J Cerebrovasc Endovasc Neurosurg.
2019 Mar;21(1):11-17. 10.7461/jcen.2019.21.1.11.
A Meta-analysis for Evaluating Efficacy of Neuroendoscopic Surgery versus Craniotomy for Supratentorial Hypertensive Intracerebral Hemorrhage
- Affiliations
-
- 1Department of Neurosurgery, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, South Korea. yzkim@skku.edu
- KMID: 2465010
- DOI: http://doi.org/10.7461/jcen.2019.21.1.11
Abstract
OBJECTIVE
Hypertensive intracerebral hemorrhage is a potentially life-threatening neurological deficit with the highest morbidity and mortality. In recent years, neuroendoscopy has been used to treat intracerebral hemorrhages (ICHs). However, the choice of neuroendoscopic surgery or craniotomy for patients with ICHs is controversial. The objective of this meta-analysis was to assess the efficacy of neuroendoscopic surgery compared to craniotomy in patients with supratentorial hypertensive ICH.
MATERIALS AND METHODS
A systematic electronic search was performed using online electronic databases such as Pubmed, Embase, and Cochrane library updated on December 2017. The meta-analysis was performed by only including studies designed as randomized controlled trials.
RESULTS
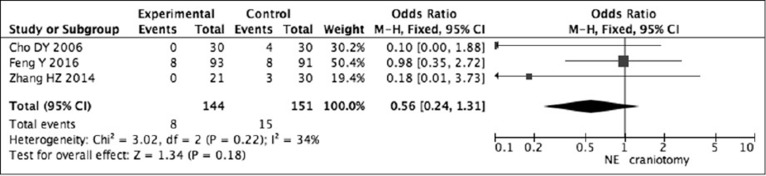
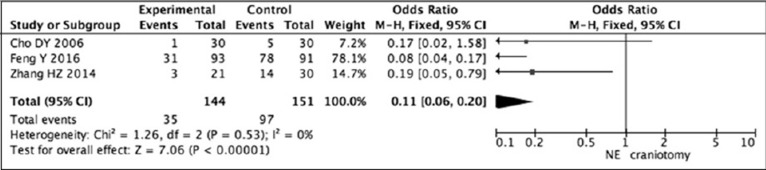
Three randomized controlled trials met our inclusion criteria. Pooled analysis of death showed that neuroendoscopic surgery decreased the rate of death compared to craniotomy (RR=0.58, 95% CI: 0.26-1.29; P=0.18). Pooled results of complications showed that neuroendoscopic surgery tended to have fewer complications than craniotomy had (RR=0.37, 95% CI: 0.28-0.49; P < 0.0001).
CONCLUSION
Although the presenting analyses suggest that neuroendoscopic surgery should have fewer complications than craniotomy dose, it had no superior advantage in morbidity rate definitely. Therefore, it may be necessary for the neurosurgeons to select best optimal patients for individual treatment.
Keyword
MeSH Terms
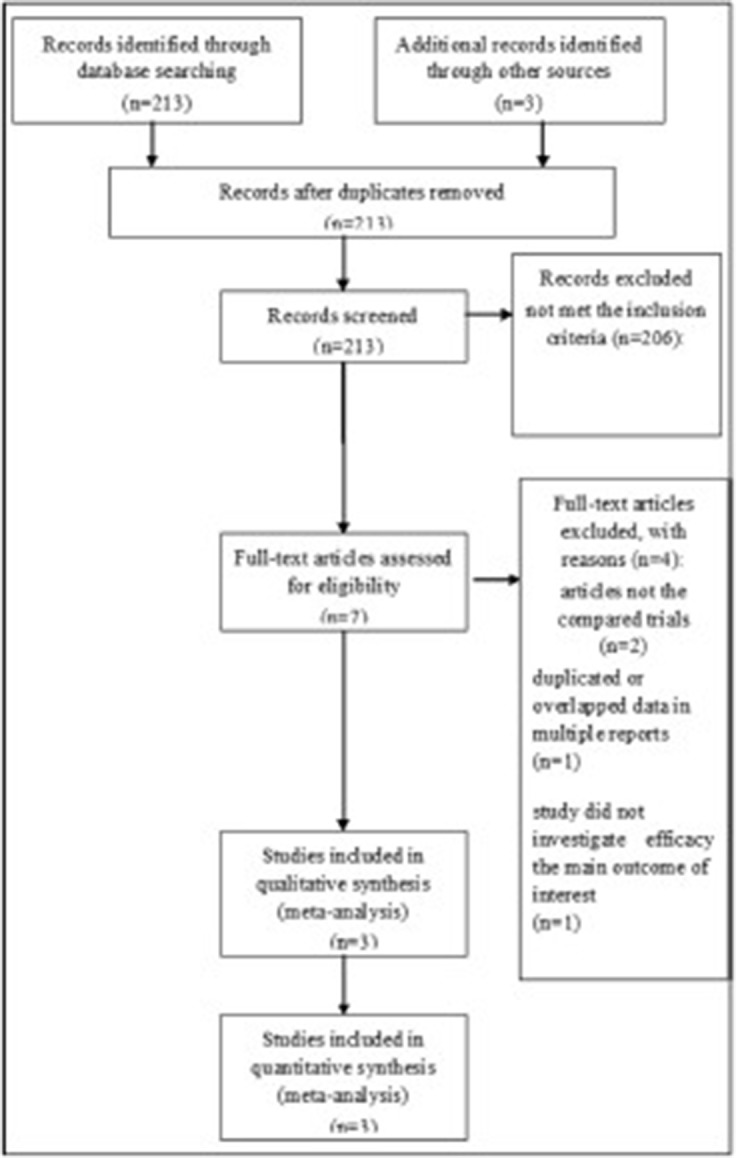
Figure
Cited by 1 articles
-
Surgical strategy for patients with supratentorial spontaneous intracerebral hemorrhage: minimally invasive surgery and conventional surgery
Je Hun Jang, Won-Sang Cho, Noah Hong, Chang Hwan Pang, Sung Ho Lee, Hyun-Seung Kang, Jeong Eun Kim
J Cerebrovasc Endovasc Neurosurg. 2020;22(3):156-164. doi: 10.7461/jcen.2020.22.3.156.
Reference
-
