Pregnancy Outcomes of Women Additionally Diagnosed as Gestational Diabetes by the International Association of the Diabetes and Pregnancy Study Groups Criteria
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Cheil General Hospital & Women's Healthcare Center, Dankook University College of Medicine, Seoul, Korea.
- 2Department of Internal Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Internal Medicine, Cheil General Hospital & Women's Healthcare Center, Dankook University College of Medicine, Seoul, Korea.
- 4Department of Obstetrics and Gynecology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- 5Department of Pediatrics, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- 6Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. janghak@snu.ac.kr
- KMID: 2466498
- DOI: http://doi.org/10.4093/dmj.2018.0192
Abstract
- BACKGROUND
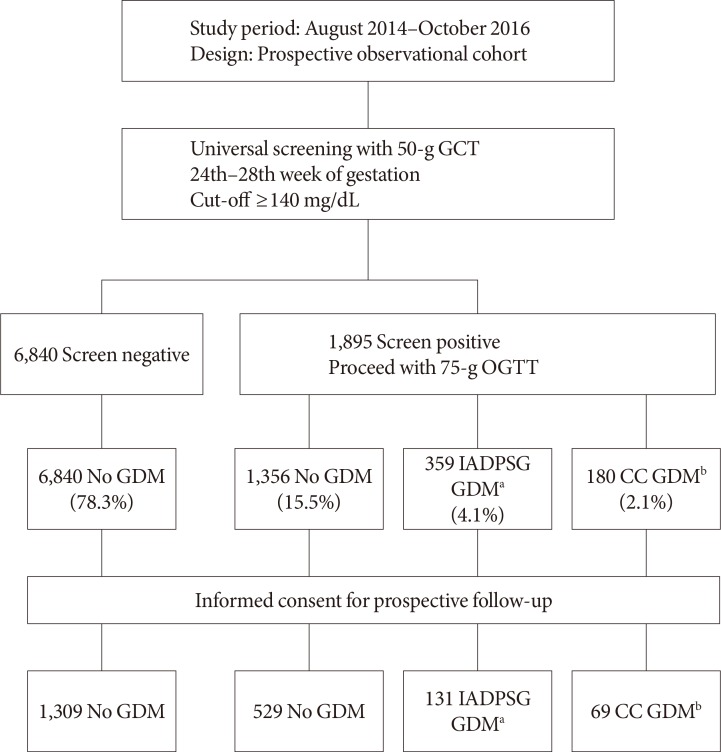
We investigated the pregnancy outcomes in women who were diagnosed with gestational diabetes mellitus (GDM) by the International Association of the Diabetes and Pregnancy Study Groups (IADPSG) criteria but not by the Carpenter-Coustan (CC) criteria.
METHODS
A total of 8,735 Korean pregnant women were identified at two hospitals between 2014 and 2016. Among them, 2,038 women participated in the prospective cohort to investigate pregnancy outcomes. Diagnosis of GDM was made via two-step approach with 50-g glucose challenge test for screening followed by diagnostic 2-hour 75-g oral glucose tolerance test. Women were divided into three groups: non-GDM, GDM diagnosed exclusively by the IADPSG criteria, and GDM diagnosed by the CC criteria.
RESULTS
The incidence of GDM was 2.1% according to the CC criteria, and 4.1% by the IADPSG criteria. Women diagnosed with GDM by the IADPSG criteria had a higher body mass index (22.0±3.1 kg/m² vs. 21.0±2.8 kg/m², P<0.001) and an increased risk of preeclampsia (odds ratio [OR], 6.90; 95% confidence interval [CI], 1.84 to 25.87; P=0.004) compared to non-GDM women. Compared to neonates of the non-GDM group, those of the IADPSG GDM group had an increased risk of being large for gestational age (OR, 2.39; 95% CI, 1.50 to 3.81; P<0.001), macrosomia (OR, 2.53; 95% CI, 1.26 to 5.10; P=0.009), and neonatal hypoglycemia (OR, 3.84; 95% CI, 1.01 to 14.74; P=0.049); they were also at an increased risk of requiring phototherapy (OR, 1.57; 95% CI, 1.07 to 2.31; P=0.022) compared to the non-GDM group.
CONCLUSION
The IADPSG criteria increased the incidence of GDM by nearly three-fold, and women diagnosed with GDM by the IADPSG criteria had an increased risk of adverse pregnancy outcomes in Korea.
