J Korean Ophthalmol Soc.
2019 Dec;60(12):1263-1268. 10.3341/jkos.2019.60.12.1263.
Analysis on Transitional Change of Refractive Error Distributions in Pediatric Population Using KNHANES
- Affiliations
-
- 1Department of Ophthalmology, Kim's Eye Hospital, Konyang University College of Medicine, Seoul, Korea. skdh17@hanmail.net
- 2Department of Ophthalmology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2466180
- DOI: http://doi.org/10.3341/jkos.2019.60.12.1263
Abstract
- PURPOSE
To investigate transitional changes in refractive error distributions in a pediatric population using the Korean National Health and Nutrition Examination Survey (KNHANES) data.
METHODS
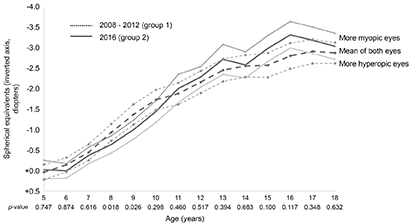
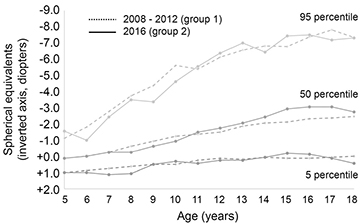
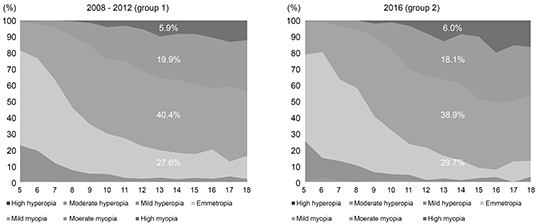
We investigated 7,181 subjects from the 4th and 5th (2008-2012) KNHANES and 1,225 subjects from the 7th (2016) KNHANES; all subjects were 5 to 18 years of age. We used the average spherical equivalent (SE) of both eyes calculated with noncycloplegic refractive errors measured via autorefractor. We determined SE percentiles by age in order from hyperopia to myopia. We acquired the mean SE by age. We investigated the proportions of subjects with mild, moderate, and severe refractive errors by age.
RESULTS
Mean refractive errors were −1.73 ± 2.16 diopters in subjects in the 4th and 5th KNHANES and −1.66 ± 2.21 diopters in subjects in the 7th KNHANES; these were not significantly different between the two groups (p = 0.071). Mean refractive errors were more myopic in subjects in the 4th and 5th than in subjects in the 7th KNHANES only at 8 and 9 years of age (p = 0.018, p = 0.026). The distribution of percentiles by age was similar between the two groups. The respective proportions of hyperopia, emmetropia, and myopia were 6.2%, 27.6%, and 66.2% in subjects in the 4th and 5th survey, and 7.3%, 29.7% and 63.0% in subjects in the 7th survey. There was no significant difference in refractive error proportion between the 2 groups (p = 0.326).
CONCLUSIONS
There was no definite transitional change of refractive error distributions between the two KNHANES groups. However, additional periodic surveys are needed to confirm this hypothesis.
