Endocrinol Metab.
2019 Dec;34(4):415-421. 10.3803/EnM.2019.34.4.415.
Revisiting Rupture of Benign Thyroid Nodules after Radiofrequency Ablation: Various Types and Imaging Features
- Affiliations
-
- 1Department of Radiology and the Research Institute of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. radbaek@naver.com
- 2Department of Radiology and Thyroid Center, Daerim St. Mary's Hospital, Seoul, Korea.
- 3Department of Radiology, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea.
- 4Department of Radiology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 2466261
- DOI: http://doi.org/10.3803/EnM.2019.34.4.415
Abstract
- BACKGROUND
To evaluate the imaging features, clinical manifestations, and prognosis of patients with thyroid nodule rupture after radiofrequency ablation (RFA).
METHODS
The records of 12 patients who experienced thyroid nodule rupture after RFA at four Korean thyroid centers between March 2010 and July 2017 were retrospectively reviewed. Clinical data evaluated included baseline patient characteristics, treatment methods, initial presenting symptoms, imaging features, treatment, and prognosis.
RESULTS
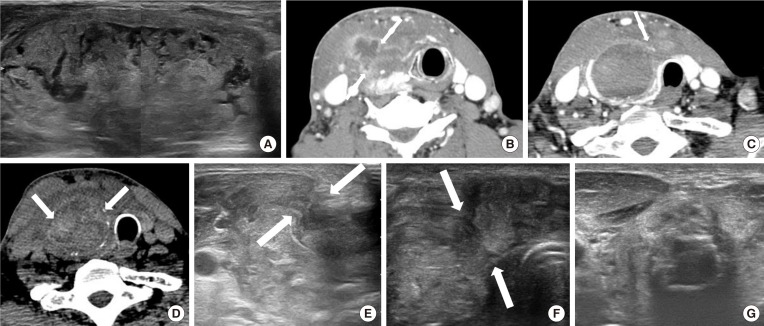
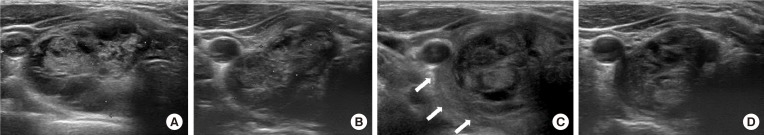
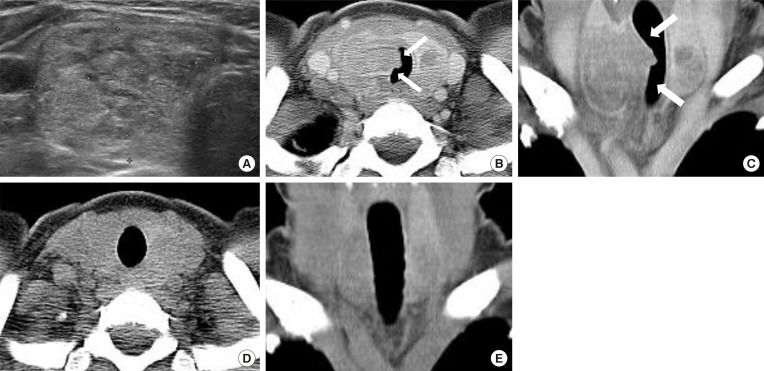
The most common symptoms of post-RFA nodule rupture were sudden neck bulging and pain. Based on imaging features, the localization of nodule rupture was classified into three types: anterior, posterolateral, and medial types. The anterior type is the most often, followed by posterolateral and medial type. Eight patients recovered completely after conservative treatment. Four patients who did not improve with conservative management required invasive procedures, including incision and drainage or aspiration.
CONCLUSION
Thyroid nodule rupture after RFA can be classified into three types based on its localization: anterior, posterolateral, and medial types. Because majority of thyroid nodule ruptures after RFA can be managed conservatively, familiarity with these imaging features is essential in avoiding unnecessary imaging workup or invasive procedures.
