J Korean Foot Ankle Soc.
2019 Dec;23(4):143-148. 10.14193/jkfas.2019.23.4.143.
Approach for the Treatment on Hallux Valgus
- Affiliations
-
- 1Department of Orthopedic Surgery, Wonkwang University Hospital, School of Medicine, Wonkwang University, Iksan, Korea. kensin06@hanmail.net
- KMID: 2465936
- DOI: http://doi.org/10.14193/jkfas.2019.23.4.143
Abstract
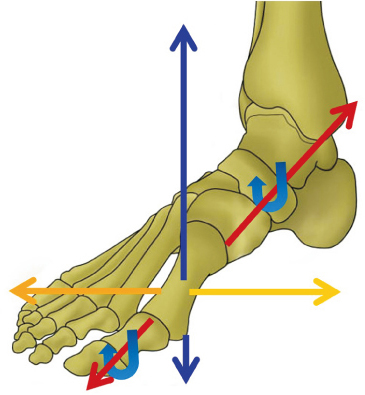
- Although many patients who undergo bunion repair do well and have satisfactory results, a critical evaluation of these results shows the potential for improvement. Metatarsal deformity of the hallux valgus is a 3-dimensional deformity, including rotation in the coronal plane. Theoretically, it is important to understand the 3-dimensional displacement of the first metatarsal for correcting the deformities of valgus rotation in the frontal plane. Yet the current methods of metatarsal osteotomy principally attempt to correct the deformity in the transverse plane. The modified technique for the Lapidus procedure can be used in a variety of hallux valgus conditions and severities, and the early results suggest that a powerful correction can be maintained. In addition, efforts have been made to correct the 3-dimensional deformity by performing metatarsal shaft osteotomy. In the case of degenerative arthritis, first metatarsophalangeal joint arthrodesis is a good option to correct the 3-dimensional deformation. Correction of the 3-dimensional deformity, including a rotational deformity in the frontal plane of the metatarsals, should be considered when selecting surgical treatment and is essential for achieving a good prognosis for patients with hallux valgus. This article reviews the classification and treatment of hallux valgus for correction of the 3-dimensional deformity.
Keyword
MeSH Terms
Figure
Reference
-
1. Coughlin MJ, Saltzman CL, Anderson RB, Mann RA. Mann's surgery of the foot and ankle. 9th ed. Philadelphia: Saunders Elsevier;2014. p. 199–300.2. Menz HB, Lord SR. Gait instability in older people with hallux valgus. Foot Ankle Int. 2005; 26:483–489. DOI: 10.1177/107110070502600610.
Article3. Coughlin MJ, Jones CP. Hallux valgus: demographics, etiology, and radiographic assessment. Foot Ankle Int. 2007; 28:759–777. DOI: 10.3113/FAI.2007.0759.
Article4. Jang KS, Kim TW, Kim HJ. Diagnosis and pathophysiology of hallux valgus. J Korean Foot Ankle Soc. 2014; 18:43–47. DOI: 10.14193/jkfas.2014.18.2.43.
Article5. Hatch DJ, Santrock RD, Smith B, Dayton P, Weil L Jr. Triplane hallux abducto valgus classification. J Foot Ankle Surg. 2018; 57:972–981. DOI: 10.1053/j.jfas.2018.02.008.
Article6. Ko KR, Sung KS. Corrective osteotomies in hallux valgus. J Korean Foot Ankle Soc. 2017; 21:43–49. DOI: 10.14193/jkfas.2017.21.2.43.
Article7. Bednarz PA, Manoli A 2nd. Modified lapidus procedure for the treatment of hypermobile hallux valgus. Foot Ankle Int. 2000; 21:816–821. DOI: 10.1177/107110070002101004.
Article8. Kim JY, Park JS, Hwang SK, Young KW, Sung IH. Mobility changes of the first ray after hallux valgus surgery: clinical results after proximal metatarsal chevron osteotomy and distal soft tissue procedure. Foot Ankle Int. 2008; 29:468–472. DOI: 10.3113/FAI.2008.0468.
Article9. Coughlin MJ, Jones CP. Hallux valgus and first ray mobility. A prospective study. J Bone Joint Surg Am. 2007; 89:1887–1898. DOI: 10.2106/JBJS.F.01139.10. Coughlin MJ, Shurnas PS. Hallux valgus in men. Part II: first ray mobility after bunionectomy and factors associated with hallux valgus deformity. Foot Ankle Int. 2003; 24:73–78. DOI: 10.1177/107110070302400112.
Article11. Coughlin MJ, Freund E. Roger A. Mann Award. The reliability of angular measurements in hallux valgus deformities. Foot Ankle Int. 2001; 22:369–379. DOI: 10.1177/107110070102200503.12. Bock P, Kluger R, Kristen KH, Mittlböck M, Schuh R, Trnka HJ. The scarf osteotomy with minimally invasive lateral release for treatment of hallux valgus deformity: intermediate and long-term results. J Bone Joint Surg Am. 2015; 97:1238–1245. DOI: 10.2106/JBJS.N.00971.
