Korean J Radiol.
2016 Dec;17(6):931-939. 10.3348/kjr.2016.17.6.931.
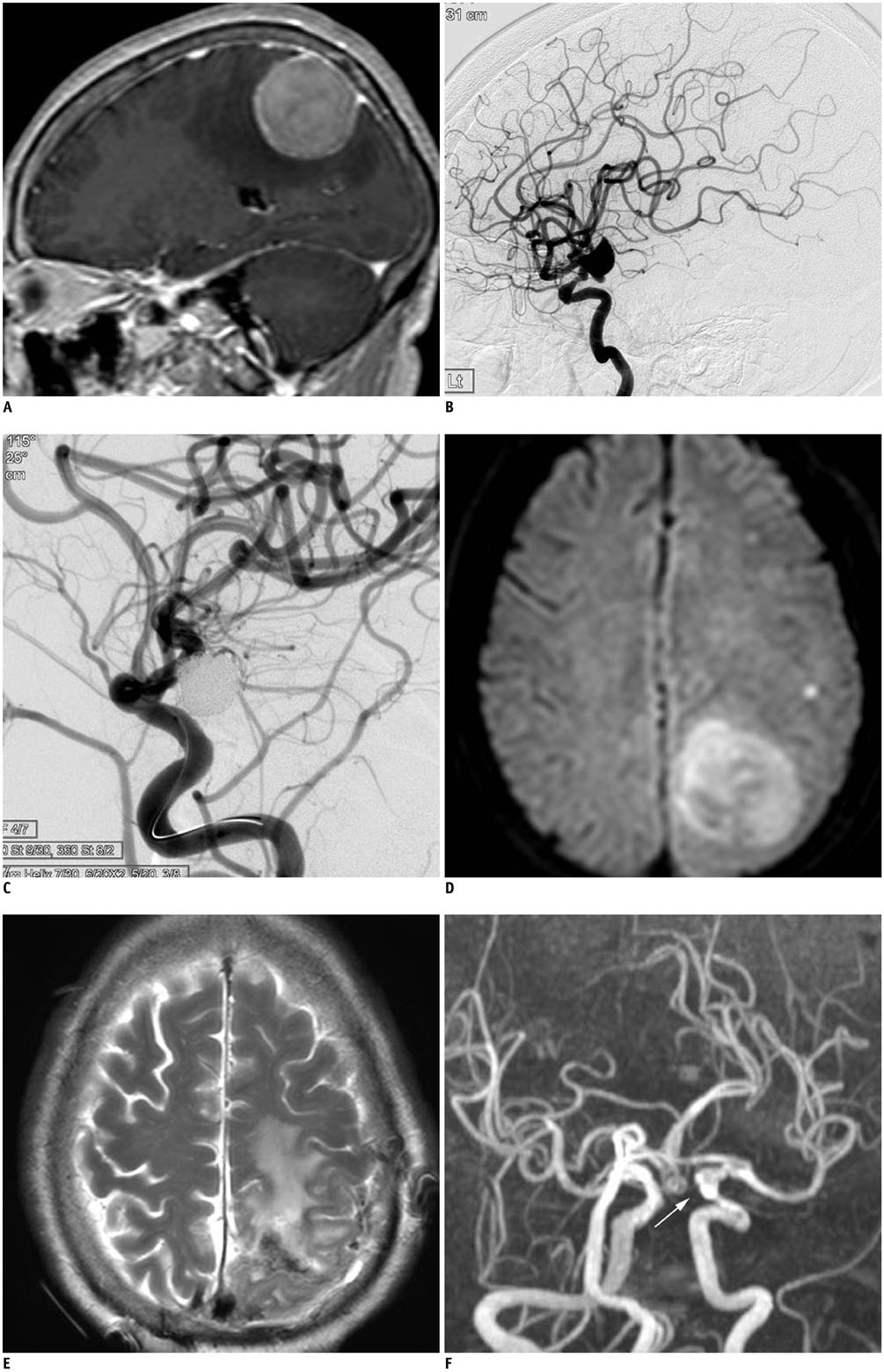
Preoperative Coiling of Coexisting Intracranial Aneurysm and Subsequent Brain Tumor Surgery
- Affiliations
-
- 1Department of Neurosurgery, Severance Hospital, Yonsei University College of Medicine, Seoul 03722, Korea.
