J Korean Foot Ankle Soc.
2019 Dec;23(4):159-165. 10.14193/jkfas.2019.23.4.159.
Radiographic Risk Factors of Recurrent Hallux Valgus Deformity after Modified Scarf and Akin Osteotomy
- Affiliations
-
- 1Department of Orthopedic Surgery, Dankook University College of Medicine, Cheonan, Korea. m3artist@hanmail.net
- 2Department of Orthopedic Surgery, Armed Forces Capital Hospital, Seongnam, Korea.
- KMID: 2465939
- DOI: http://doi.org/10.14193/jkfas.2019.23.4.159
Abstract
- PURPOSE
This study investigated the recurrence rate after performing hallux valgus correction using scarf and Akin osteotomy, and also identified the correlation and cut-off values of both the preoperative and postoperative radiographic parameters as risk factors for the recurrence of hallux valgus.
MATERIALS AND METHODS
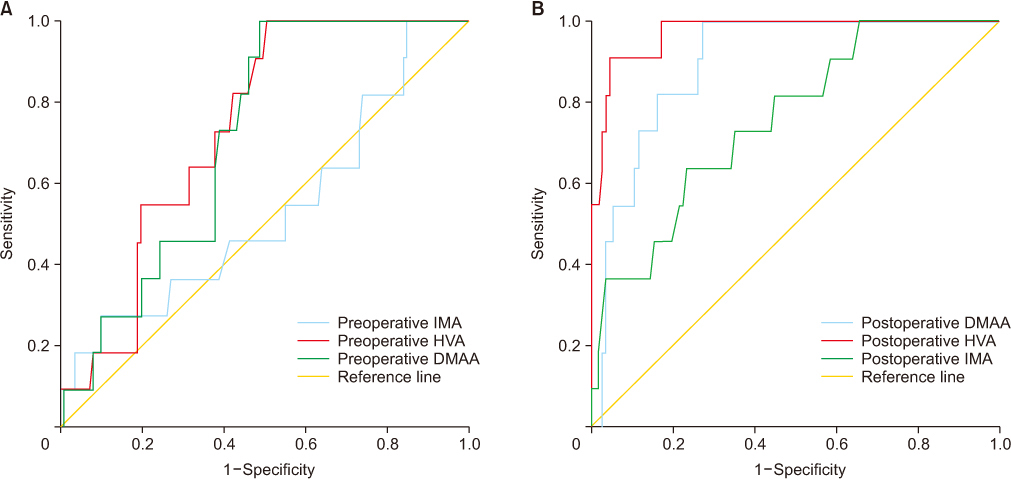
We reviewed 87 hallux valgus patients (122 feet) who received scarf and Akin osteotomy from January 2007 to August 2015. The clinical outcomes were evaluated using the visual analogue scale (VAS) and American Orthopaedic Foot and Ankle Society (AOFAS) scores. The radiological outcome measures included the hallux valgus angle (HVA), intermetatarsal angle (IMA), and distal metatarsal articular angle (DMAA) as determined on the serial weight bearing radiographs. Recurrence was defined as more than 20 degrees of HVA noted on the final follow-up radiograph. Those radiological factors associated with recurrence were evaluated and analyzed.
RESULTS
The mean follow-up duration was 20.6 months (12.0∼46.5 months) and the mean age was 44 years (13∼80 years). The VAS and AOFAS scores were significantly improved at the time of the final follow-up (7.0 to 2.0, p<0.001; 78.0 to 92.0, p<0.001; respectively). Significant corrections in the HVA, IMA, and DMAA were obtained (p<0.001). Eleven (9.0%: 11/122) cases experienced recurrent hallux valgus deformity. The postoperative IMA, DMAA and HVA showed significant moderate to strong correlation with HVA at the final follow-up (Pearson correlation coefficient: 0.44, 0.70, and 0.88, respectively; p<0.001). Postoperative HVA>16.7 degrees, postoperative DMAA>13.9 degrees, and postoperative IMA>8.2 degrees showed statistically significant correlation with radiological recurrence at the last follow-up, and the odds ratio of each variable was high in order.
