J Surg Ultrasound.
2019 May;6(1):8-13. 10.0000/jsu.2019.6.1.8.
What Is a Practical Catheter Vein Ratio to Lower the Incidence of PICC-Related Symptomatic Thrombosis?
- Affiliations
-
- 1Department of Surgery, Inje University Seoul Paik Hospital, Seoul, Korea. omarch@paik.ac.kr
- KMID: 2465875
- DOI: http://doi.org/10.0000/jsu.2019.6.1.8
Abstract
- PURPOSE
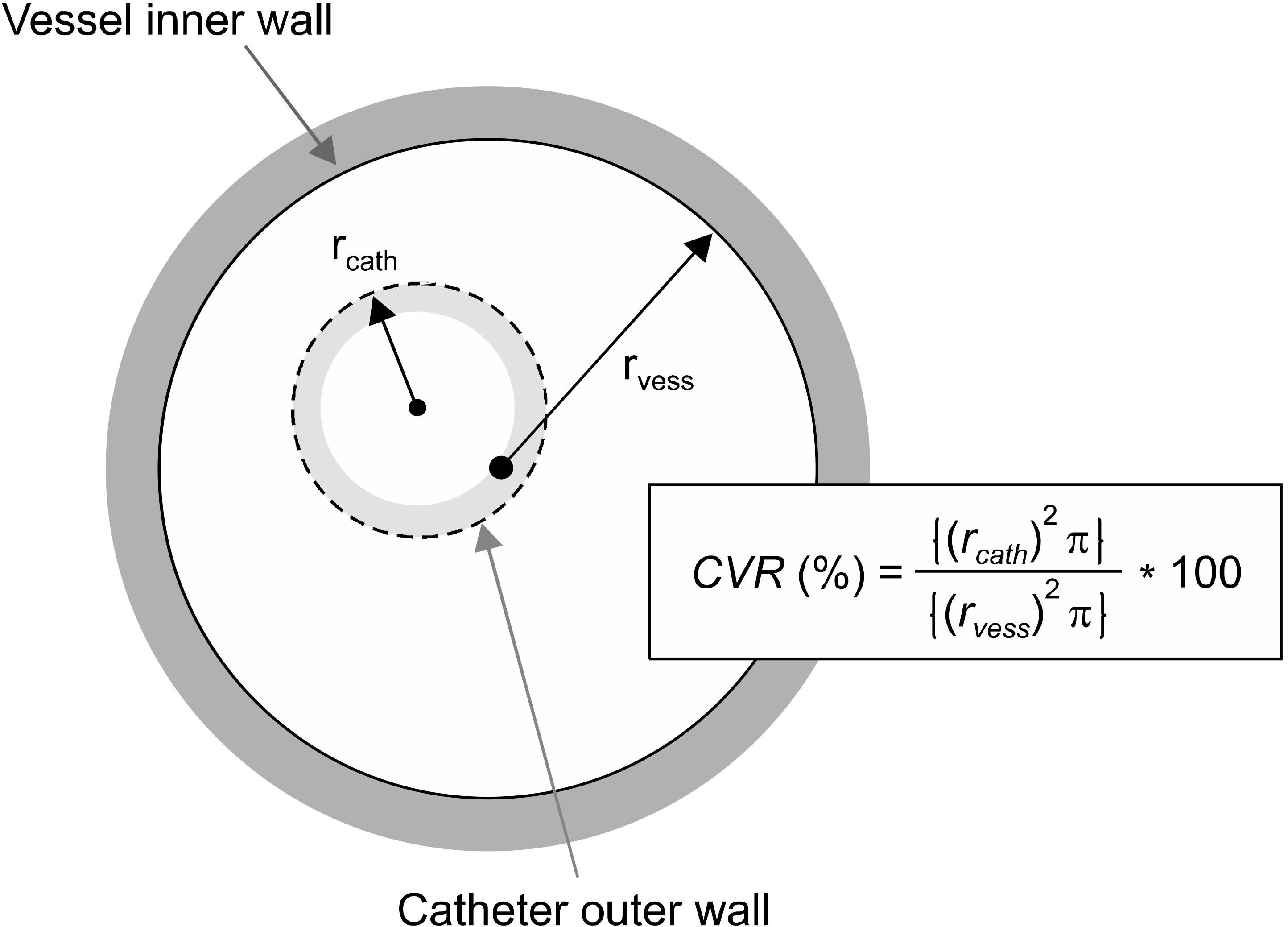
The catheter vein ratio (CVR) is one of control factors related to the incidence of catheter related thrombosis (CRT). This paper reports a practical CVR to reduce the incidence of CRT in patients receiving PICC.