MeSH Terms
Figure
Cited by 11 articles
-
Gestational Diabetes Mellitus: Diagnosis and Glycemic Control
Jung Oh Tae, Chul Jang Hak
J Korean Diabetes. 2020;21(2):69-74. doi: 10.4093/jkd.2020.21.2.69.Fetal Abdominal Obesity Detected At 24 to 28 Weeks of Gestation Persists Until Delivery Despite Management of Gestational Diabetes Mellitus
Wonjin Kim, Soo Kyung Park, Yoo Lee Kim
Diabetes Metab J. 2021;45(4):547-557. doi: 10.4093/dmj.2020.0078.Maternal Hyperglycemia during Pregnancy Increases Adiposity of Offspring
Hye Rim Chung, Joon Ho Moon, Jung Sub Lim, Young Ah Lee, Choong Ho Shin, Joon-Seok Hong, Soo Heon Kwak, Sung Hee Choi, Hak Chul Jang
Diabetes Metab J. 2021;45(5):730-738. doi: 10.4093/dmj.2020.0154.New Diagnostic Criteria for Gestational Diabetes Mellitus and Pregnancy Outcomes in Korea
Kyu Yeon Hur
Diabetes Metab J. 2019;43(6):763-765. doi: 10.4093/dmj.2019.0247.Postprandial Free Fatty Acids at Mid-Pregnancy Increase the Risk of Large-for-Gestational-Age Newborns in Women with Gestational Diabetes Mellitus
So-Yeon Kim, Young Shin Song, Soo-Kyung Kim, Yong-Wook Cho, Kyung-Soo Kim
Diabetes Metab J. 2022;46(1):140-148. doi: 10.4093/dmj.2021.0023.Gestational Diabetes Mellitus: Diagnostic Approaches and Maternal-Offspring Complications
Joon Ho Moon, Hak Chul Jang
Diabetes Metab J. 2022;46(1):3-14. doi: 10.4093/dmj.2021.0335.The Clinical Characteristics of Gestational Diabetes Mellitus in Korea: A National Health Information Database Study
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
Endocrinol Metab. 2021;36(3):628-636. doi: 10.3803/EnM.2020.948.Risk and Risk Factors for Postpartum Type 2 Diabetes Mellitus in Women with Gestational Diabetes: A Korean Nationwide Cohort Study
Mi Jin Choi, Jimi Choi, Chae Weon Chung
Endocrinol Metab. 2022;37(1):112-123. doi: 10.3803/EnM.2021.1276.Effect of Different Types of Diagnostic Criteria for Gestational Diabetes Mellitus on Adverse Neonatal Outcomes: A Systematic Review, Meta-Analysis, and Meta-Regression
Fahimeh Ramezani Tehrani, Marzieh Saei Ghare Naz, Razieh Bidhendi-Yarandi, Samira Behboudi-Gandevani
Diabetes Metab J. 2022;46(4):605-619. doi: 10.4093/dmj.2021.0178.Predicting the Risk of Insulin-Requiring Gestational Diabetes before Pregnancy: A Model Generated from a Nationwide Population-Based Cohort Study in Korea
Seung-Hwan Lee, Jin Yu, Kyungdo Han, Seung Woo Lee, Sang Youn You, Hun-Sung Kim, Jae-Hyoung Cho, Kun-Ho Yoon, Mee Kyoung Kim
Endocrinol Metab. 2023;38(1):129-138. doi: 10.3803/EnM.2022.1609.2023 Clinical Practice Guidelines for Diabetes Management in Korea: Full Version Recommendation of the Korean Diabetes Association
Jun Sung Moon, Shinae Kang, Jong Han Choi, Kyung Ae Lee, Joon Ho Moon, Suk Chon, Dae Jung Kim, Hyun Jin Kim, Ji A Seo, Mee Kyoung Kim, Jeong Hyun Lim, Yoon Ju Song, Ye Seul Yang, Jae Hyeon Kim, You-Bin Lee, Junghyun Noh, Kyu Yeon Hur, Jong Suk Park, Sang Youl Rhee, Hae Jin Kim, Hyun Min Kim, Jung Hae Ko, Nam Hoon Kim, Chong Hwa Kim, Jeeyun Ahn, Tae Jung Oh, Soo-Kyung Kim, Jaehyun Kim, Eugene Han, Sang-Man Jin, Jaehyun Bae, Eonju Jeon, Ji Min Kim, Seon Mee Kang, Jung Hwan Park, Jae-Seung Yun, Bong-Soo Cha, Min Kyong Moon, Byung-Wan Lee
Diabetes Metab J. 2024;48(4):546-708. doi: 10.4093/dmj.2024.0249.