1. Auer LM, Deinsberger W, Niederkorn K, Gell G, Kleinert R, Schneider G, et al. Endoscopic surgery versus medical treatment for spontaneous intracerebral hematoma: a randomized study. J Neurosurg. 1989; 4. 70(4):530–535. PMID: 2926492.
Article2. Batjer HH, Reisch JS, Allen BC, Plaizier LJ, Su CJ. Failure of surgery to improve outcome in hypertensive putaminal hemorrhage. A prospective randomized trial. Arch Neurol. 1990; 10. 47(10):1103–1106. PMID: 2222242.3. Bhattathiri PS, Gregson B, Prasad KS, Mendelow AD, Investigators S. Intraventricular hemorrhage and hydrocephalus after spontaneous intracerebral hemorrhage: results from the STICH trial. Acta Neurochir Suppl. 2006; 96:65–68. PMID: 16671427.
Article4. Bosel J, Zweckberger K, Hacke W. Haemorrhage and hemicraniectomy: refining surgery for stroke. Curr Opin Neurol. 2015; 2. 28(1):16–22. PMID: 25490194.5. Cho DY, Chen CC, Chang CS, Lee WY, Tso M. Endoscopic surgery for spontaneous basal ganglia hemorrhage: comparing endoscopic surgery, stereotactic aspiration, and craniotomy in noncomatose patients. Surg Neurol. 2006; 6. 65(6):547–555. PMID: 16720167.
Article6. Feng Y, He J, Liu B, Yang L, Wang Y. Endoscope-Assisted Keyhole Technique for Hypertensive Cerebral Hemorrhage in Elderly Patients: A Randomized Controlled Study in 184 Patients. Turk Neurosurg. 2016; 26(1):84–89. PMID: 26768873.7. Hemphill JC, 3rd , Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, et al. Guidelines for the Management of Spontaneous Intracerebral Hemorrhage: A Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke. 2015; 7. 46(7):2032–2060. PMID: 26022637.
Article8. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002; 6. 21(11):1539–1558. PMID: 12111919.
Article9. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 9. 327(7414):557–560. PMID: 12958120.
Article10. Lee JI, Nam DH, Kim JS, Hong SC, Shin HJ, Park K, et al. Stereotactic aspiration of intracerebral haematoma: significance of surgical timing and haematoma volume reduction. J Clin Neurosci. 2003; 7. 10(4):439–443. PMID: 12852882.
Article11. Li F, Chen QX. Risk factors for mental disorders in patients with hypertensive intracerebral hemorrhage following neurosurgical treatment. J Neurol Sci. 2014; 6. 341(1-2):128–132. PMID: 24814350.
Article12. Li Q, Yang CH, Xu JG, Li H, You C. Surgical treatment for large spontaneous basal ganglia hemorrhage: retrospective analysis of 253 cases. Br J Neurosurg. 2013; 10. 27(5):617–621. PMID: 23406426.