METHODS
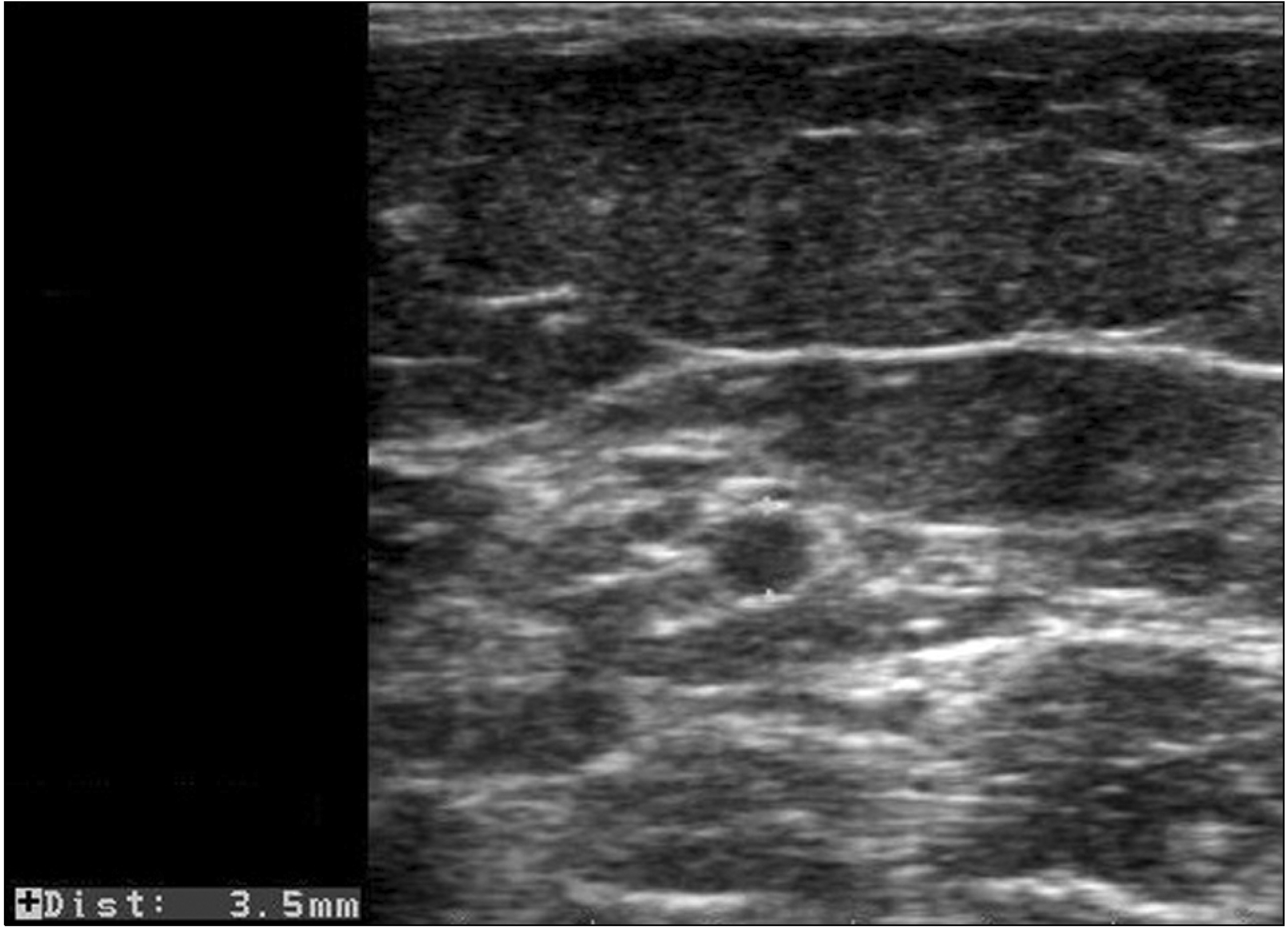
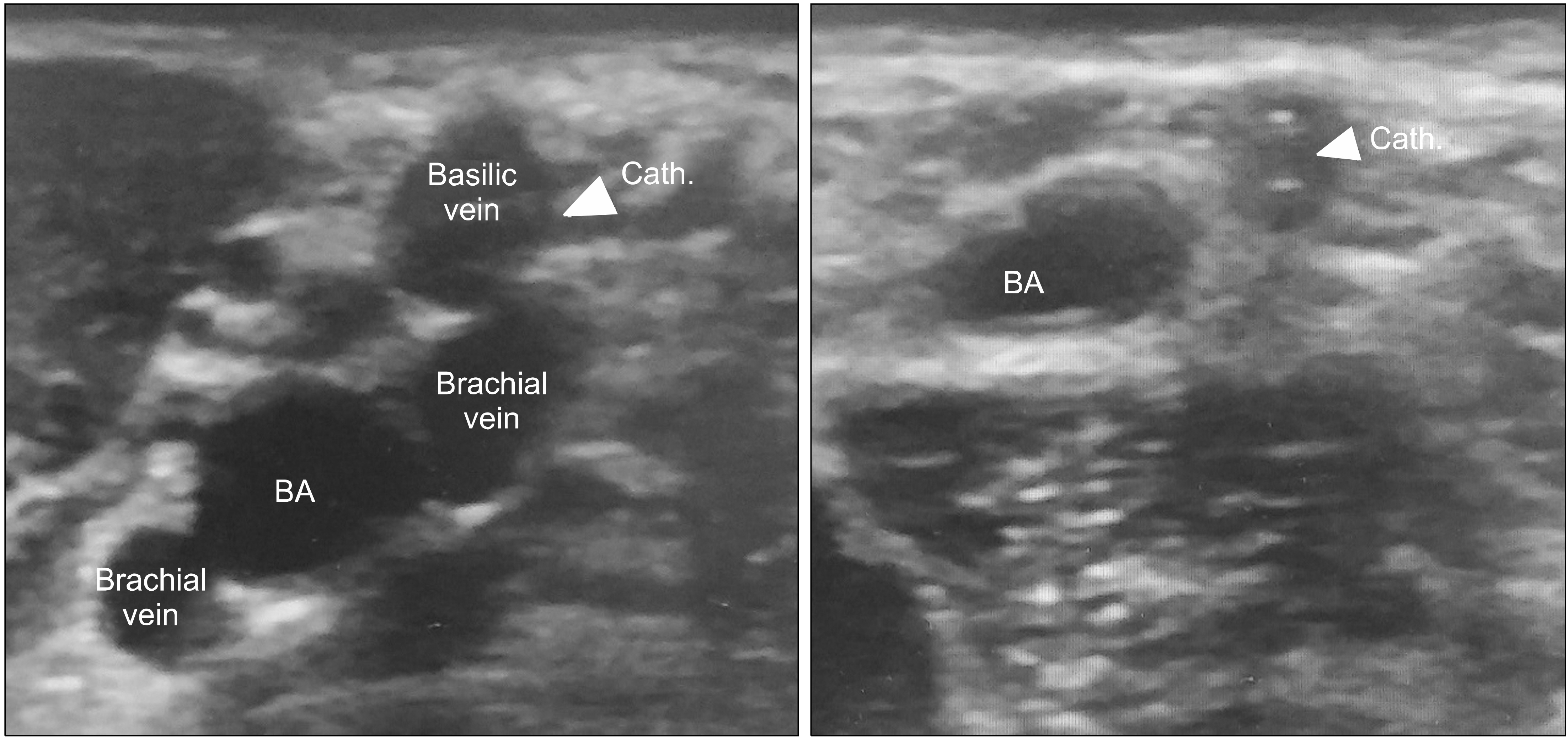
Information on patients with PICC insertion between January 2018 and December 2018 was extracted retrospectively from a single center. The information was composed of age, sex, BMI, access locations, comorbidities, catheter sizes, catheter days, catheter removal cause, and CRT. The incidence of CRT and other factors were analyzed.