Reference
-
1. American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2018. Diabetes Care. 2018; 41(Suppl 1):S13–S27. PMID: 29222373.2. Metzger BE, Coustan DR. Summary and recommendations of the Fourth International Workshop-Conference on Gestational Diabetes Mellitus. The Organizing Committee. Diabetes Care. 1998; 21(Suppl 2):B161–B167. PMID: 9704245.3. Jang HC, Cho NH, Min YK, Han IK, Jung KB, Metzger BE. Increased macrosomia and perinatal morbidity independent of maternal obesity and advanced age in Korean women with GDM. Diabetes Care. 1997; 20:1582–1588. PMID: 9314639.
Article4. International Association of Diabetes and Pregnancy Study Groups Consensus Panel. Metzger BE, Gabbe SG, Persson B, Buchanan TA, Catalano PA, Damm P, Dyer AR, Leiva Ad, Hod M, Kitzmiler JL, Lowe LP, McIntyre HD, Oats JJ, Omori Y, Schmidt MI. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010; 33:676–682. PMID: 20190296.
Article5. Pettitt DJ, Knowler WC, Baird HR, Bennett PH. Gestational diabetes: infant and maternal complications of pregnancy in relation to third-trimester glucose tolerance in the Pima Indians. Diabetes Care. 1980; 3:458–464. PMID: 7389563.
Article6. Ferrara A, Weiss NS, Hedderson MM, Quesenberry CP Jr, Selby JV, Ergas IJ, Peng T, Escobar GJ, Pettitt DJ, Sacks DA. Pregnancy plasma glucose levels exceeding the American Diabetes Association thresholds, but below the National Diabetes Data Group thresholds for gestational diabetes mellitus, are related to the risk of neonatal macrosomia, hypoglycaemia and hyperbilirubinaemia. Diabetologia. 2007; 50:298–306. PMID: 17103140.
Article7. Ferrara A. Increasing prevalence of gestational diabetes mellitus: a public health perspective. Diabetes Care. 2007; 30(Suppl 2):S141–S146. PMID: 17596462.8. Kim C. Gestational diabetes mellitus in Korean women: similarities and differences from other racial/ethnic groups. Diabetes Metab J. 2014; 38:1–12. PMID: 24627822.
Article9. Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS. Australian Carbohydrate Intolerance Study in Pregnant Women (ACHOIS) Trial Group. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med. 2005; 352:2477–2486. PMID: 15951574.
Article10. HAPO Study, Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U, Coustan DR, Hadden DR, McCance DR, Hod M, McIntyre HD, Oats JJ, Persson B, Rogers MS, Sacks DA. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008; 358:1991–2002. PMID: 18463375.11. Carpenter MW, Coustan DR. Criteria for screening tests for gestational diabetes. Am J Obstet Gynecol. 1982; 144:768–773. PMID: 7148898.
Article12. Sacks DA, Hadden DR, Maresh M, Deerochanawong C, Dyer AR, Metzger BE, Lowe LP, Coustan DR, Hod M, Oats JJ, Persson B, Trimble ER. HAPO Study Cooperative Research Group. Frequency of gestational diabetes mellitus at collaborating centers based on IADPSG consensus panel-recommended criteria: the Hyperglycemia and Adverse Pregnancy Outcome (HAPO) Study. Diabetes Care. 2012; 35:526–528. PMID: 22355019.13. Vandorsten JP, Dodson WC, Espeland MA, Grobman WA, Guise JM, Mercer BM, Minkoff HL, Poindexter B, Prosser LA, Sawaya GF, Scott JR, Silver RM, Smith L, Thomas A, Tita AT. NIH consensus development conference: diagnosing gestational diabetes mellitus. NIH Consens State Sci Statements. 2013; 29:1–31. PMID: 23748438.14. World Health Organization. Diagnostic criteria and classification of hyperglycaemia first detected in pregnancy. Geneva: World Health Organization;2013.15. IDF Clinical Guidelines Task Force. Global guideline for type 2 diabetes: recommendations for standard, comprehensive, and minimal care. Diabet Med. 2006; 23:579–593. PMID: 16759299.16. Committee on Practice Bulletins: Obstetrics. Obstetrics Practice bulletin no. 137: gestational diabetes mellitus. Obstet Gynecol. 2013; 122(2 Pt 1):406–416. PMID: 23969827.17. Feldman RK, Tieu RS, Yasumura L. Gestational diabetes screening: the International Association of the Diabetes and Pregnancy Study Groups compared with Carpenter-Coustan screening. Obstet Gynecol. 2016; 127:10–17. PMID: 26646142.18. Duran A, Saenz S, Torrejon MJ, Bordiu E, Del Valle L, Galindo M, Perez N, Herraiz MA, Izquierdo N, Rubio MA, Runkle I, Perez-Ferre N, Cusihuallpa I, Jimenez S, Garcia de, Fernandez MD, Montanez C, Familiar C, Calle-Pascual AL. Introduction of IADPSG criteria for the screening and diagnosis of gestational diabetes mellitus results in improved pregnancy outcomes at a lower cost in a large cohort of pregnant women: the St. Carlos Gestational Diabetes Study. Diabetes Care. 2014; 37:2442–2450. PMID: 24947793.