Article13. Chong A, Nazarian N, Chandrananth J, Tacey M, Shepherd D, Tran P. Surgery for the correction of hallux valgus: minimum five-year results with a validated patient-reported outcome tool and regression analysis. Bone Joint J. 2015; 97-B:208–214. DOI: 10.1302/0301-620X.97B2.34891.14. Jeuken RM, Schotanus MG, Kort NP, Deenik A, Jong B, Hendrickx RP. Long-term follow-up of a randomized controlled trial comparing scarf to chevron osteotomy in hallux valgus correction. Foot Ankle Int. 2016; 37:687–695. DOI: 10.1177/1071100716639574.
Article15. Iyer S, Demetracopoulos CA, Sofka CM, Ellis SJ. High rate of recurrence following proximal medial opening wedge osteotomy for correction of moderate hallux valgus. Foot Ankle Int. 2015; 36:756–763. DOI: 10.1177/1071100715577195.
Article16. Okuda R, Kinoshita M, Yasuda T, Jotoku T, Kitano N, Shima H. Postoperative incomplete reduction of the sesamoids as a risk factor for recurrence of hallux valgus. J Bone Joint Surg Am. 2009; 91:1637–1645. DOI: 10.2106/JBJS.H.00796.
Article17. Okuda R, Kinoshita M, Yasuda T, Jotoku T, Kitano N, Shima H. The shape of the lateral edge of the first metatarsal head as a risk factor for recurrence of hallux valgus. J Bone Joint Surg Am. 2007; 89:2163–2172. DOI: 10.2106/JBJS.F.01455.
Article18. Yasuda T, Okuda R, Jotoku T, Shima H, Hida T, Neo M. Proximal supination osteotomy of the first metatarsal for hallux valgus. Foot Ankle Int. 2015; 36:696–704. DOI: 10.1177/1071100715572188.
Article19. Scranton PE Jr, Rutkowski R. Anatomic variations in the first ray: Part I. Anatomic aspects related to bunion surgery. Clin Orthop Relat Res. 1980; (151):244–255.20. Kim Y, Kim JS, Young KW, Naraghi R, Cho HK, Lee SY. A new measure of tibial sesamoid position in hallux valgus in relation to the coronal rotation of the first metatarsal in CT scans. Foot Ankle Int. 2015; 36:944–952. DOI: 10.1177/1071100715576994.
Article21. Dayton P, Kauwe M, Feilmeier M. Clarification of the anatomic definition of the bunion deformity. J Foot Ankle Surg. 2014; 53:160–163. DOI: 10.1053/j.jfas.2013.10.007.
Article22. Dayton P, Feilmeier M, Kauwe M, Hirschi J. Relationship of frontal plane rotation of first metatarsal to proximal articular set angle and hallux alignment in patients undergoing tarsometatarsal arthrodesis for hallux abducto valgus: a case series and critical review of the literature. J Foot Ankle Surg. 2013; 52:348–354. DOI: 10.1053/j.jfas.2013.01.006.
Article23. DiDomenico LA, Fahim R, Rollandini J, Thomas ZM. Correction of frontal plane rotation of sesamoid apparatus during the Lapidus procedure: a novel approach. J Foot Ankle Surg. 2014; 53:248–251. DOI: 10.1053/j.jfas.2013.12.002.
Article24. Robinson AH, Cullen NP, Chhaya NC, Sri-Ram K, Lynch A. Variation of the distal metatarsal articular angle with axial rotation and inclination of the first metatarsal. Foot Ankle Int. 2006; 27:1036–1040. DOI: 10.1177/107110070602701207.
Article25. Yi Y, Lee WC. Comparison of three-dimensional displacement among different metatarsal osteotomies. Foot Ankle Clin. 2018; 23:193–203. DOI: 10.1016/j.fcl.2018.01.004.
Article26. Wagner P, Wagner E. Is the rotational deformity important in our decision-making process for correction of hallux valgus deformity? Foot Ankle Clin. 2018; 23:205–217. DOI: 10.1016/j.fcl.2018.01.009.
Article27. Swanton E, Mason L, Molloy A. How do i use the scarf osteotomy to rotate the metatarsal and correct the deformity in three dimensions? Foot Ankle Clin. 2018; 23:239–246. DOI: 10.1016/j.fcl.2018.01.008.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Incidence of Hallux Valgus Interphalangeus in the Normal and Hallux Valgus Feet and its Correlations with Hallux Valgus Angle and Intermetatarsal Angle
- Consideration of Various Medial Capsulorrhaphy Methods in Hallux Valgus Surgery
- Corrective Osteotomies in Hallux Valgus
- Technique Tip: A Simple Method to Treat Hallux Valgus with Severe Metatarsus Adductus
- A clinical analysis of the operative treatment in hallux valgus