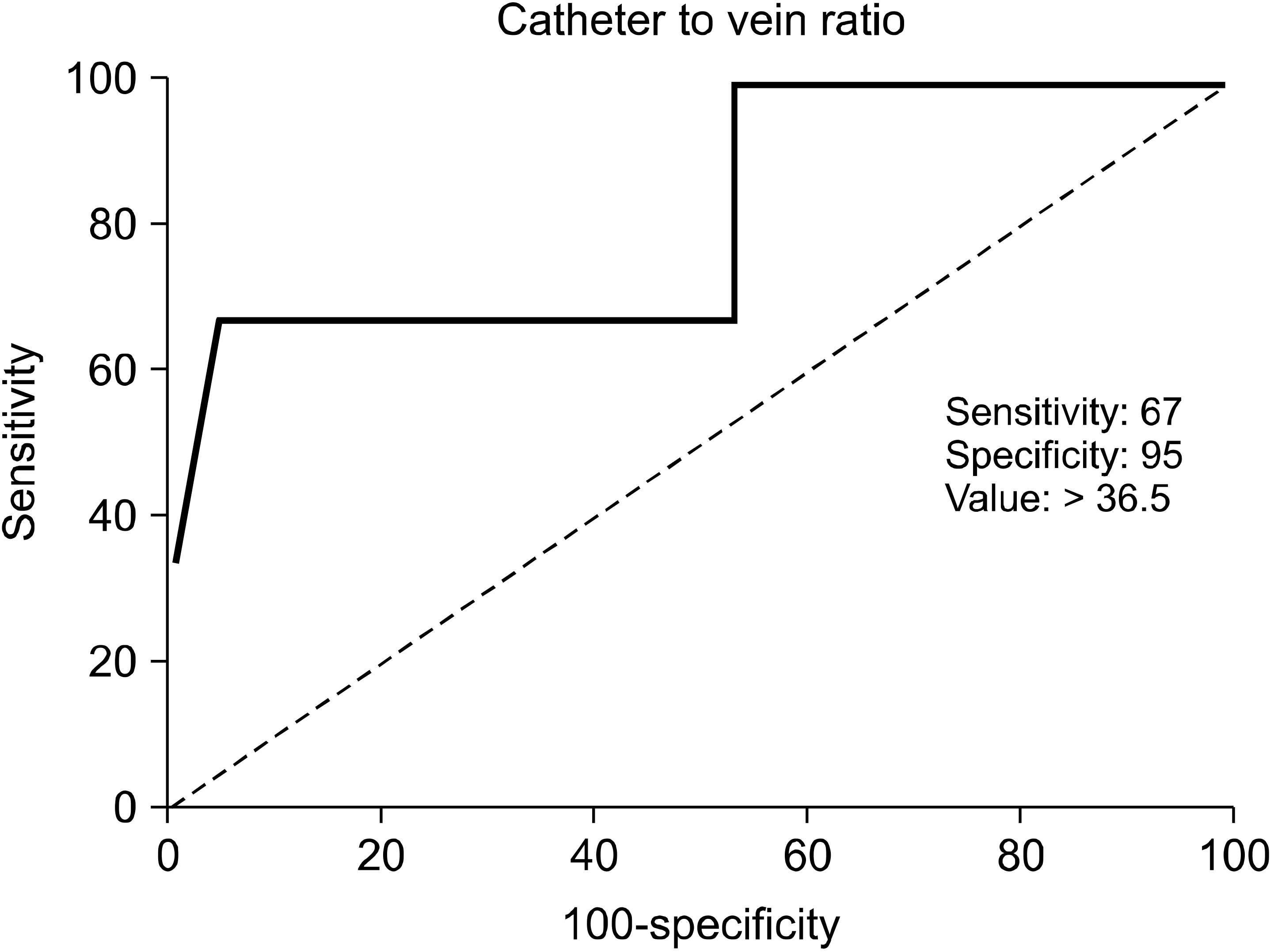
RESULTS
Of the 164 patients who underwent PICC and 2,697 catheter days in the study, three patients (1.8%) experienced a symptomatic thrombosis. Without significance to other factors, the incidence of thrombosis was relevant only in those with higher CVR vs. those with lower CVR (P = 0.047). In addition, its cut-off value was 36.5% (AUC 0.813, 95% CI: 1.003-1.495). Compared to the higher and lower than 36.5% CVR, the odd ratio was 38.25 in the group with a higher than 36.5% CVR (95% CI: 3.129-467.611, P = 0.010).
CONCLUSION
CVR is one of the factors that can be controlled to reduce the clinical relevance of CRT. A lower than 36.5% CVR should be maintained to be in the safety zone from PICC related thrombosis.
Keyword
MeSH Terms
Figure
Reference
-
Loughran SC., Borzatta M. 1995. Peripherally inserted central catheters: a report of 2506 catheter days. JPEN J Parenter Enteral Nutr. 19:133–6. DOI: 10.1177/0148607195019002133. PMID: 7609278.
ArticleNg PK., Ault MJ., Maldonado LS. 1996. Peripherally inserted central catheters in the intensive care unit. J Intensive Care Med. 11:49–54. DOI: 10.1177/088506669601100107. PMID: 10160070.
ArticleFallouh N., McGuirk HM., Flanders SA., Chopra V. 2015. Peripherally inserted central catheter-associated deep vein thrombosis: a narrative review. Am J Med. 128:722–38. DOI: 10.1016/j.amjmed.2015.01.027. PMID: 25697969.