- 2Department of Radiology, Severance Hospital, Yonsei University College of Medicine, Seoul 03722, Korea. bmoon21@hanmail.net
- KMID: 2466290
- DOI: http://doi.org/10.3348/kjr.2016.17.6.931
Abstract
OBJECTIVE
Few studies have investigated treatment strategies for brain tumor with a coexisting unruptured intracranial aneurysm (cUIA). The purpose of this study was to evaluate the safety and efficacy of preoperative coiling for cUIA, and subsequent brain tumor surgery.
MATERIALS AND METHODS
A total of 19 patients (mean age, 55.2 years; M:F = 4:15) underwent preoperative coiling for 23 cUIAs and subsequent brain tumor surgery. Primary brain tumors were meningiomas (n = 7, 36.8%), pituitary adenomas (n = 7, 36.8%), gliomas (n = 3, 15.8%), vestibular schwannoma (n = 1, 5.3%), and Rathke's cleft cyst (n = 1, 5.3%). cUIAs were located at the distal internal carotid artery (n = 9, 39.1%), anterior cerebral artery (n = 8, 34.8%), middle cerebral artery (n = 4, 17.4%), basilar artery top (n = 1, 4.3%), and posterior cerebral artery, P1 segment (n = 1, 4.3%). The outcomes of preoperative coiling of cUIA and subsequent brain tumor surgery were retrospectively evaluated.
RESULTS
Single-microcatheter technique was used in 13 cases (56.5%), balloon-assisted in 4 cases (17.4%), double-microcatheter in 4 cases (17.4%), and stent-assisted in 2 cases (8.7%). Complete cUIA occlusion was achieved in 18 cases (78.3%), while residual neck occurred in 5 cases (21.7%). The only coiling-related complication was 1 transient ischemic attack (5.3%). Neurological deterioration did not occur in any patient during the period between coiling and tumor surgery. At the latest clinical follow-up (mean, 29 months; range, 2-120 months), 15 patients (78.9%) had favorable outcomes (modified Rankin Scale, 0-2), while 4 patients (21.1%) had unfavorable outcomes due to consequences of brain tumor surgery.
CONCLUSION
Preoperative coiling and subsequent tumor surgery was safe and effective, making it a reasonable treatment option for patients with brain tumor and cUIA.
Keyword
MeSH Terms
Figure
Reference
-
1. Tsuchida T, Tanaka R, Yokoyama M, Sato H. Rupture of anterior communicating artery aneurysm during transsphenoidal surgery for pituitary adenoma. Surg Neurol. 1983; 20:67–70.2. Taylor PE. Delayed postoperative hemorrhage from intracranial aneurysm after craniotomy for tumor. Neurology. 1961; 11:225–231.3. Javalkar V, Guthikonda B, Vannemreddy P, Nanda A. Association of meningioma and intracranial aneurysm: report of five cases and review of literature. Neurol India. 2009; 57:772–776.4. Oh MC, Kim EH, Kim SH. Coexistence of intracranial aneurysm in 800 patients with surgically confirmed pituitary adenoma. J Neurosurg. 2012; 116:942–947.5. Oshino S, Nishino A, Suzuki T, Arita H, Tateishi A, Matsumoto K, et al. Prevalence of cerebral aneurysm in patients with acromegaly. Pituitary. 2013; 16:195–201.6. Pant B, Arita K, Kurisu K, Tominaga A, Eguchi K, Uozumi T. Incidence of intracranial aneurysm associated with pituitary adenoma. Neurosurg Rev. 1997; 20:13–17.7. Fischer BR, Palkovic S, Holling M, Niederstadt T, Jeibmann A, Wassmann H. Coexistence of cerebral aneurysm and meningioma--pure accident? Clin Neurol Neurosurg. 2009; 111:647–654.8. Jakubowski J, Kendall B. Coincidental aneurysms with tumours of pituitary origin. J Neurol Neurosurg Psychiatry. 1978; 41:972–979.9. Kim YH, Lee YJ, Han JH, Ahn S, Lee J, Kim JH, et al. Association of intracranial aneurysms and meningiomas: a case-control study. J Neurosurg. 