Article19. Waters TP, Dyer AR, Scholtens DM, Dooley SL, Herer E, Lowe LP, Oats JJ, Persson B, Sacks DA, Metzger BE, Catalano PM. HAPO Cooperative Study Research Group. Maternal and neonatal morbidity for women who would be added to the diagnosis of GDM using IADPSG criteria: a secondary analysis of the hyperglycemia and adverse pregnancy outcome study. Diabetes Care. 2016; 39:2204–2210. PMID: 27634392.
Article20. Shang M, Lin L. IADPSG criteria for diagnosing gestational diabetes mellitus and predicting adverse pregnancy outcomes. J Perinatol. 2014; 34:100–104. PMID: 24232664.
Article21. Morikawa M, Yamada T, Yamada T, Akaishi R, Nishida R, Cho K, Minakami H. Change in the number of patients after the adoption of IADPSG criteria for hyperglycemia during pregnancy in Japanese women. Diabetes Res Clin Pract. 2010; 90:339–342. PMID: 20870307.
Article22. American Diabetes Association. Standards of medical care in diabetes: 2014. Diabetes Care. 2014; 37(Suppl 1):S14–S80. PMID: 24357209.23. American College of Obstetricians and Gynecologists. Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists' Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013; 122:1122–1131. PMID: 24150027.24. American College of Obstetricians and Gynecologists' Committee on Practice Bulletins: Obstetrics. Practice bulletin no. 173: fetal macrosomia. Obstet Gynecol. 2016; 128:e195–e209. PMID: 27776071.25. Lee JJ. Birth weight for gestational age patterns by sex, plurality, and parity in Korean population. Korean J Pediatr. 2007; 50:732–739.
Article26. Brown FM, Wyckoff J. Application of one-step IADPSG versus two-step diagnostic criteria for gestational diabetes in the real world: impact on health services, clinical care, and outcomes. Curr Diab Rep. 2017; 17:85. PMID: 28799123.
Article27. Hedderson MM, Williams MA, Holt VL, Weiss NS, Ferrara A. Body mass index and weight gain prior to pregnancy and risk of gestational diabetes mellitus. Am J Obstet Gynecol. 2008; 198:409.e1–409.e7. PMID: 18068138.
Article28. Black MH, Sacks DA, Xiang AH, Lawrence JM. The relative contribution of prepregnancy overweight and obesity, gestational weight gain, and IADPSG-defined gestational diabetes mellitus to fetal overgrowth. Diabetes Care. 2013; 36:56–62. PMID: 22891256.
Article29. Agarwal MM, Dhatt GS, Othman Y. Gestational diabetes in a tertiary care hospital: implications of applying the IADPSG criteria. Arch Gynecol Obstet. 2012; 286:373–378. PMID: 22484479.
Article30. Landon MB, Spong CY, Thom E, Carpenter MW, Ramin SM, Casey B, Wapner RJ, Varner MW, Rouse DJ, Thorp JM Jr, Sciscione A, Catalano P, Harper M, Saade G, Lain KY, Sorokin Y, Peaceman AM, Tolosa JE, Anderson GB. Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. A multicenter, randomized trial of treatment for mild gestational diabetes. N Engl J Med. 2009; 361:1339–1348. PMID: 19797280.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnostic Criteria of Gestational Diabetes: The International Association of the Diabetes and Pregnancy Study Groups Compared with Carpenter-Coustan Criteria
- Diabetes in pregnancy
- Diagnosis and Medical Management of Gestational Diabetes
- Diagnostic Criteria for Gestational Diabetes in Korean Women: Is New ADA Criteria Appropriate?
- Management of Gestational Diabetes Mellitus