Neonatal Med.
2019 Nov;26(4):198-203. 10.5385/nm.2019.26.4.198.
Perinatal Risk Factors for Postnatal Weight Loss in Late Preterm Infants
- Affiliations
-
- 1Department of Pediatrics, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea.
- 2Department of Pediatrics, Soonchunhyang University Cheonan Hospital, Soonchunhyang University College of Medicine, Cheonan, Korea. joonanii@naver.com
- KMID: 2466639
- DOI: http://doi.org/10.5385/nm.2019.26.4.198
Abstract
- PURPOSE
Many studies have reported associations of early postnatal growth failure in preterm infants with several morbidities. However, the risk factors for postnatal weight loss (PWL) in late preterm infants have not been identified. We investigated the independent risk factors for PWL in late preterm infants.
METHODS
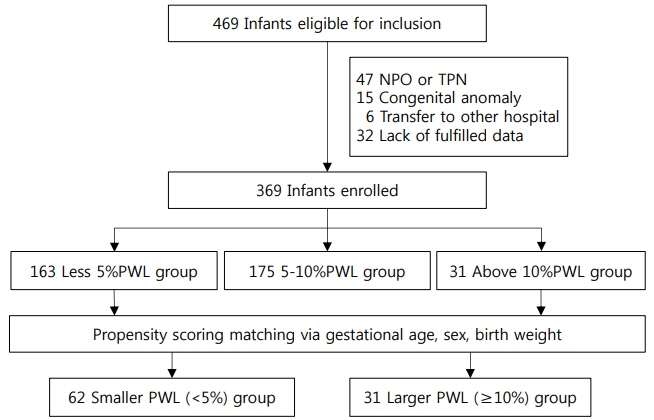
This was a retrospective cohort study. We enrolled 369 late preterm infants born at 34âºâ° to 36âºâ¶ weeks gestational age who were admitted to the Soonchunhyang University Cheonan Hospital between 2015 and 2017. PWL% was calculated as (birth weight-lowest weight)/birth weight×100. The infants were classified into lower (< 5%) and higher (≥10%) PWL% groups by propensity score matching for gestational age, sex, and birth weight. Perinatal risk factors were analyzed using multivariable logistic regression.
RESULTS
The lower and higher PWL% groups included 62 and 31 infants, respectively. Antenatal steroids administered within 1 week before birth (odds ratio [OR], 3.26; 95% confidence interval [CI], 1.015 to 10.465; P=0.047), lower total calorie intake during days 1 to 7 (OR, 0.98; 95% CI, 0.977 to 0.999; P=0.027), and phototherapy (OR, 5.28; 95% CI, 1.327 to 21.024; P=0.018) were independent risk factors for the higher PWL%.
CONCLUSION
Further studies are needed to identify the risk factors that cause high PWL% according to gestational age and short- and long-term morbidities based on the degree of PWL.
Keyword
MeSH Terms
Figure
Reference
-
1. Paul IM, Schaefer EW, Miller JR, Kuzniewicz MW, Li SX, Walsh EM, et al. Weight change nomograms for the first month after birth. Pediatrics. 2016; 138:e20162625.2. Jaiswal A, Murki S, Gaddam P, Reddy A. Early neonatal morbidities in late preterm infants. Indian Pediatr. 2011; 48:607–11.3. Teune MJ, Bakhuizen S, Gyamfi Bannerman C, Opmeer BC, van Kaam AH, van Wassenaer AG, et al. A systematic review of severe morbidity in infants born late preterm. Am J Obstet Gynecol. 2011; 205:374.4. Tsai ML, Lien R, Chiang MC, Hsu JF, Fu RH, Chu SM, et al. Prevalence and morbidity of late preterm infants: current status in a medical center of Northern Taiwan. Pediatr Neonatol. 2012; 53:171–7.5. Muelbert M, Harding JE, Bloomfield FH. Nutritional policies for late preterm and early term infants: can we do better? Semin Fetal Neonatal Med. 2019; 24:43–7.6. Aksoy HT, Guzoglu N, Eras Z, Gokce IK, Canpolat FE, Uras N, et al. The association of early postnatal weight loss with outcome in extremely low birth weight infants. Pediatr Neonatol. 2019; 60:192–6.7. Bauer K, Versmold H. Postnatal weight loss in preterm neonates less than 1,500 g is due to isotonic dehydration of the extracellular volume. Acta Paediatr Scand Suppl. 1989; 360:37–42.8. Hartnoll G, Betremieux P, Modi N. Body water content of extremely preterm infants at birth. Arch Dis Child Fetal Neonatal Ed. 2000; 83:F56–9.9. Eriksson L, Haglund B, Ewald U, Odlind V, Kieler H. Short and long-term effects of antenatal corticosteroids assessed in a cohort of 7,827 children born preterm. Acta Obstet Gynecol Scand. 