2015; 123:357–361.10. Akutsu N, Hosoda K, Ohta K, Tanaka H, Taniguchi M, Kohmura E. Subarachnoid hemorrhage due to rupture of an intracavernous carotid artery aneurysm coexisting with a prolactinoma under cabergoline treatment. J Neurol Surg Rep. 2014; 75:e73–e76.11. Cheng WY, Shen CC. Minimally invasive approaches to treat simultaneous occurrence of glioblastoma multiforme and intracranial aneurysm -- case report. Minim Invasive Neurosurg. 2004; 47:181–185.12. Hoya K, Yoshimoto Y, Shin M, Nemoto S. Rupture of an internal carotid artery aneurysm within a clinoidal meningioma following stereotactic radiosurgery. Acta Neurochir (Wien). 2011; 153:1995–1996.13. Rustagi T, Uy EM, Rai M, Kannan S, Senatus P. Intracranial hemorrhage from undetected aneurysmal rupture complicating transphenoidal pituitary adenoma resection. Conn Med. 2011; 75:393–398.14. Berker M, Aghayev K, Saatci I, Palaoğlu S, Onerci M. Overview of vascular complications of pituitary surgery with special emphasis on unexpected abnormality. Pituitary. 2010; 13:160–167.15. Zhong Z, Sun Y, Lin D, Sun Q, Bian L. Surgical treatment of brain tumor coexisted with intracranial aneurysm--case series and review of the literature. Neurosurg Rev. 2013; 36:645–656. discussion 656.16. Licata C, Pasqualin A, Freschini A, Barone G, Da Pian R. Management of associated primary cerebral neoplasms and vascular malformations: 1. intracranial aneurysms. Acta Neurochir (Wien). 1986; 82:28–38.17. Yamada S, Yamada SM, Hirohata T, Ishii Y, Hoya K, Murakami M, et al. Endoscopic extracapsular removal of pituitary adenoma: the importance of pretreatment of an adjacent unruptured internal carotid artery aneurysm. Case Rep Neurol Med. 2012; 2012:891847.18. Xia X, Ramanathan M, Orr BA, Salmasi V, Salvatori R, Reh DD, et al. Expanded endonasal endoscopic approach for resection of a growth hormone-secreting pituitary macroadenoma coexistent with a cavernous carotid artery aneurysm. J Clin Neurosci. 2012; 19:1437–1441.19. Yu K, Herwadkar A, Kearney T, Gnanalingham KK. Pituitary adenoma and incidental superior hypophyseal aneurysm. Br J Neurosurg. 2011; 25:432–433.20. Cho YD, Rhim JK, Kang HS, Park JJ, Jeon JP, Kim JE, et al. Use of triple microcatheters for endovascular treatment of wide-necked intracranial aneurysms: a single center experience. Korean J Radiol. 2015; 16:1109–1118.21. Cho YD, Rhim JK, Park JJ, Jeon JS, Yoo RE, Kang HS, et al. Microcatheter looping to facilitate aneurysm selection in coil embolization of paraclinoid aneurysms. Korean J Radiol. 2015; 16:899–905.22. Kim BM, Shin YS, Baik MW, Lee DH, Jeon P, Baik SK, et al. Pipeline embolization device for large/giant or fusiform aneurysms: an initial multi-center experience in Korea. Neurointervention. 2016; 11:10–17.23. Kwon WH, Jeong HW, Kim ST, Seo JH. Angiographic and clinical result of endovascular treatment in paraclinoid aneurysms. Neurointervention. 2014; 9:83–88.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Life-threatening Blood-Brain Barrier Disruption after Coiling of Unruptured Intracranial Aneurysm: Role of Immediate Postembolization CT scanning
- Coiling as Retreatment in Intracranial Aneurysm of de novo Formation or Regrowth: Case Report
- Current Update on the Randomized Controlled Trials of Intracranial Aneurysms
- Delayed Self-expansion Phenomenon as a Complication of Neuroform Stent Assisted Coiling for Ruptured Intracranial Aneurysm
- Comprehension of Two Modalities: Endovascular Coiling and Microsurgical Clipping in Treatment of Intracranial Aneurysms