CONCLUSION
Our radiographic results indicated that postoperative HVA>16.7 degrees, postoperative DMAA>13.9 degrees, and postoperative IMA>8.2 degrees can be risk factors for hallux valgus recurrence. These risk factors may be helpful for modifying surgical procedures and preventing the recurrence of hallux valgus.
Keyword
MeSH Terms
Figure
Reference
-
1. Garrido IM, Rubio ER, Bosch MN, González MS, Paz GB, Llabrés AJ. Scarf and akin osteotomies for moderate and severe hallux valgus: clinical and radiographic results. Foot Ankle Surg. 2008; 14:194–203. DOI: 10.1016/j.fas.2008.02.003.2. Molloy A, Widnall J. Scarf osteotomy. Foot Ankle Clin. 2014; 19:165–180. DOI: 10.1016/j.fcl.2014.02.001.
Article3. Okuda R, Kinoshita M, Yasuda T, Jotoku T, Shima H, Takamura M. Hallux valgus angle as a predictor of recurrence following proximal metatarsal osteotomy. J Orthop Sci. 2011; 16:760–764. DOI: 10.1007/s00776-011-0136-1.
Article4. Raikin SM, Miller AG, Daniel J. Recurrence of hallux valgus: a review. Foot Ankle Clin. 2014; 19:259–274. DOI: 10.1016/j.fcl.2014.02.008.5. Shibuya N, Kyprios EM, Panchani PN, Martin LR, Thorud JC, Jupiter DC. Factors associated with early loss of hallux valgus correction. J Foot Ankle Surg. 2018; 57:236–240. DOI: 10.1053/j.jfas.2017.08.018.
Article6. Okuda R, Kinoshita M, Yasuda T, Jotoku T, Kitano N, Shima H. The shape of the lateral edge of the first metatarsal head as a risk factor for recurrence of hallux valgus. J Bone Joint Surg Am. 2007; 89:2163–2172. DOI: 10.2106/JBJS.F.01455.
Article7. Okuda R, Kinoshita M, Yasuda T, Jotoku T, Kitano N, Shima H. Postoperative incomplete reduction of the sesamoids as a risk factor for recurrence of hallux valgus. J Bone Joint Surg Am. 2009; 91:1637–1645. DOI: 10.2106/JBJS.H.00796.
Article8. Park CH, Lee DY. Change of reliability for distal metatarsal articular angle measurement before and after proximal chevron osteotomy. J Korean Foot Ankle Soc. 2016; 20:145–151. DOI: 10.14193/jkfas.2016.20.4.145.
Article9. Aiyer A, Shub J, Shariff R, Ying L, Myerson M. Radiographic recurrence of deformity after hallux valgus surgery in patients with metatarsus adductus. Foot Ankle Int. 2016; 37:165–171. DOI: 10.1177/1071100715608372.
Article10. Bock P, Kluger R, Kristen KH, Mittlböck M, Schuh R, Trnka HJ. The scarf osteotomy with minimally invasive lateral release for treatment of hallux valgus deformity: intermediate and long-term results. J Bone Joint Surg Am. 2015; 97:1238–1245. DOI: 10.2106/JBJS.N.00971.
Article11. Li X, Guo M, Zhu Y, Xu X. The excessive length of first ray as a risk factor for hallux valgus recurrence. PLoS One. 2018; 13:e0205560. DOI: 10.1371/journal.pone.0205560.
Article12. Park HW, Kim SJ. Treatment results of hallux valgus deformity by parallel-shaped modified scarf osteotomy. J Korean Foot Ankle Soc. 2012; 16:123–127.13. Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979; 86:420–428. DOI: 10.1037/0033-2909.86.2.420.
Article14. Rosner B. Study guide for fundamentals of biostatistics. 5th ed. Australia: Duxbury;2000.15. Muller MP, Tomlinson G, Marrie TJ, Tang P, McGeer A, Low DE, et al. Can routine laboratory tests discriminate between severe acute respiratory syndrome and other causes of community-acquired pneumonia? Clin Infect Dis. 2005; 40:1079–1086. DOI: 10.1086/428577.