2009; 88:933–8.10. Mulder EJ, de Heus R, Visser GH. Antenatal corticosteroid therapy: short-term effects on fetal behaviour and haemodynamics. Semin Fetal Neonatal Med. 2009; 14:151–6.11. Wapner RJ, Sorokin Y, Mele L, Johnson F, Dudley DJ, Spong CY, et al. Long-term outcomes after repeat doses of antenatal corticosteroids. N Engl J Med. 2007; 357:1190–8.12. Verma RP, Shibli S, Fang H, Komaroff E. Clinical determinants and utility of early postnatal maximum weight loss in fluid management of extremely low birth weight infants. Early Hum Dev. 2009; 85:59–64.13. Omar SA, DeCristofaro JD, Agarwal BI, La Gamma EF. Effects of prenatal steroids on water and sodium homeostasis in extremely low birth weight neonates. Pediatrics. 1999; 104(3 Pt 1):482–8.14. Sifianou P, Thanou V, Karga H. Metabolic and hormonal effects of antenatal betamethasone after 35 weeks of gestation. J Pediatr Pharmacol Ther. 2015; 20:138–43.15. Gyamfi-Bannerman C, Thom EA, Blackwell SC, Tita AT, Reddy UM, Saade GR, et al. Antenatal betamethasone for women at risk for late preterm delivery. N Engl J Med. 2016; 374:1311–20.16. Thorp JA, Jones PG, Peabody JL, Knox E, Clark RH. Effect of antenatal and postnatal corticosteroid therapy on weight gain and head circumference growth in the nursery. Obstet Gynecol. 2002; 99:109–15.17. Battin M, Bevan C, Harding J. Growth in the neonatal period after repeat courses of antenatal corticosteroids: data from the ACTORDS randomised trial. Arch Dis Child Fetal Neonatal Ed. 2012; 97:F99–105.18. Moltu SJ, Blakstad EW, Strommen K, Almaas AN, Nakstad B, Ronnestad A, et al. Enhanced feeding and diminished postnatal growth failure in very-low-birth-weight infants. J Pediatr Gastroenterol Nutr. 2014; 58:344–51.19. Lee SM, Kim N, Namgung R, Park M, Park K, Jeon J. Prediction of postnatal growth failure among very low birth weight infants. Sci Rep. 2018; 8:3729.20. Binchy A, Moore Z, Patton D. Feeding intervals in premature infants ≤1750 g: an integrative review. Adv Neonatal Care. 2018; 18:168–78.21. Li YW, Yan CY, Yang L, Han ZL. Effect of breastfeeding versus formula milk feeding on preterm infants in the neonatal intensive care unit. Zhongguo Dang Dai Er Ke Za Zhi. 2017; 19:572–5.22. Verma RP, Shibli S, Komaroff E. Postnatal transitional weight loss and adverse outcomes in extremely premature neonates. Pediatr Rep. 2017; 9:6962.23. Modi N. Clinical implications of postnatal alterations in body water distribution. Semin Neonatol. 2003; 8:301–6.24. Salas AA, Salazar J, Burgoa CV, De-Villegas CA, Quevedo V, Soliz A. Significant weight loss in breastfed term infants readmitted for hyperbilirubinemia. BMC Pediatr. 2009; 9:82.25. Wadhawan R, Oh W, Perritt R, Laptook AR, Poole K, Wright LL, et al. Association between early postnatal weight loss and death or BPD in small and appropriate for gestational age extremely low-birth-weight infants. J Perinatol. 2007; 27:359–64.26. Oh W, Poindexter BB, Perritt R, Lemons JA, Bauer CR, Ehrenkranz RA, et al. Association between fluid intake and weight loss during the first ten days of life and risk of bronchopulmonary dysplasia in extremely low birth weight infants. J Pediatr. 2005; 147:786–90.27. Bertini G, Perugi S, Elia S, Pratesi S, Dani C, Rubaltelli FF. Transepidermal water loss and cerebral hemodynamics in preterm infants: conventional versus LED phototherapy. Eur J Pediatr. 2008; 167:37–42.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Growth patterns of preterm infants in Korea
- Assessment of Preterm Infants Using the Bayley-III Scales in Korea
- Postnatal Body Weight Changes in Preterm SGA and Preterm AGA Infants on Fluid Restriction Therapy
- Readmission of late preterm infants after discharge from nursery
- Neurodevelopmental outcomes of preterm infants