobe S, Yamaguchi M, Ogawa Y, Kohara M, Joo C, et al. Optimal scanning technique to cover the whole breast using an automated breast volume scanner. Jpn J Radiol. 2010; 28:325–328.
Article12. Rella R, Belli P, Giuliani M, Bufi E, Carlino G, Rinaldi P, et al. Automated breast ultrasonography (ABUS) in the screening and diagnostic setting: indications and practical use. Acad Radiol. 2018; 25:1457–1470.13. Wojcinski S, Farrokh A, Hille U, Wiskirchen J, Gyapong S, Soliman AA, et al. The automated breast volume scanner (ABVS): initial experiences in lesion detection compared with conventional handheld B-mode ultrasound: a pilot study of 50 cases. Int J Womens Health. 2011; 3:337–346.
Article14. Wojcinski S, Gyapong S, Farrokh A, Soergel P, Hillemanns P, Degenhardt F. Diagnostic performance and inter-observer concordance in lesion detection with the automated breast volume scanner (ABVS). BMC Med Imaging. 2013; 13:36.
Article15. Chen L, Chen Y, Diao XH, Fang L, Pang Y, Cheng AQ, et al. Comparative study of automated breast 3-D ultrasound and handheld B-mode ultrasound for differentiation of benign and malignant breast masses. Ultrasound Med Biol. 2013; 39:1735–1742.
Article16. Golatta M, Baggs C, Schweitzer-Martin M, Domschke C, Schott S, Harcos A, et al. Evaluation of an automated breast 3D-ultrasound system by comparing it with hand-held ultrasound (HHUS) and mammography. Arch Gynecol Obstet. 2015; 291:889–895.
Article17. Golatta M, Franz D, Harcos A, Junkermann H, Rauch G, Scharf A, et al. Interobserver reliability of automated breast volume scanner (ABVS) interpretation and agreement of ABVS findings with hand held breast ultrasound (HHUS), mammography and pathology results. Eur J Radiol. 2013; 82:e332–e336.
Article18. Schmachtenberg C, Fischer T, Hamm B, Bick U. Diagnostic performance of automated breast volume scanning (ABVS) compared to handheld ultrasonography with breast MRI as the gold standard. Acad Radiol. 2017; 24:954–961.
Article19. An YY, Kim SH, Kang BJ. The image quality and lesion characterization of breast using automated whole-breast ultrasound: a comparison with handheld ultrasound. Eur J Radiol. 2015; 84:1232–1235.
Article20. Kotsianos-Hermle D, Hiltawsky KM, Wirth S, Fischer T, Friese K, Reiser M. Analysis of 107 breast lesions with automated 3D ultrasound and comparison with mammography and manual ultrasound. Eur J Radiol. 2009; 71:109–115.
Article21. Lin X, Wang J, Han F, Fu J, Li A. Analysis of eighty-one cases with breast lesions using automated breast volume scanner and comparison with handheld ultrasound. Eur J Radiol. 2012; 81:873–878.
Article22. Van Zelst JC, Platel B, Karssemeijer N, Mann RM. Multiplanar reconstructions of 3D automated breast ultrasound improve lesion differentiation by radiologists. Acad Radiol. 2015; 22:1489–1496.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Technical Note on a Novel Technique for the Evaluation of Breast Excision Specimen: Automated Breast Ultrasound System
- Clinical Application of Automated Breast Ultrasound
- Automated Breast Ultrasound Screening for Dense Breasts
- Clinical Applications of Automated Breast Ultrasound: Screening for Breast Cancer
- Utility and Diagnostic Performance of Automated Breast Ultrasound System in Evaluating Pure Non-Mass Enhancement on Breast Magnetic Resonance Imaging