J Korean Foot Ankle Soc.
2019 Dec;23(4):166-172. 10.14193/jkfas.2019.23.4.166.
Surgical Outcomes of the Reinforcing Technique of a Weakened Medial Capsule in Severe Hallux Valgus Using Internal Brace
- Affiliations
-
- 1Department of Orthopedic Surgery, Chungnam National University Hospital, Daejeon, Korea. faschan@daum.net
- 2Da Jeong S.M. Orthopedic Hospital, Sejong, Korea.
- KMID: 2465940
- DOI: http://doi.org/10.14193/jkfas.2019.23.4.166
Abstract
- PURPOSE
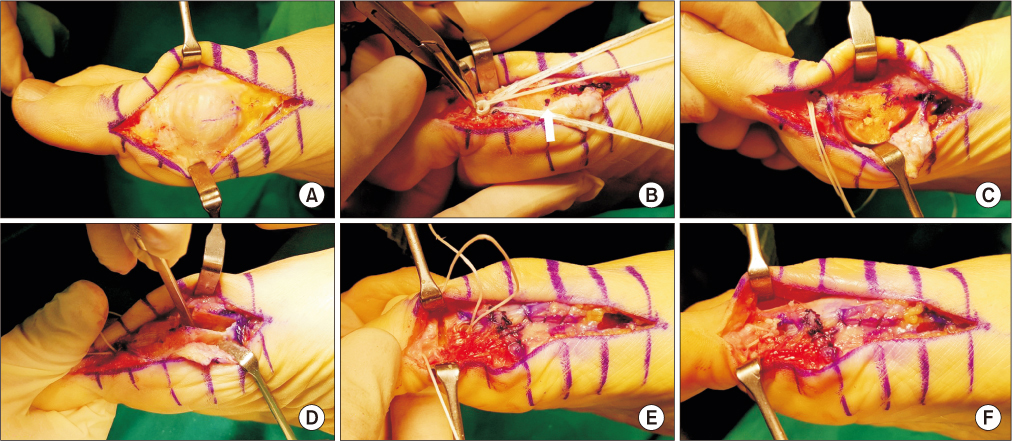
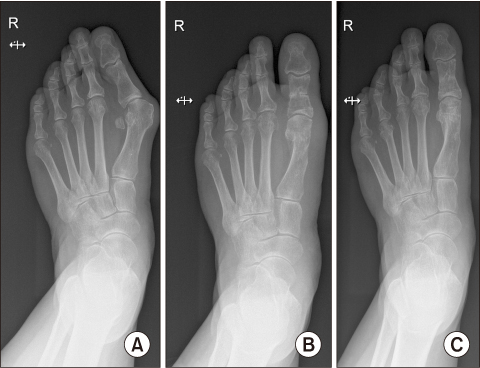
This study evaluated the clinical and radiological results after reinforcement of the weakened medial joint capsule using Internal Brace (Arthrex) for treating severe hallux valgus.
MATERIALS AND METHODS
This study reviewed 56 cases of 50 patients that were followed-up postoperatively for at least 12 months, from September 2017 until August 2018. An extended distal chevron osteotomy combined with a distal soft-tissue release was performed by a single surgeon to treat severe hallux valgus. Internal Brace was applied in 12 cases (group A) who had weakened medial joint capsules, and capsulorrhaphy was performed in 44 cases (group B), and these two groups were compared postoperatively for the clinical and radiological results. The postoperative complications were also investigated.
RESULTS
No significant differences at 1-year follow-up on the Manchester-Oxford Foot Questionnaire and the patients' satisfaction scores were found between the two groups (p=0.905 and p=0.668, respectively). For the radiology, the changes of the values between before surgery and at 1-year follow-up according to the group showed no significant differences in the hallux valgus angle, intermetatarsal angle, and the hallux interphalangeal angle (p=0.986, p=0.516, p=0.754, respectively). Recurrence of hallux valgus was reported in two cases in group A, and in three cases in group B. Transfer metatarsalgia occurred in 4 cases in group B.
CONCLUSION
Based on these results, we recommend the capsule reinforcing technique using Internal Brace as a successful operative option for treating a weakened medial capsule in patients with severe hallux valgus.
