Anesth Pain Med.
2019 Oct;14(4):449-455. 10.17085/apm.2019.14.4.449.
Effects of intubation with a double-lumen endotracheal tube on intraocular pressure during rapid sequence induction using succinylcholine chloride in patients with or without underlying systemic hypertension
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 2Department of Anesthesiology and Pain Medicine, Uijeongbu St. Mary's Hospital, The Catholic University of Korea, College of Medicine, Uijeongbu, Korea. jmlee@catholic.ac.kr
- KMID: 2465344
- DOI: http://doi.org/10.17085/apm.2019.14.4.449
Abstract
- BACKGROUND
Tracheal intubation is closely associated with increases in intraocular pressure (IOP); however, the effects of double-lumen tube (DLT) intubation on IOP have not been validated. Systemic hypertension (HTN) is another factor that may increase IOP. In this study, we observed differences in IOP increases between DLT and single-lumen tube (SLT) intubation, and evaluated the influence of underlying HTN during rapid sequence induction.
METHODS
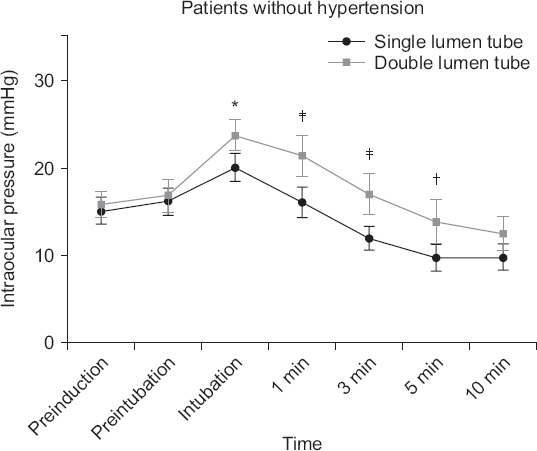
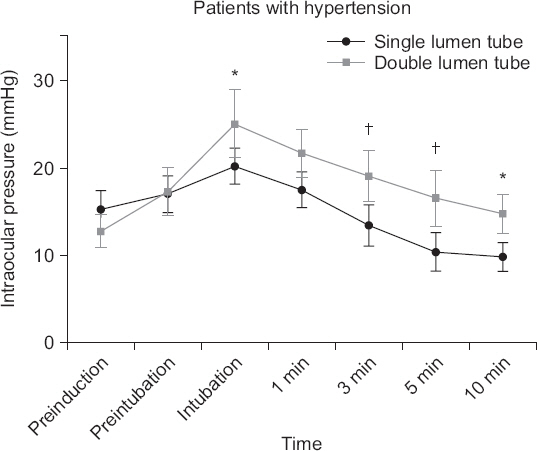
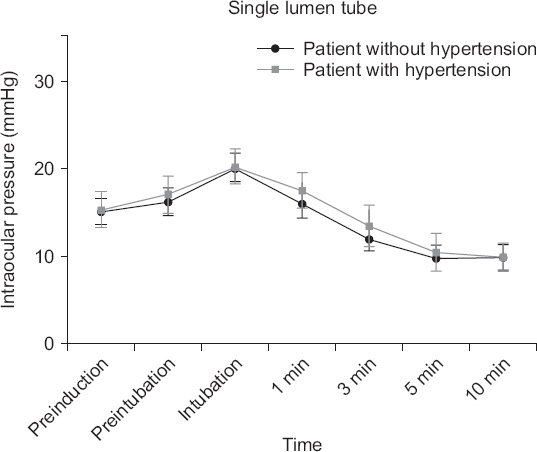
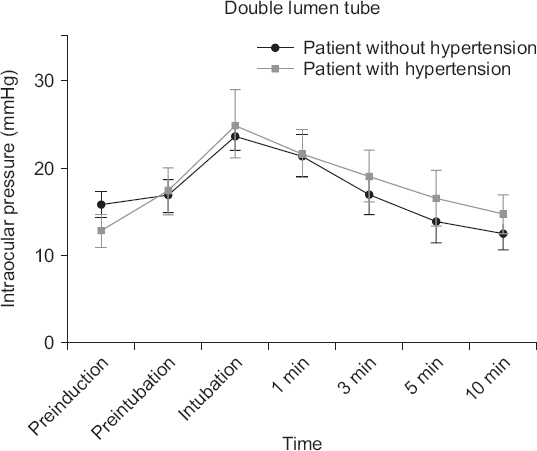
Sixty-eight patients were allocated into one of the following group: SLT/without HTN (n = 17), SLT/HTN (n = 17), DLT/without HTN (n = 17), and DLT/HTN (n = 17). An SLT was inserted for orthopedic or gynecological surgery, and a DLT was inserted for lung surgery after rapid sequence induction using succinylcholine. IOP was measured before anesthetic induction and until 10 min after intubation using a handheld tonometer (Tono-Pen AVIA®).
