Clin Endosc.
2019 Sep;52(5):479-485. 10.5946/ce.2018.163.
Diagnostic Ability of Convex-Arrayed Endoscopic Ultrasonography for Major Vascular Invasion in Pancreatic Cancer
- Affiliations
-
- 1Department of Gastroenterology and Hepatology, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Science, Okayama, Japan. matsumoto.k@okayama-u.ac.jp
- 2Department of Pathology, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Science, Okayama, Japan.
- KMID: 2464670
- DOI: http://doi.org/10.5946/ce.2018.163
Abstract
- BACKGROUND/AIMS
This study aimed to examine the diagnostic ability of endoscopic ultrasonography (EUS) for major vascular invasion in pancreatic cancer and to evaluate the relationship between EUS findings and pathological distance.
METHODS
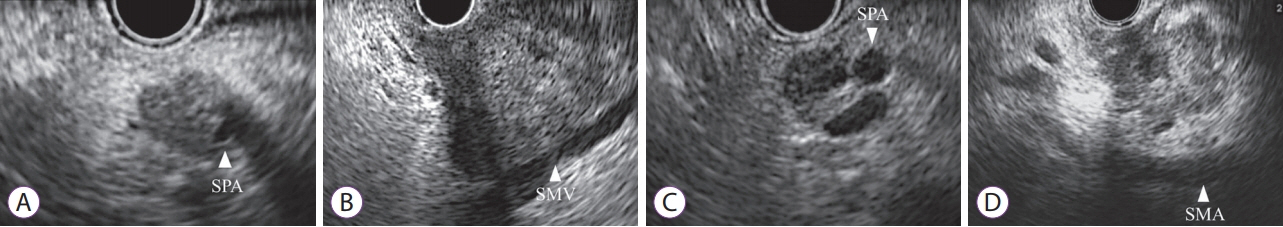
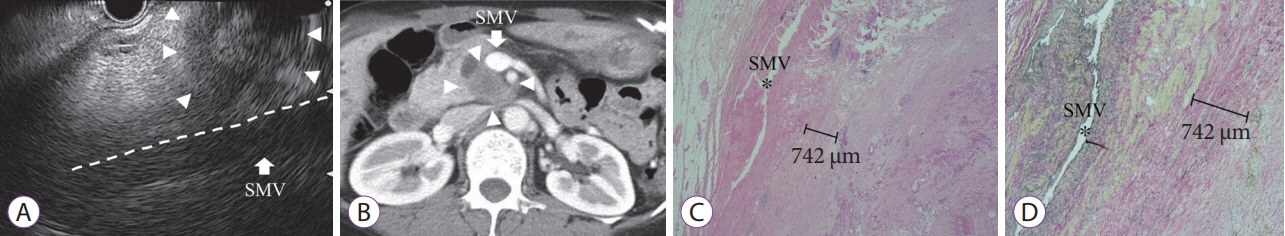
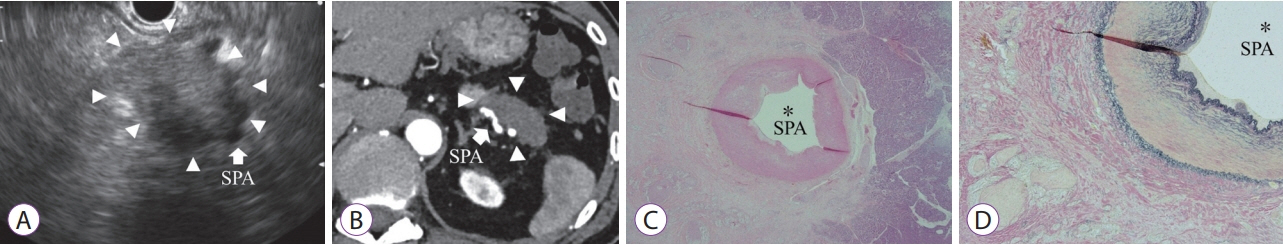
In total, 57 consecutive patients who underwent EUS for pancreatic cancer before surgery were retrospectively reviewed. EUS image findings were divided into four types according to the relationship between the tumor and major vessel (types 1 and 2: invasion, types 3 and 4: non-invasion). We also compared the EUS findings and pathologically measured distances between the tumors and evaluated vessels.
