Dement Neurocogn Disord.
2019 Dec;18(4):138-148. 10.12779/dnd.2019.18.4.138.
A Comparison Study of Cilostazol and Aspirin on Changes in Volume of Cerebral Small Vessel Disease White Matter Changes: Protocol of a Multicenter, Randomized Controlled Trial
- Affiliations
-
- 1Department of Neurology, Myongji Hospital, Hanyang University College of Medicine, Goyang, Korea.
- 2Department of Neurology, Chonnam National University Medical School, Gwangju, Korea.
- 3Department of Neurology, College of Medicine, Chung-Ang University, Seoul, Korea.
- 4Department of Neurology, Ewha Womans University School of Medicine, Seoul, Korea.
- 5Department of Neurology, National Health Insurance Service Ilsan Hospital, Goyang, Korea.
- 6Department of Neurology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 7Department of Neurology, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea.
- 8Department of Neurology, Dong-A University College of Medicine, Busan, Korea.
- 9Department of Neurology, Pusan National University Hospital, Pusan National University School of Medicine and Medical Research Institute, Busan, Korea.
- 10Department of Neurology, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea.
- 11Department of Neurology, The Catholic University of Korea Eunpyeong St. Mary's Hospital, Bucheon, Korea.
- 12Department of Neurology, Wonkwang University School of Medicine, Iksan, Korea.
- 13Department of Neurology, Konyang University College of Medicine, Daejeon, Korea.
- 14Department of Neurology, Eulji University Hospital, Eulji University School of Medicine, Daejeon, Korea.
- 15Department of Neurology, Hallym University Dongtan Sacred Heart Hospital, Hallym University College of Medicine, Hwaseong, Korea.
- 16Department of Neurology, Kyung Hee University School of Medicine, Seoul, Korea.
- 17Department of Neurology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 18Department of Anatomy and Neurology, Ajou University School of Medicine, Suwon, Korea.
- 19Department of Biomedical Engineering, Hanyang University, Seoul, Korea.
- 20Department of Neurology, Inha University School of Medicine, Incheon, Korea. seonghye@inha.ac.kr
- KMID: 2466757
- DOI: http://doi.org/10.12779/dnd.2019.18.4.138
Abstract
- BACKGROUND AND PURPOSE
Cerebral small vessel disease (CSVD) is the most common cause of vascular dementia and a major contributor to mixed dementia. CSVD is characterized by progressive cerebral white matter changes (WMC) due to chronic low perfusion and loss of autoregulation. In addition to its antiplatelet effect, cilostazol exerts a vasodilating effect and improves endothelial function. This study aims to compare the effects of cilostazol and aspirin on changes in WMC volume in CSVD.
METHODS
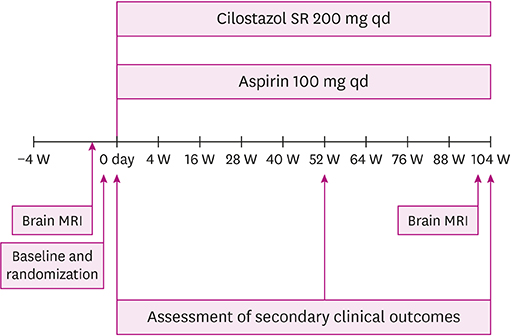
The comparison study of Cilostazol and aspirin on cHAnges in volume of cerebral smaLL vEssel disease white matter chaNGEs (CHALLENGE) is a double blind, randomized trial involving 19 hospitals across South Korea. Patients with moderate or severe WMC and ≥ 1 lacunar infarction detected on brain magnetic resonance imaging (MRI) are eligible; the projected sample size is 254. Participants are randomly assigned to a cilostazol or aspirin group at a 1:1 ratio. Cilostazol slow release 200 mg or aspirin 100 mg are taken once daily for 2 years. The primary outcome measure is the change in WMC volume on MRI from baseline to 104 weeks. Secondary imaging outcomes include changes in the number of lacunes and cerebral microbleeds, fractional anisotropy and mean diffusivity on diffusion tensor imaging, and brain atrophy. Secondary clinical outcomes include all ischemic strokes, all vascular events, and changes in cognition, motor function, mood, urinary symptoms, and disability.