MeSH Terms
Figure
Cited by 1 articles
-
Effectiveness of Injecting Cold 5% Dextrose into Patients with Nerve Damage Symptoms during Thyroid Radiofrequency Ablation
Min Kyoung Lee, Jung Hwan Baek, Sae Rom Chung, Young Jun Choi, Yu-Mi Lee, Tae Yong Kim, Jeong Hyun Lee
Endocrinol Metab. 2020;35(2):407-415. doi: 10.3803/EnM.2020.35.2.407.
Reference
-
1. Baek JH, Moon WJ, Kim YS, Lee JH, Lee D. Radiofrequency ablation for the treatment of autonomously functioning thyroid nodules. World J Surg. 2009; 33:1971–1977. PMID: 19575141.
Article2. Jeong WK, Baek JH, Rhim H, Kim YS, Kwak MS, Jeong HJ, et al. Radiofrequency ablation of benign thyroid nodules: safety and imaging follow-up in 236 patients. Eur Radiol. 2008; 18:1244–1250. PMID: 18286289.
Article3. Kim YS, Rhim H, Tae K, Park DW, Kim ST. Radiofrequency ablation of benign cold thyroid nodules: initial clinical experience. Thyroid. 2006; 16:361–367. PMID: 16646682.
Article4. Baek JH, Kim YS, Lee D, Huh JY, Lee JH. Benign predominantly solid thyroid nodules: prospective study of efficacy of sonographically guided radiofrequency ablation versus control condition. AJR Am J Roentgenol. 2010; 194:1137–1142. PMID: 20308523.
Article5. Baek JH, Kim YS, Sung JY, Choi H, Lee JH. Locoregional control of metastatic well-differentiated thyroid cancer by ultrasound-guided radiofrequency ablation. AJR Am J Roentgenol. 2011; 197:W331–W336. PMID: 21785061.
Article6. Guenette JP, Monchik JM, Dupuy DE. Image-guided ablation of postsurgical locoregional recurrence of biopsy-proven well-differentiated thyroid carcinoma. J Vasc Interv Radiol. 2013; 24:672–679. PMID: 23622038.
Article7. Kim JH, Yoo WS, Park YJ, Park DJ, Yun TJ, Choi SH, et al. Efficacy and safety of radiofrequency ablation for treatment of locally recurrent thyroid cancers smaller than 2 cm. Radiology. 2015; 276:909–918. PMID: 25848897.
Article8. Baek JH, Lee JH, Sung JY, Bae JI, Kim KT, Sim J, et al. Complications encountered in the treatment of benign thyroid nodules with US-guided radiofrequency ablation: a multicenter study. Radiology. 2012; 262:335–342. PMID: 21998044.
Article9. Wang JF, Wu T, Hu KP, Xu W, Zheng BW, Tong G, et al. Complications following radiofrequency ablation of benign thyroid nodules: a systematic review. Chin Med J (Engl). 2017; 130:1361–1370. PMID: 28524837.10. Chung SR, Suh CH, Baek JH, Park HS, Choi YJ, Lee JH. Safety of radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers: a systematic review and meta-analysis. Int J Hyperthermia. 2017; 33:920–930. PMID: 28565997.
Article11. Kim JH, Baek JH, Lim HK, Ahn HS, Baek SM, Choi YJ, et al. 2017 thyroid radiofrequency ablation guideline: Korean Society of Thyroid Radiology. Korean J Radiol. 2018; 19:632–655. PMID: 29962870.
Article12. Shin JH, Jung SL, Baek JH, Kim JH. Rupture of benign thyroid tumors after radio-frequency ablation. AJNR Am J Neuroradiol. 2011; 32:2165–2169. PMID: 21920870.
Article13. Che Y, Jin S, Shi C, Wang L, Zhang X, Li Y, et al. Treatment of benign thyroid nodules: comparison of surgery with radiofrequency ablation. AJNR Am J Neuroradiol. 2015; 36:1321–1325. PMID: 25814656.
Article14. Valcavi R, Tsamatropoulos P. Health-related quality of life after percutaneous radiofrequency ablation of cold, solid, benign thyroid nodules: a 2-year follow-up study in 40 patients. Endocr Pract. 2015; 21:887–896. PMID: 26121459.