Keyword
MeSH Terms
Figure
Reference
-
1. Thomas S, Barrington R. Hallux valgus. Orthopaedics Trauma. 2003; 17:299–307. DOI: 10.1016/S0268-0890(02)00184-6.
Article2. Glasoe WM, Nuckley DJ, Ludewig PM. Hallux valgus and the first metatarsal arch segment: a theoretical biomechanical perspective. Phys Ther. 2010; 90:110–120. DOI: 10.2522/ptj.20080298.
Article3. Chen YJ, Hsu RW, Shih HN, Huang TJ, Hsu KY. Distal chevron osteotomy with intra-articular lateral soft-tissue release for treatment of moderate to severe hallux valgus deformity. J Formos Med Assoc. 1996; 95:776–781.4. Easley ME, Trnka HJ. Current concepts review: hallux valgus part II: operative treatment. Foot Ankle Int. 2007; 28:748–758. DOI: 10.3113/FAI.2007.0748.
Article5. Lui TH, Chan KB. Technical tip: reconstruction of medial collateral ligament in correction of hallux valgus deformity with primary medial collateral ligamentous insufficiency. Foot Ankle Surg. 2012; 18:66–73. DOI: 10.1016/j.fas.2011.01.005.
Article6. Lee JW, Ahn JH, Kim MS, Kim SC. Operative treatment of hallux valgus. J Korean Foot Ankle Soc. 2014; 18:48–55. DOI: 10.14193/jkfas.2014.18.2.48.
Article7. Mahadevan D, Lines S, Hepple S, Winson I, Harries W. Extended plantar limb (modified) chevron osteotomy versus scarf osteotomy for hallux valgus correction: a randomised controlled trial. Foot Ankle Surg. 2016; 22:109–113. DOI: 10.1016/j.fas.2015.05.012.
Article8. Nery C, Barroco R, Réssio C. Biplanar chevron osteotomy. Foot Ankle Int. 2002; 23:792–798.
Article9. Vopat BG, Lareau CR, Johnson J, Reinert SE, DiGiovanni CW. Comparative study of scarf and extended chevron osteotomies for correction of hallux valgus. Foot Ankle Spec. 2013; 6:409–416. DOI: 10.1177/1938640013508431.
Article10. Song JH, Kang C, Hwang DS, Lee GS, Lee SB. Comparison of radiographic and clinical results after extended distal chevron osteotomy with distal soft tissue release with moderate versus severe hallux valgus. Foot Ankle Int. 2019; 40:297–306. DOI: 10.1177/1071100718807893.
Article11. Coughlin MJ. Hallux valgus. J Bone Joint Surg Am. 1996; 78:932–966.12. Schrier JC, Palmen LN, Verheyen CC, Jansen J, Koëter S. Patient-reported outcome measures in hallux valgus surgery. a review of literature. Foot Ankle Surg. 2015; 21:11–15. DOI: 10.1016/j.fas.2014.11.004.
Article13. Dawson J, Coffey J, Doll H, Lavis G, Cooke P, Herron M, et al. A patient-based questionnaire to assess outcomes of foot surgery: validation in the context of surgery for hallux valgus. Qual Life Res. 2006; 15:1211–1222. DOI: 10.1007/s11136-006-0061-5.
Article14. Morley D, Jenkinson C, Doll H, Lavis G, Sharp R, Cooke P, et al. The Manchester-Oxford Foot Questionnaire (MOXFQ): development and validation of a summary index score. Bone Joint Res. 2013; 2:66–69. DOI: 10.1302/2046-3758.24.2000147.15. Park CH, Lee WC. Recurrence of hallux valgus can be predicted from immediate postoperative non-weight-bearing radiographs. J Bone Joint Surg Am. 2017; 99:1190–1197. DOI: 10.2106/JBJS.16.00980.
Article16. Deenik A, van Mameren H, de Visser E, de Waal Malefijt M, Draijer F, de Bie R. Equivalent correction in scarf and chevron osteotomy in moderate and severe hallux valgus: a randomized controlled trial. Foot Ankle Int. 2008; 29:1209–1215. DOI: 10.3113/FAI.2008.1209.