CONCLUSIONS
CHALLENGE will provide evidence to support the selection of long-term antiplatelet therapy in CSVD. TRIAL REGISTRATION: ClinicalTrials.gov Identifier: NCT01932203
MeSH Terms
Figure
Reference
-
1. Debette S, Markus HS. The clinical importance of white matter hyperintensities on brain magnetic resonance imaging: systematic review and meta-analysis. BMJ. 2010; 341:c3666.
Article2. Vermeer SE, Longstreth WT Jr, Koudstaal PJ. Silent brain infarcts: a systematic review. Lancet Neurol. 2007; 6:611–619.
Article3. Rensma SP, van Sloten TT, Launer LJ, Stehouwer CD. Cerebral small vessel disease and risk of incident stroke, dementia and depression, and all-cause mortality: A systematic review and meta-analysis. Neurosci Biobehav Rev. 2018; 90:164–173.
Article4. van Agtmaal MJ, Houben AJ, Pouwer F, Stehouwer CD, Schram MT. Association of microvascular dysfunction with late-life depression: a systematic review and meta-analysis. JAMA Psychiatry. 2017; 74:729–739.
Article5. Cannistraro RJ, Badi M, Eidelman BH, Dickson DW, Middlebrooks EH, Meschia JF. CNS small vessel disease: a clinical review. Neurology. 2019; 92:1146–1156.6. Kim YJ, Kwon HK, Lee JM, Cho H, Kim HJ, Park HK, et al. Gray and white matter changes linking cerebral small vessel disease to gait disturbances. Neurology. 2016; 86:1199–1207.
Article7. van der Holst HM, van Uden IW, Tuladhar AM, de Laat KF, van Norden AG, Norris DG, et al. Cerebral small vessel disease and incident parkinsonism: The RUN DMC study. Neurology. 2015; 85:1569–1577.
Article8. Nam KW, Kwon HM, Lim JS, Han MK, Nam H, Lee YS. The presence and severity of cerebral small vessel disease increases the frequency of stroke in a cohort of patients with large artery occlusive disease. PLoS One. 2017; 12:e0184944.
Article9. Pantoni L. Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol. 2010; 9:689–701.
Article10. Wardlaw JM, Smith C, Dichgans M. Mechanisms of sporadic cerebral small vessel disease: insights from neuroimaging. Lancet Neurol. 2013; 12:483–497.
Article11. van Leijsen EM, Bergkamp MI, van Uden IW, Ghafoorian M, van der Holst HM, Norris DG, et al. Progression of white matter hyperintensities preceded by heterogeneous decline of microstructural integrity. Stroke. 2018; 49:1386–1393.
Article12. Ryoo NY, Yoon B, Yoon CW, Ahn J, Choi JY, Lim MK, et al. Diffusion tensor imaging changes correlate with clinical progression in vascular mild cognitive impairment and vascular dementia of subcortical type. Dement Neurocogn Disord. 2013; 12:61–71.
Article13. Wardlaw JM, Doubal F, Armitage P, Chappell F, Carpenter T, Muñoz Maniega S, et al. Lacunar stroke is associated with diffuse blood-brain barrier dysfunction. Ann Neurol. 2009; 65:194–202.
Article14. Shinohara Y, Katayama Y, Uchiyama S, Yamaguchi T, Handa S, Matsuoka K, et al. Cilostazol for prevention of secondary stroke (CSPS 2): an aspirin-controlled, double-blind, randomised non-inferiority trial. Lancet Neurol. 2010; 9:959–968.
