J Korean Ophthalmol Soc.
2019 Dec;60(12):1140-1147. 10.3341/jkos.2019.60.12.1140.
The Correlation between Tear Matrix Metalloproteinase-9 Concentration and Clinical Findings in Dry Eye Disease
- Affiliations
-
- 1Department of Ophthalmology, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea. qthoi85@hanmail.net
- KMID: 2466163
- DOI: http://doi.org/10.3341/jkos.2019.60.12.1140
Abstract
- PURPOSE
To investigate the correlation between the matrix metalloproteinase-9 (MMP-9) concentration, and subjective symptoms and objective signs in dry eye patients.
METHODS
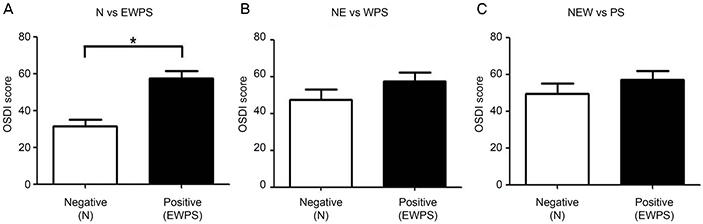
We retrospectively reviewed the medical records of 134 eyes of 67 patients who were diagnosed with dry eye disease. The results of tear MMP-9, which were conducted at a care testing facility, were defined as negative (N), equivocal (E), weak positive (W), positive (P) or strong positive (S). Using three methods with different classification ranges, MMP-9 results were classified into a negative group or positive group. The objective signs of dry eye disease, including tear break-up time (TBUT), tear volume measured by Schirmer's test, degree of corneal erosion estimated by the Oxford stain score (OSS), and ocular surface disease index (OSDI) as the subjective symptom, were recorded. The differences of indices were compared between the negative and positive groups.
RESULTS
There was no significant difference of the TBUT, Schirmer's test, or OSS between the MMP-9 negative and positive groups. Also, the percentage of females was significantly higher in the negative group compared with the positive group regardless of the classification methods (all, p < 0.05). When the MMP-9N alone was classified as a negative group, the OSDI score was significantly higher in the positive group when compared to that of the negative group (p = 0.009).
CONCLUSIONS
The measurement of MMP-9 in patients with dry eye disease may be helpful in predicting subjective symptoms of dry eye disease.
Keyword
MeSH Terms
Figure
Reference
-
1. Lemp MA. Report of the national eye institute/industry workshop on clinical trials in dry eyes. CLAO J. 1995; 21:221–232.2. The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007; 5:75–92.3. Methodologies to diagnose and monitor dry eye disease: report of the Diagnostic Methodology Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007; 5:108–152.4. Uchino M, Dogru M, Yagi Y, et al. The features of dry eye disease in a Japanese elderly population. Optom Vis Sci. 2006; 83:797–802.5. Ahn JM, Lee SH, Rim TH, et al. Prevalence of and risk factors associated with dry eye: the Korea National Health and Nutrition Examination Survey 2010-2011. Am J Ophthalmol. 2014; 158:1205–1214.6. Roh HC, Lee JK, Kim M, et al. Systemic comorbidities of dry eye syndrome: the Korean National Health and Nutrition Examination Survey V, 2010 to 2012. Cornea. 2016; 35:187–192.7. Bron AJ. Diagnosis of dry eye. Surv Ophthalmol. 2001; 45 Suppl 2:S221–S226.8. Mishima S, Kubota Z, Farris RL. The tear flow dynamics in normal and in keratoconjunctivitis sicca cases. Excerpta Medica Int Congr Ser. 1970; 222:1801–1805.9. Baudouin C, Aragona P, Van Setten G, et al. Diagnosing the severity of dry eye: a clear and practical algorithm. Br J Ophthalmol. 2014; 98:1168–1176.10. Messmer EM, von Lindenfels V, Garbe A, Kampik A. Matrix metalloproteinase 9 testing in dry eye disease using a commercially available point-of-care immunoassay. Ophthalmology. 2016; 123:2300–2308.11. Lanza NL, Valenzuela F, Perez VL, Galor A. The matrix metalloproteinase 9 point-of-care test in dry eye. Ocul Surf. 2016; 14:189–195.12. Lanza NL, McClellan AL, Batawi H, et al. Dry eye profiles in patients with a positive elevated surface matrix metalloproteinase 9 point-of-care test versus negative patients. Ocul Surf. 2016; 14:216–223.13. Seo MH, Shin JY, Lee DH, Kim JH. Objective parameters associated with subjective symptom severity in dry eye syndrome patients. J Korean Ophthalmol Soc. 2017; 58:259–267.14. Sambursky R, Davitt WF 3rd, Latkany R, et al. Sensitivity and specificity of a point-of-care matrix metalloproteinase 9 immunoassay for diagnosing inflammation related to dry eye. JAMA Ophthalmol. 2013; 131:24–28.15. Pflugfelder SC, de Paiva CS. The pathophysiology of dry eye disease: what we know and future directions for research. Ophthalmology. 2017; 124:S4–S13.16. Sambursky R, Davitt WF 3rd, Friedberg M, Tauber S. Prospective, multicenter, clinical evaluation of point-of-care matrix metalloproteinase-9 test for confirming dry eye disease. Cornea. 2014; 33:812–818.17. Bron AJ, Evans VE, Smith JA. Grading of corneal and conjunctival staining in the context of other dry eye tests. Cornea. 2003; 22:640–650.18. Miller KL, Walt JG, Mink DR, et al. Minimal clinically important difference for the ocular surface disease index. Arch Ophthalmol. 2010; 128:94–101.19. Kaufman HE. The practical detection of mmp-9 diagnoses ocular surface disease and may help prevent its complications. Cornea. 2013; 32:211–216.20. Park JY, Kim BG, Kim JS, Hwang JH. Matrix metalloproteinase 9 point-of-care immunoassay result predicts response to topical cyclosporine treatment in dry eye disease. Transl Vis Sci Technol. 2018; 7:31.21. Kolaczkowska E, Arnold B, Opdenakker G. Gelatinase B/MMP-9 as an inflammatory marker enzyme in mouse zymosan peritonitis: comparison of phase-specific and cell-specific production by mast cells, macrophages and neutrophils. Immunobiology. 2008; 213:109–124.22. Chotikavanich S, de Paiva CS, Li de Q, et al. Production and activity of matrix metalloproteinase-9 on the ocular surface increase in dysfunctional tear syndrome. Invest Ophthalmol Vis Sci. 2009; 50:3203–3209.23. Starr CE, Gupta PK, Farid M, et al. An algorithm for the preoperative diagnosis and treatment of ocular surface disorders. J Cataract Refract Surg. 2019; 45:669–684.24. Schargus M, Ivanova S, Kakkassery V, et al. Correlation of tear film osmolarity and 2 different MMP-9 tests with common dry eye tests in a cohort of non-dry eye patients. Cornea. 2015; 34:739–744.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparative Evaluation of Matrix Metalloproteinase-9 Immunoassay and Tear Osmolarity Measurement for Diagnosing Severity of Dry Eye Disease
- The Matrix Metalloproteinase-9 Point-of-Care Test for Dry Eye Disease
- Recent treatment of dry eye
- Correlation Analysis between Ocular Surface Parameters with Subjective Symptom Severity in Dry Eye Disease
- The Concentration of Tear Lysozyme in Normal Subjects and Dry Eye