RESULTS
In the DLT/without HTN and DLT/HTN groups, the maximum increases in IOPs after tracheal intubation were 7.9 and 12.2 mmHg, respectively, compared to baseline. In the SLT/without HTN and SLT/HTN groups, the maximum increases were 5.0 and 4.9 mmHg, respectively, compared to baseline. In comparisons between patients with and without underlying HTN, the values of IOPs were comparable.
CONCLUSIONS
Tracheal intubation with a DLT is associated with more increases in IOPs than with an SLT in rapid sequence induction. Well-controlled underlying hypertension did not increase IOP during tracheal intubation.
MeSH Terms
Figure
Reference
-
1. Lamb K, James MF, Janicki PK. The laryngeal mask airway for intraocular surgery:effects on intraocular pressure and stress responses. Br J Anaesth. 1992; 69:143–7. DOI: 10.1093/bja/69.2.143. PMID: 1309179.2. Hamp T, Stumpner T, Grubhofer G, Ruetzler K, Thell R, Hager H. Haemodynamic response at double lumen bronchial tube placement Airtraq vs MacIntosh laryngoscope, a randomised controlled trial. Heart Lung Vessel. 2015; 7:54–63. PMID: 25861591. PMCID: PMC4381823.3. Mizrak A, Kocamer B, Deniz H, Yendi F, Oner U. Cardiovasular changes after placement of a classic endotracheal tube, doublelumen tube, and Laryngeal Mask Airway. J Clin Anesth. 2011; 23:616–20. DOI: 10.1016/j.jclinane.2011.03.005. PMID: 22137512.4. Vaajanen A, Mervaala E, Oksala O, Vapaatalo H. Is there a relationship between blood pressure and intraocular pressure?An experimental study in hypertensive rats. Curr Eye Res. 2008; 33:325–32. DOI: 10.1080/02713680802011679. PMID: 18398707.5. Beneyto P, Barajas MA, Garcia-de-Blas F, Del Cura I, Sanz T, Vello R, et al. Predictive value of tonometry with Tono-pen XL in primary care. Br J Gen Pract. 2007; 57:653–4. PMID: 17688761. PMCID: PMC2099672.6. Tuzcu K, Tuzcu EA, Karcioglu M, Davarci I, Coskun M, Ilhan O, et al. The effects of remifentanil and esmolol on increase in intraocular pressure due to laryngoscopy and tracheal intubation:a double-blind, randomized clinical trial. J Glaucoma. 2015; 24:372–6. DOI: 10.1097/IJG.0b013e31829f9bfe. PMID: 23835673.7. Sator-Katzenschlager S, Deusch E, Dolezal S, Michalek-Sauberer A, Grubmüller R, Heinze G, et al. Sevoflurane and propofol decrease intraocular pressure equally during non-ophthalmic surgery and recovery. Br J Anaesth. 2002; 89:764–6. DOI: 10.1093/bja/89.5.764. PMID: 12393777.8. Murphy DF. Anesthesia and intraocular pressure. Anesth Analg. 1985; 64:520–30. DOI: 10.1213/00000539-198505000-00013. PMID: 3158256.9. Klein BE, Klein R, Knudtson MD. Intraocular pressure and systemic blood pressure:longitudinal perspective:the Beaver Dam Eye Study. Br J Ophthalmol. 2005; 89:284–7. DOI: 10.1136/bjo.2004.048710. PMID: 15722304. PMCID: PMC1772559.10. Mitchell P, Lee AJ, Rochtchina E, Wang JJ. Open-angle glaucoma and systemic hypertension:the blue mountains eye study. J Glaucoma. 