ArticleChopra V., Anand S., Hickner A., Buist M., Rogers MA., Saint S, et al. 2013. Risk of venous thromboembolism associated with peripherally inserted central catheters: a systematic review and meta-analysis. Lancet. 382:311–25. DOI: 10.1016/S0140-6736(13)60592-9. PMID: 23697825.
ArticleLamperti M., Bodenham AR., Pittiruti M., Blaivas M., Augoustides JG., Elbarbary M, et al. 2012. International evidence-based recommendations on ultrasound-guided vascular access. Intensive Care Med. 38:1105–17. DOI: 10.1007/s00134-012-2597-x. PMID: 22614241.
ArticleNifong TP., McDevitt TJ. 2011. The effect of catheter to vein ratio on blood flow rates in a simulated model of peripherally inserted central venous catheters. Chest. 140:48–53. DOI: 10.1378/chest.10-2637. PMID: 21349931.
ArticleSharp R., Cummings M., Fielder A., Mikocka-Walus A., Grech C., Esterman A. 2015. The catheter to vein ratio and rates of symptomatic venous thromboembolism in patients with a peripherally inserted central catheter (PICC): a prospective cohort study. Int J Nurs Stud. 52:677–85. DOI: 10.1016/j.ijnurstu.2014.12.002. PMID: 25593110.
ArticleSpencer TR., Mahoney KJ. 2017. Reducing catheter-related thrombosis using a risk reduction tool centered on catheter to vessel ratio. J Thromb Thrombolysis. 44:427–34. DOI: 10.1007/s11239-017-1569-y. PMID: 29022210.
ArticlePernar LI., Wolf LL., Seshadri A., Patel V. 2016. Impact of a surgeon-led peripherally inserted central venous catheter team on peripherally inserted central venous catheter-related complications and costs. Surg Infect (Larchmt). 17:352–6. DOI: 10.1089/sur.2015.093. PMID: 26900912.
ArticleChopra V., Kaatz S., Grant P., Swaminathan L., Boldenow T., Conlon A, et al. 2018. Risk of venous thromboembolism following peripherally inserted central catheter exchange: an analysis of 23,000 hospitalized patients. Am J Med. 131:651–60. DOI: 10.1016/j.amjmed.2018.01.017. PMID: 29408616.
ArticleSriskandarajah P., Webb K., Chisholm D., Raobaikady R., Davis K., Pepper N, et al. 2015. Retrospective cohort analysis comparing the incidence of deep vein thromboses between peripherally-inserted and long-term skin tunneled venous catheters in hemato-oncology patients. Thromb J. 13:21. DOI: 10.1186/s12959-015-0052-2. PMID: 26113804. PMCID: PMC4480444.
ArticleWall C., Moore J., Thachil J. 2016. Catheter-related thrombosis: apractical approach. J Intensive Care Soc. 17:160–7. DOI: 10.1177/1751143715618683. PMID: 28979481. PMCID: PMC5606399.Sharp R., Cummings M., Childs J., Fielder A., Mikocka-Walus A., Grech C, et al. 2015. Measurement of vein diameter for peripherally inserted central catheter (PICC) insertion: an observational study. J Infus Nurs. 38:351–7. DOI: 10.1097/NAN.0000000000000125. PMID: 26339941.Stokowski G., Steele D., Wilson D. 2009. The use of ultrasound to improve practice and reduce complication rates in peripherally inserted central catheter insertions: final report of investigation. J Infus Nurs. 32:145–55. DOI: 10.1097/NAN.0b013e3181a1a98f. PMID: 19444022.Clemence BJ., Maneval RE. 2014. Risk factors associated with catheter-related upper extremity deep vein thrombosis in patients with peripherally inserted central venous catheters: literature review: part 1. J Infus Nurs. 37:187–96. DOI: 10.1097/NAN.0000000000000037. PMID: 24694512.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Safety and Feasibility of Ultrasound-guided Peripherally Inserted Central Catheterization for Chemo-Delivery
- The Incidence of Deep Vein Thrombosis in the Lower Extremity
- Outcome of Tunneled Infusion Catheters Inserted via the Right Internal Jugular Vein
- Removal of a Peripherally Inserted Central Catheter Remnant using Cardiac Catheterization in Preterm Infant
- Safety and Efficacy of Peripherally Inserted Central Catheter Placement by Surgical Intensivist–Led Vascular Access Team