Article13. Li Y, Yang R, Li Z, Yang Y, Tian B, Zhang X, et al. Surgical Evacuation of Spontaneous Supratentorial Lobar Intracerebral Hemorrhage: Comparison of Safety and Efficacy of Stereotactic Aspiration, Endoscopic Surgery, and Craniotomy. World Neurosurg. 2017; 9. 105:332–340. PMID: 28578111.
Article14. Luo JB, Peng B, Quan W, Cao ZK, Xiao GC, Lu JP, et al. Therapeutic effects of aspiration with a directional soft tube and conservative treatment on mild hemorrhage in the basal ganglion]. Nan Fang Yi Ke Da Xue Xue Bao. 2008; 8. 28(8):1352–1353. PMID: 18753058.15. Mayer SA, Rincon F. Treatment of intracerebral haemorrhage. Lancet Neurol. 2005; 10. 4(10):662–672. PMID: 16168935.
Article16. Mendelow AD, Gregson BA, Fernandes HM, Murray GD, Teasdale GM, et al. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial intracerebral haematomas in the International Surgical Trial in Intracerebral Haemorrhage (STICH): a randomised trial. Lancet. 2005; Jan-Feb. 365(9457):387–397. PMID: 15680453.
Article17. Mendelow AD, Gregson BA, Rowan EN, Murray GD, Gholkar A, Mitchell PM, et al. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial lobar intracerebral haematomas (STICH II): a randomised trial. Lancet. 2013; 8. 382(9890):397–408. PMID: 23726393.
Article18. Nagasaka T, Tsugeno M, Ikeda H, Okamoto T, Inao S, Wakabayashi T. Early recovery and better evacuation rate in neuroendoscopic surgery for spontaneous intracerebral hemorrhage using a multifunctional cannula: preliminary study in comparison with craniotomy. J Stroke Cerebrovasc Dis. 2011; May-Jun. 20(3):208–213. PMID: 20621516.
Article19. Ohwaki K, Yano E, Nagashima H, Hirata M, Nakagomi T, Tamura A. Surgery for patients with severe supratentorial intracerebral hemorrhage. Neurocrit Care. 2006; 5(1):15–20. PMID: 16960289.
Article20. Prasad K, Browman G, Srivastava A, Menon G. Surgery in primary supratentorial intracerebral hematoma: a meta-analysis of randomized trials. Acta Neurol Scand. 1997; 2. 95(2):103–110. PMID: 9059730.
Article21. Teernstra OP, Evers SM, Lodder J, Leffers P, Franke CL, Blaauw G, et al. Stereotactic treatment of intracerebral hematoma by means of a plasminogen activator: a multicenter randomized controlled trial (SICHPA). Stroke. 2003; 4. 34(4):968–974. PMID: 12649510.22. van Asch CJ, Luitse MJ, Rinkel GJ, van der Tweel I, Algra A, Klijn CJ. Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol. 2010; 2. 9(2):167–176. PMID: 20056489.
Article23. Wang WH, Hung YC, Hsu SP, Lin CF, Chen HH, Shih YH, et al. Endoscopic hematoma evacuation in patients with spontaneous supratentorial intracerebral hemorrhage. J Chin Med Assoc. 2015; 78(2):101–107. PMID: 25467795.
Article24. Xi G, Wagner KR, Keep RF, Hua Y, de Courten-Myers GM, Broderick JP, et al. Role of blood clot formation on early edema development after experimental intracerebral hemorrhage. Stroke. 1998; 12. 29(12):2580–2586. PMID: 9836771.
Article25. Xu X, Chen X, Li F, Zheng X, Wang Q, Sun G, et al. Effectiveness of endoscopic surgery for supratentorial hypertensive intracerebral hemorrhage: a comparison with craniotomy. J Neurosurg. 2018; 2. 128(2):553–559. PMID: 28387618.
Article26. Yamashiro S, Hitoshi Y, Yoshida A, Kuratsu J. Effectiveness of Endoscopic Surgery for Comatose Patients with Large Supratentorial Intracerebral Hemorrhages. Neurol Med Chir (Tokyo). 2015; 55(11):819–823. PMID: 26369719.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Management of Spontaneous Intracerebral Hemorrhage: Medical Versus Surgical Therapy for Spontaneous Intracerebral Hemorrhage
- Surgical Management of the Hypertensive Intracerebral Hemorrhage
- Etiology and Pathogenesis of Hypertensive Intracerebral Hemorrhage
- Remote Intracerebral Hematoma after Supratentorial Graniotomy
- Continuous Free External Ventricular Drainage in Hypertensive Intracerebral Hemorrhage with Ventricular Rupture