RESULTS
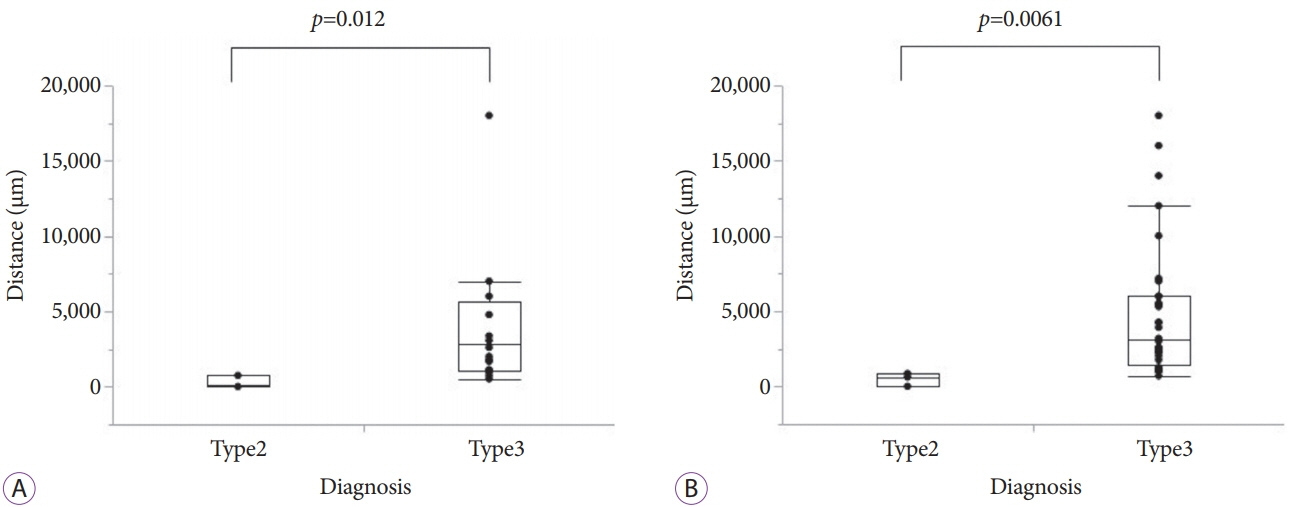
The sensitivity, specificity, and accuracy of EUS diagnosis for vascular invasion were 89%, 92%, and 91%, respectively, in the veins and 83%, 94%, and 93%, respectively, in the arteries. The pathologically evaluated distances of cases with type 2 EUS findings were significantly shorter than those of cases with type 3 EUS findings in both the major veins (median [interquartile range], 96 [0-742] µm vs. 2,833 [1,076-5,694] µm, p=0.012) and arteries (623 [0-854] µm vs. 3,097 [1,396-6,000] µm, p=0.0061). All cases with a distance of ≥1,000 µm between the tumors and main vessels were correctly diagnosed.
CONCLUSIONS
Tumors at a distance ≥1,000 µm from the main vessels were correctly diagnosed by EUS.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Endoscopic Ultrasonography for Vascular Invasion in Pancreatic Cancer
Seong-Hun Kim
Clin Endosc. 2019;52(5):397-398. doi: 10.5946/ce.2019.142.
Reference
-
1. Pancreatric Section; British Society of Gastroenterology; Association of Upper Gastrointestinal Surgeons of Great Britain and Ireland; Royal College of Pathologists; Special Interest Group for Gastro-Intestinal Radiology. Guidelines for the management of patients with pancreatic cancer periampullary and ampullary carcinomas. Gut. 2005; 54 Suppl 5:v1–v16.2. Warshaw AL, Fernández-del Castillo C. Pancreatic carcinoma. N Engl J Med. 1992; 326:455–465.
Article3. Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010; 60:277–300.
Article4. Wagner M, Redaelli C, Lietz M, Seiler CA, Friess H, Buchler MW. Curative resection is the single most important factor determining outcome in patients with pancreatic adenocarcinoma. Br J Surg. 2004; 91:586–594.
Article5. Ahmad NA, Kochman ML, Lewis JD, et al. Endosonography is superior to angiography in the preoperative assessment of vascular involvement among patients with pancreatic carcinoma. J Clin Gastroenterol. 2001; 32:54–58.
Article6. DeWitt J, Devereaux B, Chriswell M, et al. Comparison of endoscopic ultrasonography and multidetector computed tomography for detecting and staging pancreatic cancer. Ann Intern Med. 2004; 141:753–763.
Article7. Arslan A, Buanes T, Geitung JT. Pancreatic carcinoma: MR, MR angiography and dynamic helical CT in the evaluation of vascular invasion. Eur J Radiol. 2001; 38:151–159.
Article8. DiMagno EP, Reber HA, Tempero MA. AGA technical review on the epidemiology, diagnosis, and treatment of pancreatic ductal adenocarcinoma. American Gastroenterological Association. Gastroenterology. 1999; 117:1464–1484.9. Rösch T, Dittler HJ, Lorenz R, et al. [The endosonographic staging of pancreatic carcinoma]. Dtsch Med Wochenschr. 1992; 117:563–569.10. Megibow AJ, Zhou XH, Rotterdam H, et al. Pancreatic adenocarcinoma: CT versus MR imaging in the evaluation of resectability--report of the Radiology Diagnostic Oncology Group. Radiology. 1995; 195:327–332.