Keyword
Figure
Reference
-
1. Rudnicka AR, Kapetanakis VV, Wathern AK, et al. Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: implications for aetiology and early prevention. Br J Ophthalmol. 2016; 100:882–890.2. Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016; 123:1036–1042.3. McMonnies CW. Clinical prediction of the need for interventions for the control of myopia. Clin Exp Optom. 2015; 98:518–526.4. Saw SM, Gazzard G, Shin-Yen EC, Chua WH. Myopia and associated pathological complications. Ophthalmic Physiol Opt. 2005; 25:381–391.5. Yam JC, Jiang Y, Tang SM, et al. Low-concentration atropine for myopia progression (LAMP) study: a randomized, double-blinded, placebo-controlled trial of 0.05%, 0.025%, and 0.01% atropine eye drops in myopia control. Ophthalmology. 2019; 126:113–124.6. Leo SW. Scientific Bureau of World Society of Paediatric Ophthalmology and Strabismus (WSPOS). Current approaches to myopia control. Curr Opin Ophthalmol. 2017; 28:267–275.7. Chia A, Lu QS, Tan D. Five-year clinical trial on atropine for the treatment of myopia 2: myopia control with atropine 0.01% eyedrops. Ophthalmology. 2016; 123:391–399.8. Cho P, Cheung SW. Retardation of myopia in orthokeratology (ROMIO) study: a 2-year randomized clinical trial. Invest Ophthalmol Vis Sci. 2012; 53:7077–7085.9. Kim DH, Lim HT. Myopia growth chart based on a population-based survey (KNHANES IV-V): a novel prediction model of myopic progression in childhood. J Pediatr Ophthalmol Strabismus. 2019; 56:73–77.10. Jung SI, Han J, Kwon JW, et al. Analysis of myopic progression in childhood using the Korea National Health and Nutrition Examination Survey. J Korean Ophthalmol Soc. 2016; 57:1430–1434.11. Morgan IG, French AN, Ashby RS, et al. The epidemics of myopia: aetiology and prevention. Prog Retin Eye Res. 2018; 62:134–149.12. Lee JO, Kim JH. Follow-up study of refractive errors in school children. J Korean Ophthalmol Soc. 1980; 21:517–523.13. Lee MJ, Lee YH, Shyn KH. The progression of myopia with age. J Korean Ophthalmol Soc. 1987; 28:151–155.14. Choi KW, Koo BS, Lee HY. Preschool vision screening in Korea: results in 2003. J Korean Ophthalmol Soc. 2006; 47:112–120.15. Kang SH, Kim PS, Choi DG. Prevalence of myopia in 19-year-old Korean males: the relationship between the prevalence and education or urbanization. J Korean Ophthalmol Soc. 2004; 45:2082–2087.16. Han ER, Kang JE, Jun RM, Choi KR. Changes of refractive errors and optometric values in fourth graders at an urban elementary school in Korea. J Korean Ophthalmol Soc. 2007; 48:1119–1125.17. Lee SJ, Kim JM, Yu BC, et al. Prevalence of myopia in 19-year-old men in Gyeongsangnam-do, Ulsan and Busan in 2002. J Korean Ophthalmol Soc. 2009; 50:1392–1403.18. Jung SK, Lee JH, Kakizaki H, Jee D. Prevalence of myopia and its association with body stature and educational level in 19-year-old male conscripts in Seoul, South Korea. Invest Ophthalmol Vis Sci. 2012; 53:5579–5583.19. Lim HT, Yoon JS, Hwang SS, Lee SY. Prevalence and associated sociodemographic factors of myopia in Korean children: the 2005 third Korea National Health and Nutrition Examination Survey (KNHANES III). Jpn J Ophthalmol. 2012; 56:76–81.20. Lee JH, Jee D, Kwon JW, Lee WK. Prevalence and risk factors for myopia in a rural Korean population. Invest Ophthalmol Vis Sci. 2013; 54:5466–5470.21. Jung JW, Kim YE, Paik HJ. Clinical comparison of autorefractor versus retinoscopic refraction in children according to the age. J Korean Ophthalmol Soc. 2005; 46:1931–1935.22. Choi MJ, Baek SH, Gong SM. Comparison of autorefraction and clinical refraction with or without in children. J Korean Ophthalmol Soc. 2005; 46:837–846.23. Goss DA, Cox VD, Herrin-Lawson GA, et al. Refractive error, axial length, and height as a function of age in young myopes. Optom Vis Sci. 1990; 67:332–338.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analysis of Myopic Progression in Childhood Using the Korea National Health and Nutrition Examination Survey
- Intraocular Lens Power Calculation According to the Difference between Anterior and Total Keratometry Using Scheimpflug Imaging
- Relationship between Uncorrected Visual Acuity and Refractive Error in Visual Acuity Test of Children
- Prevalence and Risk Factors for Undercorrected Refractive Errors among South Korean: KNHANES 2008-2012
- A Study of the Ocular Findings According to Subdivided Myepia