Article17. Lee WC, Kim YM. Correction of hallux valgus using lateral soft-tissue release and proximal Chevron osteotomy through a medial incision. J Bone Joint Surg Am. 2007; 89 Suppl 3:82–89. DOI: 10.2106/JBJS.G.00483.
Article18. Park HW, Lee KB, Chung JY, Kim MS. Comparison of outcomes between proximal and distal chevron osteotomy, both with supplementary lateral soft-tissue release, for severe hallux valgus deformity: a prospective randomised controlled trial. Bone Joint J. 2013; 95-B:510–516. DOI: 10.1302/0301-620X.95B4.30464.19. Sanhudo JA. Extending the indications for distal chevron osteotomy. Foot Ankle Int. 2000; 21:522–523. DOI: 10.1177/107110070002100614.
Article20. Badwey TM, Dutkowsky JP, Graves SC, Richardson EG. An anatomical basis for the degree of displacement of the distal chevron osteotomy in the treatment of hallux valgus. Foot Ankle Int. 1997; 18:213–215. DOI: 10.1177/107110079701800405.
Article21. Edwards WH. Avascular necrosis of the first metatarsal head. Foot Ankle Clin. 2005; 10:117–127. DOI: 10.1016/j.fcl.2004.11.001.
Article22. Robinson AH, Limbers JP. Modern concepts in the treatment of hallux valgus. J Bone Joint Surg Br. 2005; 87:1038–1045. DOI: 10.1302/0301-620X.87B8.16467.
Article23. Schneider W. Distal soft tissue procedure in hallux valgus surgery: biomechanical background and technique. Int Orthop. 2013; 37:1669–1675. DOI: 10.1007/s00264-013-1959-5.
Article24. Uchiyama E, Kitaoka HB, Luo ZP, Grande JP, Kura H, An KN. Pathomechanics of hallux valgus: biomechanical and immunohistochemical study. Foot Ankle Int. 2005; 26:732–738. DOI: 10.1177/107110070502600911.
Article25. Kura H, Luo ZP, Kitaoka HB, An KN. Role of medical capsule and transverse metatarsal ligament in hallux valgus deformity. Clin Orthop Relat Res. 1998; (354):235–240. DOI: 10.1097/00003086-199809000-00028.26. Kempe SA, Singer RH. The modified McBride bunionectomy utilizing the adductor tendon transfer. J Foot Surg. 1985; 24:24–29.27. Mirzayan R, Cooper JD. Chronic medial epicondyle avulsion: technique of fragment excision and ligament reconstruction with internal brace augmentation. J Am Acad Orthop Surg. 2019; 27:e64–e69. DOI: 10.5435/JAAOS-D-17-00446.28. Dabis J, Wilson A. Repair and augmentation with internal brace in the multiligament injured knee. Clin Sports Med. 2019; 38:275–283. DOI: 10.1016/j.csm.2018.11.008.
Article29. Coetzee JC, Ellington JK, Stone R, Ronan J. Retrospective chart review of the internal brace ligament augmentation repair in conjunction with open broström surgery in ankle patients. Foot Ankle Orthop. 2017; 09. 01. DOI: 10.1177/2473011417S000146.
Article30. Schuh R, Benca E, Willegger M, Hirtler L, Zandieh S, Holinka J, et al. Comparison of Broström technique, suture anchor repair, and tape augmentation for reconstruction of the anterior talofibular ligament. Knee Surg Sports Traumatol Arthrosc. 2016; 24:1101–1107. DOI: 10.1007/s00167-015-3631-7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Consideration of Various Medial Capsulorrhaphy Methods in Hallux Valgus Surgery
- Technique Tip: A Simple Method to Treat Hallux Valgus with Severe Metatarsus Adductus
- Corrective Osteotomies in Hallux Valgus
- A Clinical Study of Chevron Osteotomy in Bunion - Hallux Valgus
- Arthrodesis Of The First Metsatarophalangeal Joint For Rheumatoid Arthritis And Hallux Valgus