Article15. Gurbel PA, Tantry US. Combination antithrombotic therapies. Circulation. 2010; 121:569–583.
Article16. de Donato G, Setacci F, Mele M, Giannace G, Galzerano G, Setacci C. Restenosis after coronary and peripheral intervention: efficacy and clinical impact of cilostazol. Ann Vasc Surg. 2017; 41:300–307.
Article17. Morishita R. A scientific rationale for the CREST trial results: evidence for the mechanism of action of cilostazol in restenosis. Atheroscler Suppl. 2005; 6:41–46.
Article18. Aoki M, Morishita R, Hayashi S, Jo N, Matsumoto K, Nakamura T, et al. Inhibition of neointimal formation after balloon injury by cilostazol, accompanied by improvement of endothelial dysfunction and induction of hepatocyte growth factor in rat diabetes model. Diabetologia. 2001; 44:1034–1042.
Article19. Kawabe-Yako R, Ii M, Masuo O, Asahara T, Itakura T. Cilostazol activates function of bone marrow-derived endothelial progenitor cell for re-endothelialization in a carotid balloon injury model. PLoS One. 2011; 6:e24646.
Article20. Edrissi H, Schock SC, Cadonic R, Hakim AM, Thompson CS. Cilostazol reduces blood brain barrier dysfunction, white matter lesion formation and motor deficits following chronic cerebral hypoperfusion. Brain Res. 2016; 1646:494–503.
Article21. Schmidt R, Berghold A, Jokinen H, Gouw AA, van der Flier WM, Barkhof F, et al. White matter lesion progression in LADIS: frequency, clinical effects, and sample size calculations. Stroke. 2012; 43:2643–2647.22. Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA. MR Signal abnormalities at 1.5T in Alzheimer's dementia and normal aging. AJR Am J Roentgenol. 1987; 149:351–356.23. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24:35–41.
Article24. Beckett LA, Donohue MC, Wang C, Aisen P, Harvey DJ, Saito N, et al. The Alzheimer's disease neuroimaging initiative phase 2: increasing the length, breadth, and depth of our understanding. Alzheimers Dement. 2015; 11:823–831.
Article25. Zhang Y, Brady M, Smith S. Segmentation of brain MR images through a hidden Markov random field model and the expectation-maximization algorithm. IEEE Trans Med Imaging. 2001; 20:45–57.
Article26. Han C, Jo SA, Jo I, Kim E, Park MH, Kang Y. An adaptation of the Korean mini-mental state examination (K-MMSE) in elderly Koreans: demographic influence and population-based norms (the AGE study). Arch Gerontol Geriatr. 2008; 47:302–310.
Article27. Choi SH, Lee BH, Kim S, Hahm DS, Jeong JH, Yoon SJ, et al. Interchanging scores between clinical dementia rating scale and global deterioration scale. Alzheimer Dis Assoc Disord. 2003; 17:98–105.
Article28. Bae JN, Cho MJ. Development of the Korean version of the Geriatric Depression Scale and its short form among elderly psychiatric patients. J Psychosom Res. 2004; 57:297–305.
Article29. Kang SJ, Choi SH, Lee BH, Jeong Y, Hahm DS, Han IW, et al. Caregiver-administered neuropsychiatric inventory (CGA-NPI). J Geriatr Psychiatry Neurol. 2004; 17:32–35.
Article30. Kim SH, Seo SW, Go SM, Chin J, Lee BH, Lee JH, et al. Pyramidal and extrapyramidal scale (PEPS): a new scale for the assessment of motor impairment in vascular cognitive impairment associated with small vessel disease. Clin Neurol Neurosurg. 2011; 113:181–187.
Article31. Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991; 39:142–148.
Article32. Oh SJ, Park HG, Paick SH, Park WH, Choo MS. Translation and Linguistic validation of Korean version of the king's health questionnaire instrument. Korean J Urol. 2005; 46:438–450.33. Choi SH, Na DL, Lee BH, Kang SJ, Ha CK, Han SH, et al. Validation of the Korean version of the Bayer activities of daily living scale. Hum Psychopharmacol. 2003; 18:469–475.