Article16. Lee DW, Lee HS, You JS, Park YS, Chung SP. Validation of the glasgow-blatchford score and the pre-endoscopic rockall score for predicting active gastrointestinal bleeding in emergency department patients with suspected upper gastrointestinal bleeding. J Korean Soc Emerg Med. 2014; 25:645–652.17. Dancey CP, Reidy J. Statistics without maths for psychology. 5th ed. Harlow: Prentice Hall/Pearson education;2011.18. Coetzee JC, Resig SG, Kuskowski M, Saleh KJ. The Lapidus procedure as salvage after failed surgical treatment of hallux valgus. Surgical technique. J Bone Joint Surg Am. 2004; 86-A Suppl 1:30–36. DOI: 10.2106/00004623-200403001-00005.19. Park CH, Lee WC. Is double metatarsal osteotomy superior to proximal chevron osteotomy in treatment of hallux valgus with increased distal metatarsal articular angle? J Foot Ankle Surg. 2018; 57:241–246. DOI: 10.1053/j.jfas.2017.08.020.
Article20. Smith BW, Coughlin MJ. Treatment of hallux valgus with increased distal metatarsal articular angle: use of double and triple osteotomies. Foot Ankle Clin. 2009; 14:369–382. DOI: 10.1016/j.fcl.2009.03.005.
Article21. Lee KT, Cha SD, Young KW, Kim JY, Joh JW. The results of triple osteotomy in adult hallux valgus patients with highly increased distal metatarsal articular angle. J Korean Foot Ankle Soc. 2007; 11:28–34.22. Moon GH, Ahn GY, Yun HH, Lee YH, Lee JI, Nam IH. Multi-dimentional correction of the scarf osteotomy for the treatment of hallux valgus. J Korean Foot Ankle Soc. 2007; 11:23–27.23. Park CH, Lee WC, Kim JR, Lim SW. Characteristics of severe hallux valgus deformity with moderate intermetatarsal angle. J Korean Foot Ankle Soc. 2014; 18:173–177. DOI: 10.14193/jkfas.2014.18.4.173.
Article24. Rosner B. Fundamentals of biostatistics. 7th ed. Boston: Brooks/Cole, Cengage Learning;2011.25. Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982; 143:29–36. DOI: 10.1148/radiology.143.1.7063747.
Article26. Coughlin MJ, Freund E, Roger A. Mann Award. The reliability of angular measurements in hallux valgus deformities. Foot Ankle Int. 2001; 22:369–379. DOI: 10.1177/107110070102200503.27. Shima H, Okuda R, Yasuda T, Jotoku T, Kitano N, Kinoshita M. Radiographic measurements in patients with hallux valgus before and after proximal crescentic osteotomy. J Bone Joint Surg Am. 2009; 91:1369–1376. DOI: 10.2106/JBJS.H.00483.
Article28. Jastifer JR, Coughlin MJ, Schutt S, Hirose C, Kennedy M, Grebing B, et al. Comparison of radiographic and anatomic distal metatarsal articular angle in cadaver feet. Foot Ankle Int. 2014; 35:389–393. DOI: 10.1177/1071100714522027.
Article29. Robinson AH, Cullen NP, Chhaya NC, Sri-Ram K, Lynch A. Variation of the distal metatarsal articular angle with axial rotation and inclination of the first metatarsal. Foot Ankle Int. 2006; 27:1036–1040. DOI: 10.1177/107110070602701207.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment Results of Hallux Valgus Deformity by Parallel-Shaped Modified Scarf Osteotomy
- The Effect of Derotational Closing Wedge Akin Osteotomy for the Treatment of Hallux Valgus with the Pronation of Great Toe
- Minimally Invasive Distal Transverse Metatarsal Osteotomy – Akin Osteotomy (MITA) for Recurrent Hallux Valgus: A Report of Four Cases
- Modified Proximal Scarf Osteotomy for Hallux Valgus
- Short Scarf Osteotomy for Moderate Hallux Valgus