Article15. Na DG, Baek JH, Jung SL, Kim JH, Sung JY, Kim KS, et al. Core needle biopsy of the thyroid: 2016 consensus statement and recommendations from Korean Society of Thyroid Radiology. Korean J Radiol. 2017; 18:217–237. PMID: 28096731.
Article16. Shin JH, Baek JH, Chung J, Ha EJ, Kim JH, Lee YH, et al. Ultrasonography diagnosis and imaging-based management of thyroid nodules: revised Korean Society of Thyroid Radiology consensus statement and recommendations. Korean J Radiol. 2016; 17:370–395. PMID: 27134526.
Article17. Baek JH. Current status of core needle biopsy of the thyroid. Ultrasonography. 2017; 36:83–85. PMID: 28301922.
Article18. Park HS, Baek JH, Park AW, Chung SR, Choi YJ, Lee JH. Thyroid radiofrequency ablation: updates on innovative devices and techniques. Korean J Radiol. 2017; 18:615–623. PMID: 28670156.
Article19. Park HS, Baek JH, Choi YJ, Lee JH. Innovative techniques for image-guided ablation of benign thyroid nodules: combined ethanol and radiofrequency ablation. Korean J Radiol. 2017; 18:461–469. PMID: 28458598.
Article20. Sim JS, Baek JH, Lee J, Cho W, Jung SI. Radiofrequency ablation of benign thyroid nodules: depicting early sign of regrowth by calculating vital volume. Int J Hyperthermia. 2017; 33:905–910. PMID: 28540795.
Article21. Ha EJ, Baek JH, Lee JH. Ultrasonography-based thyroidal and perithyroidal anatomy and its clinical significance. Korean J Radiol. 2015; 16:749–766. PMID: 26175574.
Article22. Deandrea M, Limone P, Basso E, Mormile A, Ragazzoni F, Gamarra E, et al. US-guided percutaneous radiofrequency thermal ablation for the treatment of solid benign hyperfunctioning or compressive thyroid nodules. Ultrasound Med Biol. 2008; 34:784–791. PMID: 18207307.
Article23. Lee JH, Kim YS, Lee D, Choi H, Yoo H, Baek JH. Radiofrequency ablation (RFA) of benign thyroid nodules in patients with incompletely resolved clinical problems after ethanol ablation (EA). World J Surg. 2010; 34:1488–1493. PMID: 20376445.
Article24. Spiezia S, Garberoglio R, Milone F, Ramundo V, Caiazzo C, Assanti AP, et al. Thyroid nodules and related symptoms are stably controlled two years after radiofrequency thermal ablation. Thyroid. 2009; 19:219–225. PMID: 19265492.
Article25. Hong MJ, Baek JH, Choi YJ, Lee JH, Lim HK, Shong YK, et al. Radiofrequency ablation is a thyroid function-preserving treatment for patients with bilateral benign thyroid nodules. J Vasc Interv Radiol. 2015; 26:55–61. PMID: 25446422.26. Lim HK, Lee JH, Ha EJ, Sung JY, Kim JK, Baek JH. Radiofrequency ablation of benign non-functioning thyroid nodules: 4-year follow-up results for 111 patients. Eur Radiol. 2013; 23:1044–1049. PMID: 23096937.
Article27. Ha EJ, Baek JH, Kim KW, Pyo J, Lee JH, Baek SH, et al. Comparative efficacy of radiofrequency and laser ablation for the treatment of benign thyroid nodules: systematic review including traditional pooling and Bayesian network meta-analysis. J Clin Endocrinol Metab. 2015; 100:1903–1911. PMID: 25695887.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effective and Safe Application of Radiofrequency Ablation for Benign Thyroid Nodules
- Non-surgical, Image-guided Management of Benign Thyroid Nodules
- Ultrasound (US)-Guided Ablation of Thyroid Nodules
- Radiofrequency Ablation of Benign Thyroid Nodule
- Effective and Safe Application of Radiofrequency Ablation for Benign Thyroid Nodules