Article34. Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J. 1965; 14:61–65.35. Wardlaw JM, Smith C, Dichgans M. Small vessel disease: mechanisms and clinical implications. Lancet Neurol. 2019; 18:684–696.
Article36. Sonnen JA, Santa Cruz K, Hemmy LS, Woltjer R, Leverenz JB, Montine KS, et al. Ecology of the aging human brain. Arch Neurol. 2011; 68:1049–1056.
Article37. Schneider JA, Arvanitakis Z, Bang W, Bennett DA. Mixed brain pathologies account for most dementia cases in community-dwelling older persons. Neurology. 2007; 69:2197–2204.
Article38. Erkinjuntti T, Inzitari D, Pantoni L, Wallin A, Scheltens P, Rockwood K, et al. Research criteria for subcortical vascular dementia in clinical trials. J Neural Transm Suppl. 2000; 59:23–30.
Article39. Alber J, Alladi S, Bae HJ, Barton DA, Beckett LA, Bell JM, et al. White matter hyperintensities in vascular contributions to cognitive impairment and dementia (VCID): knowledge gaps and opportunities. Alzheimers Dement (N Y). 2019; 5:107–117.
Article40. Park JH, Heo SH, Lee MH, Kwon HS, Kwon SU, Lee JS, et al. White matter hyperintensities and recurrent stroke risk in patients with stroke with small-vessel disease. Eur J Neurol. 2019; 26:911–918.
Article41. Jorgensen DR, Shaaban CE, Wiley CA, Gianaros PJ, Mettenburg J, Rosano C. A population neuroscience approach to the study of cerebral small vessel disease in midlife and late life: an invited review. Am J Physiol Heart Circ Physiol. 2018; 314:H1117–H1136.
Article42. Mok VC, Lam WW, Fan YH, Wong A, Ng PW, Tsoi TH, et al. Effects of statins on the progression of cerebral white matter lesion: Post hoc analysis of the ROCAS (Regression of Cerebral Artery Stenosis) study. J Neurol. 2009; 256:750–757.
Article43. Dufouil C, Chalmers J, Coskun O, Besançon V, Bousser MG, Guillon P, et al. Effects of blood pressure lowering on cerebral white matter hyperintensities in patients with stroke: the PROGRESS (Perindopril Protection Against Recurrent Stroke Study) Magnetic Resonance Imaging Substudy. Circulation. 2005; 112:1644–1650.
Article44. Jokinen H, Gouw AA, Madureira S, Ylikoski R, van Straaten EC, van der Flier WM, et al. Incident lacunes influence cognitive decline: the LADIS study. Neurology. 2011; 76:1872–1878.
Article45. Qiu C, Cotch MF, Sigurdsson S, Jonsson PV, Jonsdottir MK, Sveinbjrnsdottir S, et al. Cerebral microbleeds, retinopathy, and dementia: the AGES-Reykjavik Study. Neurology. 2010; 75:2221–2228.
Article46. Kim BJ, Lee EJ, Kwon SU, Park JH, Kim YJ, Hong KS, et al. Prevention of cardiovascular events in Asian patients with ischaemic stroke at high risk of cerebral haemorrhage (PICASSO): a multicentre, randomised controlled trial. Lancet Neurol. 2018; 17:509–518.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship Between Cerebral Microbleeds and Aspirin Use Regarding White Matter Hyperintensity Volume
- Prevention and Management of Cerebral Small Vessel Disease
- Lacunar Infarction and Small Vessel Disease: Pathology and Pathophysiology
- Prognostic Impact of Cerebral Small Vessel Disease on Stroke Outcome
- Evolving Concept of Small Vessel Disease through Advanced Brain Imaging