2004; 13:319–26. DOI: 10.1097/00061198-200408000-00010. PMID: 15226661.11. Xu L, Wang H, Wang Y, Jonas JB. Intraocular pressure correlated with arterial blood pressure:the beijing eye study. Am J Ophthalmol. 2007; 144:461–2. DOI: 10.1016/j.ajo.2007.05.013. PMID: 17765433.12. Gherghel D, Hosking SL, Orgül S. Autonomic nervous system, circadian rhythms, and primary open-angle glaucoma. Surv Ophthalmol. 2004; 49:491–508. DOI: 10.1016/S0039-6257(04)00110-9. PMID: 15325194.13. Czarnik T, Gawda R, Kolodziej W, Latka D, Sznajd-Weron K, Weron R. Associations between intracranial pressure, intraocular pressure and mean arterial pressure in patients with traumatic and non-traumatic brain injuries. Injury. 2009; 40:33–9. DOI: 10.1016/j.injury.2008.10.010. PMID: 19135194.14. Ding C, Wang P, Tian N. Effect of general anesthetics on IOP in elevated IOP mouse model. Exp Eye Res. 2011; 92:512–20. DOI: 10.1016/j.exer.2011.03.016. PMID: 21457709. PMCID: PMC3116023.15. Stambough JL, Dolan D, Werner R, Godfrey E. Ophthalmologic complications associated with prone positioning in spine surgery. J Am Acad Orthop Surg. 2007; 15:156–65. DOI: 10.5435/00124635-200703000-00005. PMID: 17341672.16. Pinkney TD, King AJ, Walter C, Wilson TR, Maxwell-Armstrong C, Acheson AG. Raised intraocular pressure (IOP) and perioperative visual loss in laparoscopic colorectal surgery:a catastrophe waiting to happen?A systematic review of evidence from other surgical specialities. Tech Coloproctol. 2012; 16:331–5. DOI: 10.1007/s10151-012-0879-5. PMID: 22936587.17. Nickels TJ, Manlapaz MR, Farag E. Perioperative visual loss after spine surgery. World J Orthop. 2014; 5:100–6. DOI: 10.5312/wjo.v5.i2.100. PMID: 24829872. PMCID: PMC4017302.18. Trivli A, Koliarakis I, Terzidou C, Goulielmos GN, Siganos CS, Spandidos DA, et al. Normal-tension glaucoma:pathogenesis and genetics. Exp Ther Med. 2019; 17:563–74. DOI: 10.3892/etm.2018.7011. PMID: 30651837. PMCID: PMC6307418.19. Razeghinejad MR, Lee D. Managing normal tension glaucoma by lowering the intraocular pressure. Surv Ophthalmol. 2019; 64:111–6. DOI: 10.1016/j.survophthal.2018.07.003. PMID: 30300624.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Optimal Dosage of Propofol for Prevention of Increase in IOP during Rapid Sequence Induction with Endotracheal Intubation
- The Effects of Remifentanil on Hemodynamic Changes in Endotracheal Intubation during Rapid Sequence Induction using Thiopental-succinylcholine or Propofol-succinylcholine
- The Effect on Inhibition of Raising Intraocular Pressure during Endotracheal Intubation in Man
- Comparison of Intubation Following Propofol-Fentanyl with Intubation Following Succinylcholine-Thiopental Sodium
- The Comparison of Vecuronium with Succinylcholine for Endotracheal Intubation