Article11. Saftoiu A, Vilmann P. Role of endoscopic ultrasound in the diagnosis and staging of pancreatic cancer. J Clin Ultrasound. 2009; 37:1–17.12. Michl P, Pauls S, Gress TM. Evidence-based diagnosis and staging of pancreatic cancer. Best Pract Res Clin Gastroenterol. 2006; 20:227–251.
Article13. Dewitt J, Devereaux BM, Lehman GA, Sherman S, Imperiale TF. Comparison of endoscopic ultrasound and computed tomography for the preoperative evaluation of pancreatic cancer: a systematic review. Clin Gastroenterol Hepatol. 2006; 4:717–725. quiz 664.
Article14. Nawaz H, Fan CY, Kloke J, et al. Performance characteristics of endoscopic ultrasound in the staging of pancreatic cancer: a meta-analysis. JOP. 2013; 14:484–497.15. Yang R, Lu M, Qian X, et al. Diagnostic accuracy of EUS and CT of vascular invasion in pancreatic cancer: a systematic review. J Cancer Res Clin Oncol. 2014; 140:2077–2086.
Article16. Puli SR, Singh S, Hagedorn CH, Reddy J, Olyaee M. Diagnostic accuracy of EUS for vascular invasion in pancreatic and periampullary cancers: a meta-analysis and systematic review. Gastrointest Endosc. 2007; 65:788–797.
Article17. Japan Pancreas Society. Classification of pancreatic carcinoma. 4th ed. Tokyo: Kanehara & Co., Ltd;2017.18. Nakata B, Nishino H, Ogawa Y, et al. Prognostic predictive value of endoscopic ultrasound findings for invasive ductal carcinomas of pancreatic head. Pancreas. 2005; 30:200–205.
Article19. Yeo CJ, Cameron JL, Lillemoe KD, et al. Pancreaticoduodenectomy for cancer of the head of the pancreas. 201 patients. Ann Surg. 1995; 221:721–731. discussion 731-733.
Article20. Tylén U, Arnesjö B. Resectability and prognosis of carcinoma of the pancreas evaluated by angiography. Scand J Gastroenterol. 1973; 8:691–697.
Article21. Geer RJ, Brennan MF. Prognostic indicators for survival after resection of pancreatic adenocarcinoma. Am J Surg. 1993; 165:68–72. discussion 72-73.
Article22. Cameron JL, Crist DW, Sitzmann JV, et al. Factors influencing survival after pancreaticoduodenectomy for pancreatic cancer. Am J Surg. 1991; 161:120–124. discussion 124-125.
Article23. Launois B, Franci J, Bardaxoglou E, et al. Total pancreatectomy for ductal adenocarcinoma of the pancreas with special reference to resection of the portal vein and multicentric cancer. World J Surg. 1993; 17:122–126. discussion 126-127.
Article24. ACR Committee on Drugs and Contrast Media, et al. ACR manual on contrast media version 10.3. [Internet]. Washington, D.C.: American College of Radiology;2017. [updated 2017; cited 2019 Jan 3]. Available from: https://www.acr.org/Quality-Safety/Resources/Contrast-Manual.25. Buchs NC, Chilcott M, Poletti PA, Buhler LH, Morel P. Vascular invasion in pancreatic cancer: imaging modalities, preoperative diagnosis and surgical management. World J Gastroenterol. 2010; 16:818–831.26. Buchs NC, Frossard JL, Rosset A, et al. Vascular invasion in pancreatic cancer: evaluation of endoscopic ultrasonography, computed tomography, ultrasonography, and angiography. Swiss Med Wkly. 2007; 137:286–291.27. Zhang Y, Huang J, Chen M, Jiao LR. Preoperative vascular evaluation with computed tomography and magnetic resonance imaging for pancreatic cancer: a meta-analysis. Pancreatology. 2012; 12:227–233.
Article28. Li JH, He R, Li YM, Cao G, Ma QY, Yang WB. Endoscopic ultrasonography for tumor node staging and vascular invasion in pancreatic cancer: a meta-analysis. Dig Surg. 2014; 31:297–305.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Capability of Radial- and Convex-Arrayed Echoendoscopes for Visualization of the Pancreatobiliary Junction
- Role of contrast-enhanced harmonic endoscopic ultrasonography (EUS) and EUS elastography in pancreatic lesions
- Forward viewing liner echoendoscopy for therapeutic interventions
- Factors Affecting the Diagnostic Accuracy of Endoscopic Ultrasonography for the Depth of Invasion in Early Gastric Cancer
- Diagnostic value of computed tomography in pancreatic cancer